Public Accounts Committee
Access to General Practice in Northern Ireland: Citizen Space Survey Results
Citizen GP Survey Report.pdf (1.13 mb)
Contents
Executive Summary - Access to GP Services Survey
2.1 Survey Design
2.2 Survey Fieldwork
2.3 Amendments to Questions During the Fieldwork Period
2.4 Adjusted Samples and Variation Between Full and Adjusted Data
2.5 Qualitative Responses and Thematic Analysis
2.6 Analysis of free-text comments
5. Analysis of Qualitative Responses
6. Discussion of Survey Findings
6.1 Experience of Accessing GP Services in the Past 12 Months
6.2 Access and Appointment barriers
6.3 Barriers to Booking Appointments
6.4 Inability to Secure an Appointment
6.4.1 Alternative Pathways for Help
6.5 Percieved Administrative Barriers
6.6 Appropriateness of Consultation
6.7 Impact on Patient Care and Outcomes
Executive Summary - Access to GP Services CITIZEN SPACE Survey
This survey provides a comprehensive picture of patient experiences accessing GP services in Northern Ireland, based on 15,237 responses gathered through a Citizen Space consultation to inform the Public Accounts Committee's inquiry into Access to General Practice in Northern Ireland. While not a representative sample of the entire population, the large volume of responses offers a powerful insight into recurring barriers, patient behaviours and the consequences of system pressures within primary care.
The findings reveal widespread difficulty accessing GP services, with 51% of respondents rating their overall experience as poor in the past 12 months and just 12% reporting a positive experience. Access barriers are dominated by difficulties getting through by telephone - the primary method used by 95% of respondents. Nine in ten reported challenges getting through on the phone, and two-thirds said it was not at all easy. Many described making dozens - and in some cases hundreds - of attempts to connect.
Limited appointment availability compounds these issues. Seven in ten reported a lack of face-to-face appointments, and around six in ten highlighted restricted access to both routine and urgent appointments. One-third were unable to secure a routine appointment at all, and 15% of urgent requests went unmet.
Consultation formats also emerged as a concern. Remote methods dominate (65% telephone vs. 35% in-person), with 45% of respondents feeling the format offered was not appropriate for their health needs. Only one in five telephone/video consultations fully resolved the issue, and nearly half required an in-person follow-up - suggesting inefficiencies in initial triage and reduced continuity of care.
The consequences of access barriers are significant. Almost three-quarters of respondents (74%) delayed seeking medical care due to difficulties accessing their GP, contributing to worsening symptoms, delayed diagnoses, use of emergency and out-of-hours services, and increased reliance on private healthcare. Many described emotional distress, loss of confidence in GP systems, and concerns about safety, particularly for chronic conditions, women's health and digital exclusion by some groups such as the elderly.
The survey results also highlight variation in how practices operate, with some offering more flexible or innovative systems - such as digital triage, voicemail callbacks or hybrid approaches - which patients described positively. These examples point to opportunities for improvement and potential models for wider adoption.
1. Background
In February 2025, the Public Accounts Committee opened its inquiry into Access to General Practice Services in Northern Ireland. Members heard evidence from the Department of Health, the Royal College of General Practitioners, the British Medical Association and the Patient Client Council.
Members were keen to ensure that the voice of the public, as service users, was included in the inquiry, therefore a decision was made to gather evidence from the public through the use of a Citizen Space survey in order to better understand the challenges faced when trying to access their GP.
2. Methodology
2.1 Survey Design
The survey was designed to gather public views on access to general practice services in Northern Ireland. Its structure and content were informed by the GP Patient Survey, an independent and methodologically robust instrument conducted by Ipsos on behalf of NHS England. The survey was adapted to reflect the specific context of Northern Ireland and the terms of the reference of the Committee's inquiry.
2.2 Survey Fieldwork
The survey was conducted online and open to the public between 28 February 2025 and 27 March 2025. A total of 15,237 responses were received. A paper format was also available on request.
Figure 1: No of responses received
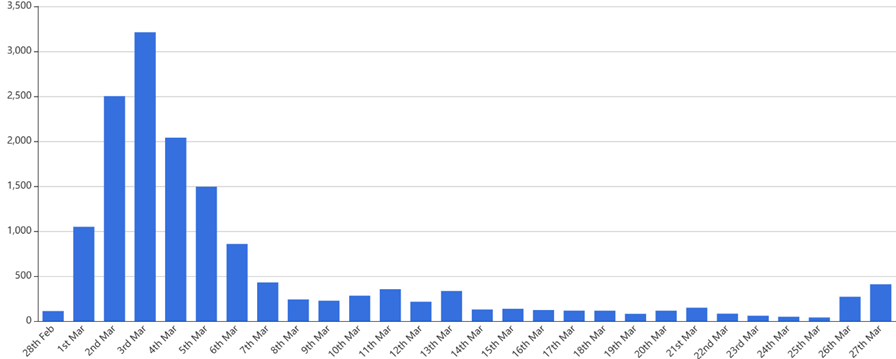
Number of responses received by date
2.3 Amendments to Questions During the Fieldwork Period
On 3 March 2025, following respondent feedback, the survey was temporarily taken offline to improve clarity and inclusivity of questions 7, 11, 12 and 20. Responses prior to that were excluded from certain analysis to maintain validity. These amendments ensured that all relevant response options were available to respondents from that date onwards. A summary of the changes made is provided below:
|
Box 1: Amendments to Survey Questions
Q7 - What are the main challenges you have faced when trying to access GP Services? (Tick all that apply). An 'I have not experienced any issues' option was added.
Q11 - How long did you have to wait for your most routine GP appointment?
Q12 - How long did you have to wait for your most urgent GP appointment? An option for 4-7 days was added to the response options available.
Q20 - What did you do if you were unable to get a suitable appointment? A 'Does not apply' option was added. |
2.4 Adjusted Samples and Variation Between Full and Adjusted Data
To address the amendments made to the survey on 3 March 2025 (notably Q7 and Q20), results were analysed using both the full sample of 15,237 respondents and an adjusted sample excluding responses received before the amendments (10,817 responses). Across most questions, there was minimal variation between full and adjusted samples, with percentage differences generally within 1-2 percentage points. This suggests that the amendments did not substantially alter the overall patterns of responses, though the adjusted sample provides a more accurate reflection of experiences for the updated questions.
2.5 Reporting of results
For reporting purposes, the figures provided in the analysis are taken from the adjusted sample.
Results have been rounded to remove decimal points, where 0%* is indicated, this is not reflective of zero respondents in that category, but that the result was rounded to 0%.
2.6 Qualitative Responses and Thematic Analysis
Free-text fields were added to allow respondents to describe experiences not fully captured by the listed response categories. Specifically:
- Question 7 invited respondents to describe any additional challenges they may have identified in accessing GP services.
- Question 9 invited respondents to provide further information regarding how they book appointments with their practice.
- Question 14 invited respondents to provide comments on the type of consultation offered for their last GP appointment.
- Question 19 invited respondents to describe any impact a delay in accessing GP services may have had on their health.
- Question 22 provided an open-ended opportunity for respondents to share any additional comments on access to GP services.
2.7 Analysis of free-text comments
Respondents were able to submit comments across multiple questions. As a result, the number of free-text responses represents the volume of feedback provided, not the number of respondents. Some themes therefore appear multiple times where respondents raised similar issues in different parts of the survey.
Free-text responses were analysed thematically to identify recurring patterns and key issues. These findings should be interpreted as qualitative evidence that provides insight into the nature and frequency of concerns, supplementing the quantitative survey results.
A tailored coding framework was developed for Question 22, which received the largest volume of free-text responses (over 10,000) and acted as a catch-all question. Given the richness of this dataset, comments were analysed both qualitatively and quantitatively to ensure that the breadth and significance of patient issues raised were fully captured.
2.8 Limitations
This was a survey on the views of those who wished to participate and while every effort was made to ensure that as many respondents as possible had the opportunity to respond, it cannot be considered as a representative sample of the general public or of any specific group.
3. Profile of respondents
The survey was open to Northern Ireland residents aged 18 and over. Responses were received from across all Health and Social Care Trust areas and a wide age range, with the largest group aged 35-54.
The following section sets out the demographic profile and geographical distribution of respondents.
The age demographics are broken down in the table below;
|
Age Bracket |
Whole Sample |
Adjusted Sample |
|
18-24 |
2% |
2% |
|
25-34 |
11% |
10% |
|
35-54 |
46% |
44% |
|
55-64 |
23% |
24% |
|
65 or over |
18% |
20% |
|
Not answered |
0%* |
0%* |
Respondents were also asked to indicate which Health and Social Care Trust (HSCT) they were located in to assist in identifying any differences in responses across trust areas.
|
Trust Area |
Whole Sample |
Adjusted Sample |
|
Belfast HSCT |
16% |
17% |
|
Northern HSCT |
29% |
28% |
|
South Eastern HSCT |
25% |
26% |
|
Southern HSCT |
23% |
21% |
|
Western HSCT |
11% |
13% |
|
Not answered |
0%* |
0%* |
4. Survey Data
This section contains all quantitative data tables from the survey, including both full and adjusted samples. Tables are presented exactly as reported in the Citizen Space dataset for transparency as follows:
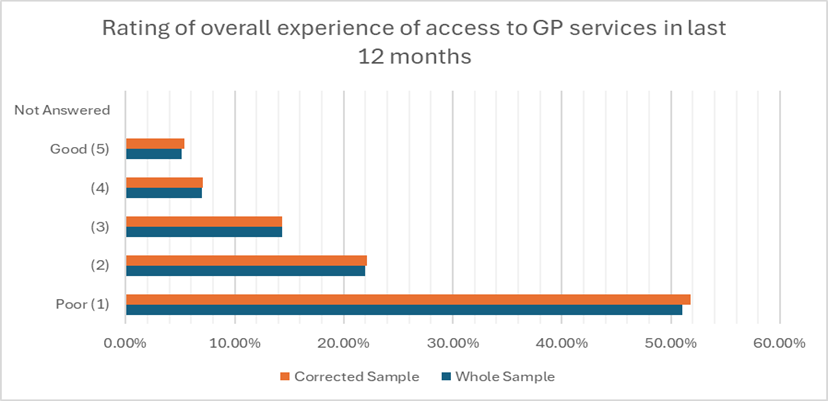
Q6 - On a scale of 1 to 5 how would you rate your overall experience on accessing GP services in the past 12 months? (1 poor - 5 excellent)
|
Rating |
All Responses |
Adjusted Sample |
||
|
1 - Poor |
7865 |
52% |
5524 |
51% |
|
2 |
3340 |
22% |
2391 |
22% |
|
3 |
2185 |
14% |
1554 |
14% |
|
4 |
1060 |
7% |
764 |
7% |
|
5 - Excellent |
786 |
5% |
583 |
5% |
|
Not Answered |
1 |
0%* |
1 |
0%* |
Q7 - What are the main challenges you have faced when trying to access GP Services? (Tick all that apply)
|
Option |
All Responses |
Adjusted Sample |
||
|
Difficulty getting through on the phone |
13870 |
91% |
9768 |
90% |
|
Lack of face to face appointments |
10724 |
70% |
7528 |
70% |
|
Limited availability of same day / urgent appointments |
9772 |
64% |
6816 |
63% |
|
Limited availability of routine appointments |
9307 |
61% |
6479 |
60% |
|
Long wait times for an appointment |
7145 |
47% |
5103 |
47% |
|
Issues with online booking systems |
2342 |
15% |
1615 |
15% |
|
A disability or health condition |
1103 |
7% |
797 |
7% |
|
Difficulties using computers, smartphones or the internet |
653 |
4% |
471 |
4% |
|
I have not experienced any challenges |
491 |
3% |
491 |
5% |
|
English is not your first language |
34 |
0%* |
22 |
0%* |
|
Not answered |
1 |
0%* |
1 |
0%* |
Other Category
There were 1,078 responses submitted under the 'Other' category. These comments reflected the themes highlighted in the Patient Insights box, including difficulties securing appointments, variation in digital triage approaches, and patients seeking alternative care pathways where GP appointments could not be secured.
Q8 - When did you last try to make a GP appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
In the last 3 months |
10728 |
70% |
7556 |
70% |
|
Between 3 and 6 months |
2432 |
16% |
1735 |
16% |
|
Between 6 and 12 months |
1336 |
9% |
979 |
9% |
|
More than 12 months |
578 |
4% |
433 |
4% |
|
Don't know |
162 |
1% |
113 |
1% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q9 - How do you usually book an appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
Phone |
14450 |
95% |
10233 |
95% |
|
Online |
317 |
2% |
218 |
2% |
|
In person |
469 |
3% |
365 |
3% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Other category
There were 957 responses submitted under the 'Other' category. The comments echoed the wider themes summarised in the Patient Insights box, particularly barriers to booking appointments; challenges for patients with work, caring or mobility needs; and perceived administrative barriers to accessing care.
Q10 - Generally, how easy is it to get through to someone at your GP practice on the phone?
|
Option |
All Responses |
Adjusted Sample |
||
|
Very easy |
340 |
2% |
250 |
2% |
|
Fairly easy |
1527 |
10% |
1107 |
10% |
|
Not easy |
3142 |
21% |
2254 |
21% |
|
Not at all easy |
10204 |
67% |
7187 |
66% |
|
Haven't tried |
23 |
0%* |
18 |
0%* |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q11 - How long did you have to wait for your most routine GP appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
Same day |
1325 |
9% |
901 |
8% |
|
1-3 days |
1825 |
12% |
1203 |
11% |
|
4-7 days |
1179 |
8% |
1179 |
11% |
|
More than a week |
2192 |
14% |
1402 |
13% |
|
More than 2 weeks |
2574 |
17% |
1795 |
17% |
|
I did not get an appointment |
5422 |
36% |
3617 |
33% |
|
I did not require an appointment |
719 |
5% |
719 |
7% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q12 - How long did you have to wait for your most urgent GP appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
Same day |
5049 |
33% |
3396 |
31% |
|
1-3 days |
3488 |
23% |
2316 |
21% |
|
4-7 days |
769 |
5% |
769 |
7% |
|
More than a week |
872 |
6% |
461 |
4% |
|
More than 2 weeks |
520 |
3% |
332 |
3% |
|
I did not get an appointment |
2598 |
17% |
1602 |
15% |
|
I did not require an appointment |
1940 |
13% |
1940 |
18% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q13 - Before you tried to get your most recent appointment, did you do any of the following? (Please tick all that apply)
|
Option |
All Responses |
Adjusted Sample |
||
|
I tried to treat myself or the person I was making the appointment for |
8994 |
59% |
6273 |
58% |
|
I looked for information online |
8507 |
56% |
5847 |
54% |
|
I spoke to a Pharmacist |
6569 |
43% |
4582 |
42% |
|
Tried to get information or advice from elsewhere |
5295 |
35% |
3686 |
34% |
|
Asked for advice from a family member or friend |
4839 |
32% |
3320 |
31% |
|
I did not try to get information or advice |
1575 |
10% |
1195 |
11% |
|
Went to or contacted another NH Service |
1410 |
9% |
979 |
9% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q14 - What type of consultation was offered for your last GP appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
Telephone |
10004 |
66% |
7022 |
65% |
|
Face to face |
5192 |
35% |
3765 |
35% |
|
Video call |
24 |
0%* |
17 |
0%* |
|
Home Visit |
16 |
0%* |
12 |
0%* |
|
Not answered |
1 |
0%* |
1 |
0%* |
Free text responses
There were 1,527 responses submitted under the 'Other' category. These comments were consistent with the themes outlined in the Patient Insights box, including difficulties with advance booking, challenges for those requiring follow-up appointments or long-term condition management, and concerns regarding call-back systems.
Q15 - Did you feel the type of consultation you were offered was appropriate for your health concern?
|
Option |
All Responses |
Adjusted Sample |
||
|
Yes |
6487 |
43% |
4685 |
43% |
|
No |
6984 |
46% |
4858 |
45% |
|
Not sure |
1765 |
12% |
1273 |
12% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q16 - If you had a telephone / video conference did you feel that your issue was fully addressed?
|
Option |
All Responses |
Adjusted Sample |
||
|
Yes |
3149 |
21% |
2245 |
21% |
|
No |
6545 |
43% |
4559 |
42% |
|
Not sure |
3158 |
21% |
2286 |
21% |
|
Not answered |
2385 |
16% |
1727 |
16% |
Q17 - Did you need a follow-up in person appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
Yes |
7385 |
48% |
5243 |
48% |
|
No |
7851 |
52% |
5573 |
52% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q18 - How satisfied were you with the appointment that was offered to you?
|
Rating |
All Responses |
Adjusted Sample |
||
|
Very satisfied |
2421 |
16% |
1770 |
16% |
|
Fairly satisfied |
3383 |
22% |
2435 |
23% |
|
Neither satisfied nor dissatisfied |
2870 |
19% |
2055 |
19% |
|
Fairly dissatisfied |
2265 |
15% |
1589 |
15% |
|
Very dissatisfied |
2312 |
15% |
1582 |
15% |
|
I was unable to get an appointment |
1985 |
13% |
1385 |
13% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q19 - Have you ever had to delay seeking medical help because of difficulties accessing GP Services?
|
Option |
All Responses |
Adjusted Sample |
||
|
Yes |
11515 |
76% |
8057 |
74% |
|
No |
3720 |
24% |
2758 |
26% |
|
Not answered |
2 |
0%* |
2 |
0%* |
Free text responses
There were 9,625 responses submitted under the 'Other' category. These responses aligned closely with the broader themes summarised in the Patient Insights box, highlighting the main challenges in accessing routine and long-term care, delays in test results and referrals, impacts on health and employment, and increased use of urgent or private services where access barrier were encountered.
Q20 - What did you do if you were unable to get a suitable appointment?
|
Option |
All Responses |
Adjusted Sample |
||
|
Try to contact my GP another time |
3373 |
22% |
2263 |
21% |
|
Went to A&E |
1898 |
13% |
1306 |
12% |
|
Contact Out of Hours GP |
1751 |
11% |
1178 |
11% |
|
Contacted a private healthcare provider |
1741 |
11% |
1186 |
11% |
|
Looked for information online |
1626 |
11% |
1134 |
10% |
|
Does not apply |
1509 |
10% |
1509 |
14% |
|
Spoke to a Pharmacist |
1121 |
7% |
768 |
7% |
|
Did Nothing |
1054 |
7% |
1054 |
10% |
|
Spoke to a friend or family member for advice |
598 |
4% |
417 |
4% |
|
Not answered |
566 |
4% |
2 |
0%* |
Q21 - As far as you know, which of the following services does your GP offer?
|
Option |
All Responses |
Adjusted Sample |
||
|
Booking appointments online |
2154 |
14% |
1562 |
14% |
|
Ordering repeat prescriptions online |
10396 |
68% |
7372 |
68% |
|
None of these |
2910 |
19% |
2048 |
19% |
|
Don't know |
1848 |
12% |
1336 |
12% |
|
Not answered |
1 |
0%* |
1 |
0%* |
Q22 - Any other comments
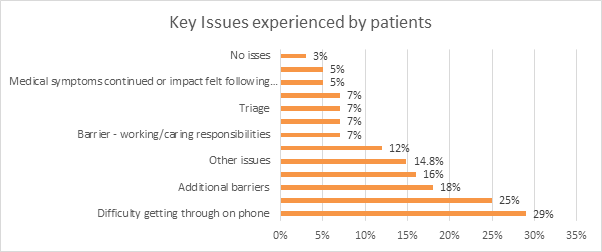
There were 10,660 comments submitted under the 'Any Other Comments' question. The accompanying chart provides a quantitative overview of the key themes identified. These comments reflected the wider themes summarised in the Patient Insights box, particularly in relation to challenges securing timely appointments, increased use of urgent and private services, difficulties accessing follow-up care, tests and chronic condition reviews, and reported impacts on health, wellbeing and confidence in primary care access.
These issues closely align with themes highlighted in earlier survey questions and are explored further in the Survey Findings section.
The chart overleaf provides a quantitative summary of the issues most commonly raised in the free-text responses to this question. It illustrates the proportion of respondents who highlighted specific access and service issues. While individual themes varied in frequency, the dominant issue was the difficulties and barriers in securing timely GP appointments and the related health impacts on care. A small proportion of respondents (3 per cent) reported no issues.
Figure 2: Key issues experienced by patients
Note: Free-text responses are voluntary and typically reflect the experiences of individuals who choose to provide additional feedback. These comments offer valuable insight but should be interpreted as qualitative evidence rather than a statistically representative dataset. Figure 3 Additional Low-Frequency Issues
Figure 3: Other issues Further issues raised in smaller numbers, offering additional insight beyond the main coded themes.
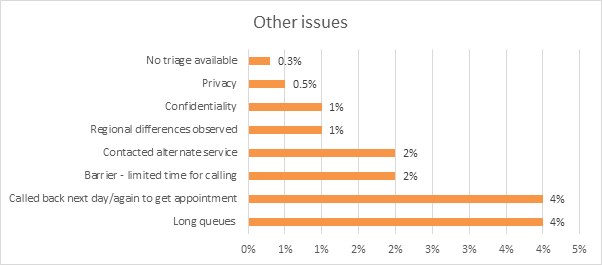
Other issues: A further 14 per cent of respondents raised issues that did not fall within the main coded themes but nonetheless provide valuable context. These included comments relating to privacy and confidentiality, variation between practices, queueing to access services, and restricted booking windows.
5. Analysis of Qualitative responses
While the quantitative data captures clear patterns of patient experience, respondents also submitted over 23,000 free-text comments. These provide rich insight into the lived experience behind the statistics.
Across Questions 7, 9, 14, 19 and 22, over 23,000free-text comments were submitted relating to experiences accessing GP services. While each question focused on a different part of the patient experience, responses were very consistent. Alongside examples of good practice and innovative digital access, many respondents described persistent challenges securing appointments, continuity of care and timely follow-up, with consequences for health and confidence in primary care systems.
A consolidated summary of these qualitative insights is set out in the Patient Insights box overleaf.
Box 2: Key Patient Insights from Free-Text ResponsesBooking and Access Challenges
These issues particularly affected those with caring responsibilities, employment commitments, disabilities, mobility limitations or unreliable mobile signal.
Triage and Communication
Positive feedback was provided where digital triage and tools such as text messaging and photo uploads were available.
Continuity and Follow-Up Care
Alternative Pathways and Escalation
A small number reported disengaging from seeking care.
Impact on Health and Emotional Wellbeing
Impact on Daily Life and Functioning
|
6. Discussion of Survey Findings
The qualitative and quantitative evidence together offer a coherent picture of the access challenges faced by patients. This section synthesises these findings, exploring their implications for appointment availability, consultation formats, administrative processes, and patient outcomes.
6.1 Experience of accessing GP Services in the past 12 months
This section explores overall patient sentiment regarding GP access over the past 12 months, drawing together ratings data and illustrative examples to highlight the broader context of dissatisfaction.
The survey data reveals significant challenges in accessing GP services across Northern Ireland. Over half of respondents (51%) rated their experience as poor (1 out of 5), while only 12% reported a positive rating (4 or 5 out of 5). The volume and consistency of responses suggest deep and widespread dissatisfaction with current access arrangements.
Table 1: Rating of experiences accessing GP Services
Although many respondents expressed confidence in the clinical advice once they were seen, their difficulty in securing timely access was overshadowed by their satisfaction with the care received. Several patients described a sense of frustration, anxiety and helplessness due to delays and repeated attempts to reach their GP.
Patients frequently contrasted the quality of the clinical care with the structural barriers surrounding access. Many described long periods of uncertainty while trying to obtain appointments, often requiring multiple days of effort or repeated attempts. Respondents reported being unable to reach reception staff, facing abrupt end of booking windows, or finding that all appointments for the day had been filled within minutes. These combined factors contribute to a perception among respondents that GP services have become increasingly difficult to access, even for non-urgent but clinically important issues.
|
You are made to feel like your medical problems unless life or death are unimportant. You feel like you MUST be gravely ill to see a GP and getting appointments for routine problems is really difficult |
|
My GP is excellent and staff are incredible, polite and knowledgeable. Unfortunately the system is broken and I fear it will only get worse. Not being able to get an appointment and being sent to A&E as an alternative for non-emergent appointment only adds to the pressure on different sector. |
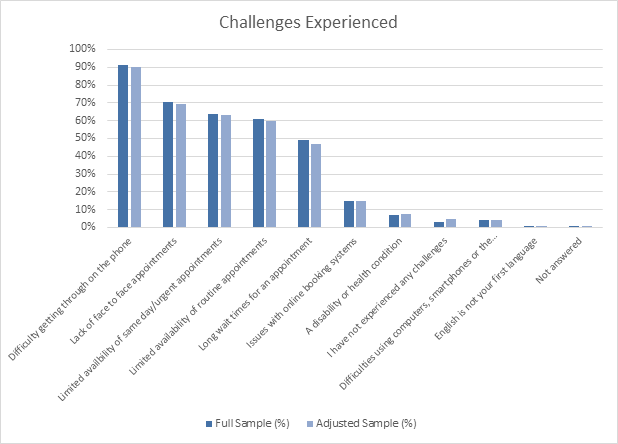
6.2 Access and appointment barriers
Respondents identified multiple structural obstacles to accessing appointments which are explored below.
Responses consistently pointed to substantial structural barriers that prevent patients from obtaining GP appointments in a timely and predictable manner. While individual experiences vary by practice, several recurring access problems emerged across the survey, indicating systemic issues rather than isolated incidents.
Table 2: Difficulties identified
6.3 Barriers to booking appointments
Booking systems, especially reliance on telephone access, emerged as a consistent source of frustration. This section examines specific barriers such as limited booking windows, call congestion and digital exclusion.
The most prominent barrier reported was difficulty getting through on the phone. Although 95% of respondents typically used the telephone to book appointments, 90% experienced challenges in reaching their practice, with more than two-thirds stating it was "not at all easy." Many described long queues, repeated redialling, and calls that cut off before being answered-particularly during early-morning booking windows when demand peaks. Some reported making over 100 calls before successfully speaking with reception staff, with one individual recording more than 600 attempts.
|
Once I get through the care is excellent. However, its time consuming & inconvenient to redial to get an appointment & if you miss the slots that day you have to try again the following with no guarantee of getting through again. |
Strict booking windows were a key source of frustration. Many practices required patients to call at opening time for same-day appointments, with slots allocated on a first-come, first-served basis and filled within minutes. Those juggling work or caring responsibilities often found this model unworkable, leading to repeated delays in obtaining care. Several respondents noted that these systems also carried financial and emotional costs, citing exhaustion and significant phone credit spent without success-for example, two individuals reported spending £17 and £22 respectively without securing an appointment.
|
Rang over 20 times and no one answers. Phone bill I got showed it cost me over £10 and got nowhere. All I hear is your call is important to us. |
Booking processes were often described as unpredictable, stressful, and heavily dependent on timing, with limited flexibility built into practice systems. Some respondents felt discouraged from seeking help unless their issue was urgent, contributing to delayed presentation and worsening symptoms. Concerns were also raised about practices that offered only same-day telephone triage with no facility to pre-book routine appointments, creating difficulties for those requiring regular reviews, follow-up care, or management of chronic conditions.
Call congestion was compounded by limited alternatives. While some practices had previously offered online booking, many respondents explained that these systems were withdrawn during or after the COVID-19 pandemic and have not been reinstated. Only 14% reported access to any online booking facility, and in several cases these were restricted to repeat prescriptions or administrative requests rather than appointments.
|
I feel the option to request repeat prescriptions or respond to appointment requests online would help patients. |
Awareness of available digital tools was also low: 19% said their practice did not offer any online facility, and a further 12% were unsure what was available. A small number (4%) experienced digital-exclusion issues such as difficulty using devices or the internet, while 7% reported barriers related to disability or health conditions.
|
I wish you could book appointments online. I have a disability which makes phonecalls almost impossible. Therefore my partner has to ring for me. This reduces my independence, privacy and dignity. In this day and age healthcare should be more accessible. Otherwise my GP surgery is generally excellent and the doctors work very hard. I wish they weren't under so much pressure. |
|
My GP surgery sends me text messages about vaccines. You are supposed to click a link to book. I don't have a smart phone so this is useless to me. |
Respondents described mixed experiences with newer digital or call-management systems. Positive examples included call-back services, voicemail-based triage, and online forms that allowed patients to describe symptoms in advance. However, others felt that these systems reduced personal contact and limited the information available to clinicians, potentially affecting diagnosis and treatment. While digital innovation offers clear potential to reduce telephone bottlenecks, respondents cautioned that online-first models may deepen digital exclusion unless supported by accessible alternatives.
While many respondents described frustration with the processes involved in booking appointments-including long telephone queues, restricted online systems, and inconsistent triage arrangements-these procedural barriers often translated directly into an inability to secure an appointment at all. For some, the challenge was not just how to book, but whether any appointments were available by the time they got through.
6.4 Inability to Secure an appointment
The inability to secure either routine or urgent appointments represents one of the most prominent issues highlighted by respondents. This is explored further below.
Limited appointment availability was one of the most commonly cited barriers to accessing GP services, compounding the problem of access. Around six in ten respondents reported difficulties securing same-day, urgent, or routine appointments. Many described situations where, after finally getting through to their practice, they were told that all slots for the day were already taken and advised to try again later or the following day.
|
So difficult to get through on phone to surgery. Line opens at 8.30 at which time I am in work. You have to continuously re-dial to get through. My last attempt took 98 re-dials until I actually got into the queue to await phone being answered. There are many times I have had to give up trying as I am in work and cannot take time to continue trying to get through. By 9 am all appointments are gone. |
Some practices were reported to offer only same-day appointments, with no facility to pre-book for routine consultations. This created difficulties for managing chronic conditions, medication reviews, or recurring health issues, as patients were forced to compete each morning for limited slots regardless of clinical need.
The qualitative feedback highlighted widespread frustration with telephone-only booking systems, often restricted to early morning calls. Respondents described long call queues, limited appointment availability, and difficulty obtaining a suitable time. For some, this system led to taking time off work, or delaying and sometimes avoiding care altogether.
|
You cannot access appointments - you have to call every day at 8.30AM, which for most parents is impossible due to getting ready for school or school run times. |
A large number of respondents also felt inappropriately redirected to Out of Hours, Urgent Care, or A&E services due to the unavailability of GP appointments.
For routine care, one-third (33%) could not get an appointment at all, and nearly three in ten waited more than a week. While one in three urgent appointment requests were met on the same day, 15% were unable to secure one.
6.4.1 Alternative pathways for help
When patients were unable to secure a suitable appointment, most either tried again later (21%) or sought help elsewhere - including Accident and Emergency departments (12%), out-of-hours GP services (11%), or private healthcare (11%), often at significant personal cost.
|
I had to go private as I was so unwell I couldn't wait any longer to get an appointment it was a cost to me of almost £100 app and prescription and sick line money I could not afford. |
Patients were frequently redirected to Out-of-Hours, Urgent Care, or Accident and Emergency services, either following advice from their GP practice or as a consequence of being unable to obtain an appointment.
|
Very stressful as I made over 100 calls to finally get an answer to be told no appointment's would be available as there where no doctors and to phone again the next day this happened for 8 consecutive days. Finally when I got to speak to a doctor they told me to go to A&E and get bloods done. On calling A&E they told me the GP should be dealing with this case. Finally got seen by an out of hours doctor. |
|
When I call and can't get an appointment they tell me to go to A&E which I don't feel is appropriate |
Some respondents reported feeling compelled to use alternative services inappropriately, or postponed seeking care to avoid adding pressure to other parts of the system.
More than half had sought information or advice before contacting their GP - most commonly online or through self-care - while over 40% consulted a pharmacist. Others sought support from NHS helplines, friends, or family members. Only 10% of respondents had not sought any information or advice before making contact with their GP.
|
I hesitated for a few weeks until the problem got worse - before I called the GP I looked it up online, tried to self medicate, then I did speak to a pharmacist and a GP OoO, and finally went to my GP who gave me the right prescription |
|
After I self treated myself, I attended pharmacy and spoke with pharmacist, who advised I seek gp urgent appointment. This is where the system fail me. I was unable to get a gp appointment as admin would not permit same day appointment. I had to resort to visiting A&E to get confirmed diagnosis and prescription. |
The evidence illustrates that limited appointment availability not only delays access to primary care but also shifts demand onto other parts of the health system. Many patients reported feeling caught in a cycle of repeated attempts, redirection, or self-management - often without clinical support. These experiences, coupled with frustration at the booking process itself, contributed to a growing perception among respondents that administrative processes and frontline staff were acting as barriers rather than facilitators of care, a theme explored further in the next section.
6.5 Percieved administrative barriers
Alongside ongoing difficulties with telephone access and appointment availability, many respondents described additional administrative obstacles that shaped their overall experience of accessing GP services. These barriers often contributed to delays, confusion, and frustration, and created a perception that administrative systems - rather than clinical need - determined whether a patient could obtain care. For example, a considerable number of respondents felt that both reception staff and pre-recorded telephone messages appeared to discourage patients from contacting their GP. Some also noted that automated messages continued to include outdated information relating to the Covid-19 pandemic.
|
Having to listen to a very long message on the phone saying that they are experiencing unprecedented demand, that they will not tolerate any abuse (understandable), and that I am to contact my MLA if I am unhappy with the service |
|
My GP practice regularly updates their social media pages with the message that they are only dealing with urgent care and not to be contacting the surgery |
Many respondents raised concerns regarding triage and gatekeeping by reception staff. A key concern centred on the role of reception staff in the triage process. Whilst may respondents recognised that receptionists are essential in managing high demand, others expressed discomfort with having to share sensitive information with non-clinical staff and uncertainty over how decisions were made about urgency and suitability for appointments.
|
Receptionists ask too much personal information, receptionists decide if you can request a call back from GP, receptionists give medical advice despite not being medically trained |
|
You shouldn't have to go into detail with the receptionist about your illness. I understand they have to triage you but on two separate occasions they tried to diagnose me and gave me wrong information rather than giving me an appointment |
|
Receptionist decided what treatment I needed, rather than giving me a GP appointment. I got wrong medication and condition got worse causing a small infection to turn to sepsis and requiring hospital visit and months of various treatments |
Many said the tone of recorded messages and staff interactions left them feeling unwelcome or dismissed. While many acknowledged the professionalism of reception staff, others reported less positive experiences. Many also reported feeling that the overall triage process lacked empathy.
|
It is utterly inappropriate to be having conversations with a receptionist about your condition and for them to have the power to decide how important your case is. The system of ringing over and over, often for an hour or more, is no system at all. The role of the GP today is questionable to say the least, and one is often forced to pursue an alternative for medical assistance. |
Overall, the evidence suggests that administrative systems and staff interactions play a crucial role in shaping patient perceptions of access and care. While many respondents acknowledged the pressures facing GP practices and the professionalism of administrative staff, others felt that the tone and structure of these interactions could undermine confidence and trust.
6.6 Appropriateness of consultation
With remote consultations now the dominant mode, this section assesses patient views on suitability, accuracy, and clinical effectiveness, alongside risks of misdiagnosis and the need for in-person follow-up.
In addition to difficulties securing appointments, many respondents questioned whether the type of consultation they received was appropriate for their clinical needs. The balance between remote and face-to-face appointments was a particular concern, with many feeling that the consultation method was determined more by practice systems than by the nature or complexity of their health problem.
Seven in ten (70%) reported a lack of face-to-face appointments, with the shift towards remote consultations a significant source of dissatisfaction. Nearly two-thirds (65%) of appointments were by telephone, compared to 35% held in person.
|
Being unable to see GP in person means I've avoided raising some health concerns as a phone appt is too impersonal and remote. With my mental health issues I need face to face at times. |
Almost half (45%) felt the consultation type was not appropriate for their health concern, and only one in five (21%) who had a telephone/video consultation felt their issue was fully addressed. Nearly half (48%) required a follow-up in-person appointment, raising questions about efficiency and patient outcomes.
|
The lack of seeing a doctor in person is really worrying. I was misdiagnosed several times, and I feel this wouldn't have happened if I was seen in person. I have been diagnosed with a health condition now from hospital appointments but never was face to face with a GP once. |
A number of respondents, including those living with disabilities or supporting elderly relatives with hearing difficulties, reported being unable to participate in telephone consultations.
|
I have difficulties with telephone conversations because of my hearing difficulties |
The concerns expressed about consultation formats and access arrangements were often linked to wider effects on diagnosis, treatment, and continuity of care. These themes are explored further in the following section, which examines the impact on patient care and outcomes.
6.7 Impact on Patient Care and Outcomes
This section highlights reported impacts on diagnosis, treatment, wellbeing and daily functioning.
Difficulties in accessing appropriate consultations and appointments had a tangible effect on patient care. Respondents frequently described delays that affected diagnosis, treatment, and ongoing management. Almost three-quarters (74%) reported postponing or avoiding seeking medical help because of access difficulties.
The consequences extended beyond inconvenience, influencing clinical outcomes, emotional wellbeing, and wider health-system pressures. Many patients reported worsening symptoms, prolonged illness, or deterioration of chronic conditions due to delayed care. Some conditions progressed to the point of requiring emergency intervention or hospital admission, and a small number reported delayed or missed diagnoses, including serious illnesses such as cancer.
|
I have a number of health concerns that need to have addressed by a doctor but because some of them are not urgent, I tend to not even try to get an appointment because it is so difficult. I normally end up waiting until something is urgent before I contact a doctor and then try and address a number of issues at once. This is very stressful. Having to redial over 200 times on occasion means I tend to leave things too long before seeking help. Meaning the problem is worse by the time I get to speak to someone |
6.7.1 Continuity and Ongoing Care
Respondents often highlighted a lack of continuity, rarely seeing the same GP or receiving follow-up such as explanation of test results or medication reviews. Accessing chronic-disease management services-for asthma, diabetes, or hypertension-was described as particularly challenging. Difficulties obtaining repeat prescriptions or arranging reviews sometimes resulted in interruptions to essential medication, with a few patients resorting to purchasing medicines online without clinical oversight.
|
It's impossible to get through, even for a repeat prescription automated line. This has resulted in my prescription being delayed. The type of medication I take has quick acting impact when doses are skipped. |
|
I've had a number of occasions where my medicine has been delayed as I couldn't speak to a GP. As a health care professional, I've have had to go out of my way to advocate for my health and also source alternative treatments meaning having to pay on occasion |
6.7.2 Access to care for Chronic Conditions
Access to care for long-term conditions such as asthma, diabetes, and hypertension was described as particularly challenging. Treatment rooms, practice nurses, and chronic disease management clinics were often difficult to access, and delays in arranging reviews or obtaining repeat prescriptions sometimes led to interruptions in essential medication. In isolated cases, patients reported purchasing medicines online, including antibiotics and hormone replacement therapy, without medical oversight.
|
I feel I have been neglected over the last 4/5 years, wasn't seen at the diabetic clinic for 3 years and the Dr's and nurses at the surgery don't want to know either |
|
Have access to GP based pharmacist who manages medications for certain conditions e.g diabetes which has been helpful. However other checks, routine blood checks HbA1c, asthma reviews are sometimes overdue due to other pressures |
6.7.3 Access to Specialist and Women's Health Services
Several respondents experienced problems obtaining referrals to specialist care, both within the NHS and privately, because they were unable to secure a GP appointment. Women reported delays in accessing contraception, smear tests, post-natal care, and hormone-replacement therapy, all of which had significant effects on health and wellbeing.
|
Difficulty is getting help for routine but important things like hrt, which effect everyday health. None of my GPS know enough about menopause to effectively help and a couple have just not been interested in helping, so I feel no further forward. I just feel there's no point in even asking for help anymore. |
6.7.4 Wider Impacts
The cumulative effect of these challenges took a toll on patients' daily lives and emotional health. Many described stress, frustration, and anxiety linked to delays in treatment or uncertainty about their condition. Some neglected their own health because they believed their issue was not "urgent enough" to warrant an appointment. Health deterioration often affected their ability to work, exercise, or manage everyday tasks, while administrative burdens such as medical paperwork added further strain.
|
It becomes very worrying, as there is both frustration and concern: frustration I can't get through to someone easily, and concern that what I'm experiencing may get worse. |
|
The delay in accessing a gp appointment delayed commencement of appropriate treatment and slowed down healing. This had a negative impact on my physical wellbeing as I was unwell for longer and mental wellbeing as i had increased anxiety about my condition. It also affected me financially as I more missed days at work due to my condition. |
Many respondents reported a loss of confidence in GP services, with some expressing a sense of being dismissed or undervalued. Overall, the evidence indicates that barriers to timely GP access have far-reaching effects - clinically, emotionally, and socially - highlighting the importance of ensuring care that is accessible, continuous, and well coordinated.
7. Regional variations
Survey responses were collected from individuals living across all Health and Social Care Trust areas in Northern Ireland (see Appendix 1). While each Trust includes a mix of rural, urban, and geographically diverse communities, the overall pattern of reported experience was strikingly consistent. Access barriers described throughout the survey - including difficulty with appointment booking, challenges with telephone access, limited availability of face-to-face consultations, and administrative hurdles - were evident across all Trust areas.
Quantitative analysis revealed no significant differences between Trust regions on key indicators such as ease of obtaining an appointment, satisfaction with consultation format, or difficulty contacting practices by phone. Across all geographic areas, respondents highlighted similar frustrations, suggesting that the access problems identified represent system-wide challenges rather than issues isolated to specific localities or individual practices.
Although free-text responses occasionally referenced local factors - such as rural travel distances, practice size, variation in staffing levels or perceived differences in practice culture - these did not emerge as dominant trends within the quantitative dataset. Instead, they reflect individual experiences rather than widespread geographic patterns. Similarly, respondents in urban areas sometimes attributed difficulties to high population density, while those in rural areas described concerns around limited choice of practices, but these perspectives balanced out across the full dataset.
Several respondents highlighted positive examples of practices that offered efficient triage systems, flexible use of digital tools, or good communication with patients. These examples appeared across multiple Trusts and did not cluster in any particular area, reinforcing the view that variability in access is more dependent on practice-level processes and systems than on geographic region.
Overall, the analysis indicates that regional variation accounts for only a small proportion of the differences in respondent experience. Shared themes across Trust areas point to overarching structural pressures within the general practice system in Northern Ireland. These pressures include telephone congestion, appointment scarcity, reliance on remote consultations, limited pre-booking options, and challenges navigating administrative systems.
8. Conclusion
The survey findings provide a clear and compelling picture of significant patient difficulty in accessing GP services in Northern Ireland. Across all Trust areas, respondents consistently reported barriers in securing appointments, getting through by telephone, obtaining routine follow-up care, and accessing face-to-face consultations. These challenges result in delayed care, reduced confidence in primary care systems, and a notable shift in patient behaviour towards out-of-hours services, Accident & Emergency departments, and private healthcare.
Telephone access remains the central bottleneck, amplified by limited booking windows, high call volumes, and the withdrawal or inconsistency of online booking systems. Reduced availability of routine and urgent appointments - and the dominance of remote consultations - has led to concerns about clinical appropriateness, misdiagnosis, and repeated follow-up appointments.
As a result, many patients reported deterioration of conditions, prolonged illness, challenges in managing chronic disease, delays in obtaining test results, and difficulties accessing essential medication reviews. These experiences contribute to increased pressure on urgent and emergency services.
Equity concerns was evident from the data. Patients with disabilities, the elderly, those reliant on others for phone access, people with poor hearing, limited digital literacy, or caring responsibilities face particular disadvantage. A lack of continuity of care and inconsistent triage processes further exacerbate these risks.
However, despite the overall negative sentiment, there were examples of effective practice. Some practices have adopted innovative or streamlined approaches that patients view as accessible, respectful, and efficient.
Overall, the findings point to a system under considerable strain. However, while the overall picture is one of widespread access difficulty, some respondents reported positive experiences, indicating that some practices have developed more effective systems. These examples of good practice may offer valuable insights for improving access more widely in the future.
Appendix
Appendix 1: Survey responses from individuals across all Health and Social Care Trust areas in Northern Ireland
Q6 - On a scale of 1 to 5 how would you rate your overall experience on accessing GP services in the past 12 months? (1 poor - 5 excellent)
|
Rating |
Belfast HSCT |
South Eastern HSCT |
Southern HSCT |
Northern HSCT |
Western HSCT |
|
|
1 - Poor |
47% |
51% |
53% |
51% |
52% |
|
|
2 |
22% |
22% |
21% |
22% |
21% |
|
|
3 |
15% |
13% |
13% |
15% |
14% |
|
|
4 |
8% |
7% |
6% |
6% |
5% |
|
|
5 - Excellent |
5% |
4% |
5% |
4% |
5% |
|
Q7 - What are the main challenges you have faced when trying to access GP Services? (Tick all that apply)
|
Long wait times for an appointment |
51% |
52% |
47% |
41% |
43% |
|
Lack of face to face appointments |
66% |
71% |
71% |
70% |
66% |
|
Limited availability of same day / urgent appointments |
57% |
63% |
66% |
62% |
66% |
|
Limited availability of routine appointments |
56% |
61% |
58% |
59% |
65% |
|
Issues with online booking systems |
19% |
17% |
9% |
15% |
12% |
|
Difficulties using computers, smartphones or the internet |
5% |
4% |
3% |
4% |
4% |
|
English is not your first language |
0.32% |
0.18% |
0.13% |
0.20% |
0.14% |
|
A disability or health condition |
9% |
7% |
6% |
7% |
8% |
Q8 - When did you last try to make a GP appointment?
|
Option |
Belfast HSCT |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
||
|
In the last 3 months |
69% |
69% |
70% |
71% |
72% |
||
|
Between 3 and 6 months |
16% |
16% |
15% |
15% |
15% |
||
|
Between 6 and 12 months |
8% |
9% |
8% |
8% |
7% |
||
|
More than 12 months |
4% |
3% |
3% |
3% |
2% |
||
|
Don't know |
0.84% |
1.20% |
1.11% |
1.08% |
0.91% |
||
Q9 - How do you usually book an appointment?
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
||
|
Phone |
93% |
92% |
96% |
94% |
96% |
||
|
Online |
3% |
3% |
1% |
1% |
0.34% |
||
|
In person |
2% |
3% |
2% |
3% |
3% |
||
Q10 - Generally, how easy is it to get through to someone at your GP practice on the phone?
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
||
|
Very easy |
3% |
2% |
2% |
1% |
2% |
||
|
Fairly easy |
12% |
10% |
9% |
9% |
8% |
||
|
Not easy |
22% |
20% |
20% |
20% |
19% |
||
|
Not at all easy |
62% |
66% |
67% |
68% |
68% |
||
|
Haven't tried |
0.17% |
0.13% |
0.17% |
0.09% |
0.34% |
||
Q11 - How long did you have to wait for your most routine GP appointment?
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
|
|
Same day |
8% |
5% |
9% |
11% |
8% |
|
|
1-3 days |
12% |
9% |
12% |
12% |
14% |
|
|
4-7 days |
8% |
7% |
7% |
7% |
8% |
|
|
More than a week |
17% |
15% |
14% |
11% |
13% |
|
|
More than 2 weeks |
19% |
22% |
13% |
14% |
13% |
|
|
I did not get an appointment |
28% |
33% |
37% |
38% |
38% |
|
|
I did not require an appointment |
5% |
4% |
4% |
5% |
3% |
|
Q12 - How long did you have to wait for your most urgent GP appointment?
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
|
|
Same day |
34% |
29% |
32% |
36% |
34% |
|
|
1-3 days |
22% |
22% |
24% |
21% |
25% |
|
|
4-7 days |
6% |
5% |
4% |
4% |
4% |
|
|
More than a week |
5% |
6% |
5% |
4% |
5% |
|
|
More than 2 weeks |
3% |
4% |
3% |
2% |
2% |
|
|
I did not get an appointment |
13% |
16% |
18% |
17% |
16% |
|
|
I did not require an appointment |
13% |
14% |
10% |
12% |
12% |
|
Q13 - Before you tried to get your most recent appointment, did you do any of the following? (Please tick all that apply)
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
|
|
I looked for information online |
57% |
57 % |
55% |
57 % |
50% |
|
|
I spoke to a Pharmacist |
40% |
44% |
46 % |
39% |
41% |
|
|
I tried to treat myself or the person I was making the appointment for |
57% |
58% |
61% |
59% |
60% |
|
|
Went to or contacted another NH Service |
9% |
9% |
10% |
8% |
9% |
|
|
Asked for advice from a family member or friend |
31% |
30% |
31% |
32% |
30% |
|
|
Tried to get information or advice from elsewhere |
34% |
34% |
34% |
34% |
35% |
|
|
I did not try to get information or advice |
11% |
9% |
8% |
11% |
11% |
|
Q14 - What type of consultation was offered for your last GP appointment?
|
Option |
Belfast HSCT |
South Eastern HSCT |
Southern HSCT |
Northern HSCT |
Western HSCT |
|
Face to face |
32% |
32% |
31% |
32% |
45% |
|
Telephone |
66% |
67% |
67% |
67% |
54% |
|
Video call |
0.17% |
0.16% |
0.17% |
0.13% |
0.11% |
|
Home Visit |
0.04% |
0.10% |
0.17% |
0.11% |
0.06% |
Q15 - Did you feel the type of consultation you were offered was appropriate for your health concern?
|
Option |
Belfast HSCT |
South Eastern HSCT |
Southern HSCT |
Northern HSCT |
Western HSCT |
|
|
Yes |
44% |
43% |
38% |
42% |
47% |
|
|
No |
43% |
45% |
49% |
46% |
41% |
|
|
Not sure |
11% |
11% |
11% |
11% |
11% |
|
Q16 - If you had a telephone / video conference did you feel that your issue was fully addressed?
|
Option |
Belfast HSCT |
South Eastern HSCT |
Southern HSCT |
Northern HSCT |
Western HSCT |
|
|
Yes |
25% |
20% |
19% |
20% |
16% |
|
|
No |
41% |
42% |
46% |
43% |
38% |
|
|
Not sure |
19% |
19% |
20% |
20% |
25% |
|
|
Not answered |
14% |
17% |
13% |
15% |
19% |
|
Q17 - Did you need a follow-up in person appointment?
|
Option |
Belfast HSCT |
South Eastern HSCT |
Southern HSCT |
Northern HSCT |
Western HSCT |
|
|
Yes |
50% |
47% |
48% |
49% |
46% |
|
|
No |
49% |
52% |
51% |
50% |
53% |
|
Q18 - How satisfied were you with the appointment that was offered to you?
|
Rating |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
|
|
Very satisfied |
18% |
15% |
14% |
15% |
16% |
|
|
Fairly satisfied |
23% |
21% |
21% |
22% |
22% |
|
|
Neither satisfied nor dissatisfied |
18% |
18% |
18% |
19% |
19% |
|
|
Fairly dissatisfied |
15% |
15% |
15% |
14% |
14% |
|
|
Very dissatisfied |
14% |
15% |
16% |
15% |
13% |
|
|
I was unable to get an appointment |
9% |
14% |
13% |
12% |
12% |
|
Q19 - Have you ever had to delay seeking medical help because of difficulties accessing GP Services?
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
|
|
Yes |
72% |
76% |
75% |
75% |
78% |
|
|
No |
27% |
23% |
24% |
24% |
21% |
|
|
Not Answered |
0% |
0% |
0% |
0.02% |
0% |
|
Q20 - What did you do if you were unable to get a suitable appointment?
|
Option |
Belfast HSTC |
South Eastern HSTC |
Southern HSTC |
Northern HSTC |
Western HSTC |
|
|
Does not apply |
15% |
9% |
12% |
14% |
12% |
|
|
Try to contact my GP another time |
22% |
20% |
22% |
21% |
20% |
|
|
Went to A&E |
12% |
12% |
12% |
11% |
13% |
|
|
Contacts Out of Hours GP |
10% |
12% |
9.57% |
11% |
11% |
|
|
Spoke to a Pharmacist |
6% |
6% |
8.47% |
6% |
8% |
|
|
Looked for information online |
9% |
11% |
9% |
10% |
10% |
|
|
Spoke to a friend or family member for advice |
3% |
3% |
3% |
4% |
4% |
|
|
Contacted a private healthcare provider |
9% |
12% |
13% |
9% |
8% |
|
|
Did Nothing |
8% |
7% |
9% |
10% |
9% |
|
|
Not answered |
0% |
3% |
0% |
0.03% |
0% |
|
Q21 - As far as you know, which of the following services does you GP offer?
|
Option |
Belfast HSCT |
South Eastern HSCT |
Southern HSCT |
Northern HSCT |
Western HSCT |
|
|
Booking appointments online |
19% |
17% |
10% |
13% |
8% |
|
|
Ordering repeat prescriptions online |
68% |
68% |
62% |
73% |
66% |
|
|
None of these |
18% |
18% |
23% |
15% |
20% |
|
|
Don't know |
12% |
11% |
13% |
10% |
13% |
|