Inquiry Report on the Impact of COVID-19 in Care Homes
Session: Session currently unavailable
Date: 01 February 2021
Reference: NIA 59/17-22
Health Committee Inquiry Report on Impact of COVID-19 in Care Homes.pdf (983.32 kb)
Ordered by the Committee for Health to be printed on 21 January 2021
Report: NIA 59/17-22
This report is embargoed until the commencement of the debate in the Assembly on 1 February 2021
Mandate 2017 - 2022
Powers and Membership
The Committee for Health is a Statutory Departmental Committee established in accordance with paragraphs 8 and 9 of Strand One of the Belfast Agreement 1998 and under Assembly Standing Order 48. The Committee has a scrutiny, policy development and consultation role with respect to the Department for Health and has a role in the initiation of legislation.
The Committee has power to:
-
consider and advise on Departmental budgets and annual plans in the context of the overall budget allocation;
-
consider subordinate legislation and take the Committee Stage of primary legislation;
-
call for persons and papers;
-
initiate inquiries and make reports; and
-
consider and advise on matters brought to the Committee by the Minister of Health.
The Committee has nine members, including a Chairperson and Deputy Chairperson, and a quorum of five. The membership of the Committee is:
Mr Colm Gildernew MLA (Chairperson)
Ms Pam Cameron MLA (Deputy Chairperson)
Ms Paula Bradshaw MLA
Mr Jonathan Buckley MLA1
Mr Gerry Carroll MLA
Mr Alan Chambers MLA2
Ms Órlaithí Flynn MLA
Ms Cara Hunter MLA3
Mr Pat Sheehan MLA4
List of Abbreviations and acronyms used in the report
| Acronym | Full Form |
|---|---|
|
ACP |
Advance care planning |
|
AGPs |
Aerosol-generating procedures |
|
AHP |
Allied Health Professions |
|
ARC |
Association for Real Change NI |
|
BASW |
British Association of Social Workers NI |
|
BMA |
British Medical Association NI |
|
BSO |
Business Services Organisation |
|
CMO |
Chief Medical Officer, Department of Health |
|
CNO |
Chief Nursing Officer, Department of Health |
|
COPNI |
The Commissioner for Older People for NI |
|
CSW |
Chief Social Worker, Department of Health |
|
DoH |
Department of Health |
|
DNACPR |
Do Not Attempt Cardiopulmonary Resuscitation |
|
DNR |
Do Not Resuscitate |
|
ECDC |
European Centre for Disease Prevention and Control |
|
GMS |
General Medical Services |
|
HSC |
Health and Social Care |
|
HSCB |
Health and Social Care Board |
|
HSCT |
Health and Social Care Trust |
|
IHCP |
Independent Health and Care Providers |
|
IPC |
Infection prevention and control |
|
KIS |
Key Information Summary |
|
NICE |
National Institute for Health and Care Excellence |
|
NIHRC |
Northern Ireland Human Rights Commission |
|
NISCC |
NI Social Care Council |
|
PCC |
Patient and Client Council |
|
PCiP |
Palliative Care in Partnership Programme |
|
PHA |
Public Health Agency |
|
PPE |
Personal protective equipment |
|
RCGP |
Royal College of General Practitioners NI |
|
RCN |
Royal College of Nursing |
|
RCPsych |
Royal College of Psychiatrists in NI |
|
RLI |
Rapid Learning Initiative |
|
RPMG |
Regional Palliative Medicines Group |
|
RQIA |
Regulation and Quality Improvement Authority |
|
SSP |
Statutory sick-pay |
|
SST |
Service Support Team |
Contents
- Powers and Membership
- List of Abbreviations and Acronyms used in the Report
- Executive Summary
- Introduction
- Context
- Consideration of Evidence
- Findings and Recommendations
- Appendix 1 Minutes of Proceedings
- Appendix 2 Minutes of Evidence
- Appendix 3 Written submissions
- Appendix 4 NIA Research Papers
- Appendix 5 Memoranda and Papers from the Department of Health
- Appendix 6 Additional Papers considered by the Committee
Executive Summary
Introduction
1. The Health Committee decided in July 2020, based on evidence it had taken in the spring in relation to the particular impact of COVID-19 on care homes, to conduct a short inquiry, in order to produce recommendations to help mitigate and manage the impact of a potential second surge of the virus in care homes.
2. A research briefing was commissioned and Members agreed terms of reference in September. The terms of reference for the inquiry were to:
- identify the key issues impacting care homes as a result of the COVID-19 pandemic;
- identify domestic and international examples of best practice in arrangements to protect and care for residents of care homes during the pandemic; and
- report to the Assembly on its findings and recommendations by 13 November 20205.
3. The Committee agreed that due to the timescales within which it wished to complete the inquiry, it would not seek public evidence but, instead, would seek written submissions from a targeted group of key stakeholders on the areas of focus identified through its review. The Committee received 21 submissions from a range of organisations spanning public, private and charitable organisations, professional bodies and trade unions.
4. The Committee also held oral evidence sessions with a number of the key stakeholders as well as oral evidence sessions with senior Department of Health officials including the Chief Nursing Officer and Chief Social Worker.
5. The Committee further agreed that it would take account of existing reports, research papers and international best practice; as well as commissioning further research from RaISe to assist the Committee in its consideration of the discharge of care home residents from hospital and the experience of public versus private care home settings.
6. The Committee was also keen to learn directly from the experience of those most impacted, and considered ways in which it could safely engage with, and garner the views of the residents of care homes, their families and care home staff in its inquiry. The Committee's engagement with these groups was carried out by holding a virtual informal meeting with family members of care home residents facilitated by PCC, COPNI and AGE NI; and through an online survey seeking the views of owners/ managers, staff and residents/ family members.
7. The Committee's online survey was launched on 10 October 2020 and was promoted via Facebook, Twitter and emailed directly to key stakeholder groups. Twenty randomly selected care homes from each county were also contacted to encourage participation and ensure regional spread. The survey closed on 19 October 2020 with 691 respondents.
8. The definition of care home, for the purpose of the inquiry, is one registered with the Regulation and Quality Improvement Authority (RQIA) as a nursing home or residential care home, in accordance with the Health and Personal Social Services (Quality, Improvement and Regulation) (Northern Ireland) Order 2003.
9. As at 13 October 20206, there were 482 registered care homes in Northern Ireland, of which 434 (90%) were independently owned and operated and 48 (10%) were publicly owned and operated. The total number of registered beds was 16,110.
10. According to NISRA statistics for the year 20207, 775 care home residents had died with COVID-19 (some in hospital), constituting around 40% of the 1895 COVID-related deaths registered during the previous twelve months. Sadly, these figures continue to grow, despite restrictions.
11. In undertaking the inquiry, the Committee was conscious of the context in which the pandemic impacted care homes, in terms of long-standing issues of workforce shortages, an acknowledged need for reform and a three-year period when there was no Executive and no Minister in place, from 2017-2020. The report acknowledges the Minister's commitment to reform and his initiatives to deal with the pandemic to date, including providing additional funding, HSC staff support and initiating the Rapid Learning Initiative and plans to develop a Framework for Enhanced Clinical Care in care homes.
12. Shortly before the report was agreed, the HSC began to roll out the vaccination programme; while the Committee welcomes the enormous progress this represents, it offers its recommendations in a spirit of constructive engagement, pending full protection of the population and as a contribution to future pandemic planning.
13. The Committee wishes to put on record its gratitude to the organisations and individuals who participated in the inquiry through the provision of written and oral evidence, informal engagement and by taking part in the Committee's online survey. The Committee also wishes to thank the Committee staff team and acknowledge the input from RaISe and Engagement teams also.
Findings and Recommendations
Visiting
14. The Committee heard compelling evidence around the importance of family contact with residents; the negative and sometimes traumatic impact of visiting restrictions on the physical and mental wellbeing of residents – and on the mental health of carers; and the vital role families play, in the care of their loved ones.
15. Members recognise that facilitating safe visiting is closely linked to issues around testing and PPE; and that there are resource implications. The Committee welcomed indications that the latest funding could be used for infrastructure upgrades including the installation of visiting pods.
16. The Committee was struck by how frequently communication issues were raised across the various strands of the inquiry but particularly in relation to decision- making around visiting. Members were moved by testimony given by family members at an informal meeting, where they described the impact of recent months on their loved ones and their families and the lack of input they had into decisions around visiting.
17. It is noted that the most recent guidance on visiting confirms that care home managers are expected to make decisions based on a dynamic risk assessment of conditions in their community, taking account of the guidance.
18. Evidence gathered by the Committee also highlighted, however, that individual circumstances including health needs, determine what is feasible and desirable in terms of visiting. For some residents with cognitive decline, or significant sensory impairment, virtual visiting is simply not workable.
Recommendations
Recommendation 1: The Committee recommends that safe and meaningful visiting be facilitated and resourced through the identification, development and implementation of innovative measures.
Recommendation 2: The Committee recommends that residents and families be involved directly in decision-making around visiting, to ensure that the particular needs and circumstances of each resident is considered, including their, and their family's, attitude to risk.
Recommendation 3: The Committee recommends further work in the area of messaging and communication around visiting, COVID-19 outbreaks in homes, including direct communication with families in respect of their loved ones and wider developments affecting the home in which their family member resides.
Recommendation 4: The Committee calls for the implementation of the care partner initiative to be expedited, supported by urgent work with unions and providers to resolve issues raised, including safeguarding, insurance, role specification and testing.
Recommendation 5: PPE must be provided as required to facilitate safe visiting.
Recommendation 6: The Committee recommends that the implementation of visiting guidance be monitored across care homes to ensure consistency and compliance with best practice.
Testing
19. The Committee noted that the context had changed significantly since the outbreak of the pandemic, in terms of testing capacity, increased frequency of testing, regular symptom-monitoring and new approaches.
20. Members also recognised, however, the resource implications of increased testing, in terms of the impact on staff time and additional training requirements.
21. Consistent with the findings of the Rapid Learning Initiative, the Committee was concerned by evidence that care homes do not necessarily have all the required equipment, or adequately trained staff, to undertake symptom-monitoring in line with guidance.
22. The Committee sought particular advice on human rights and consent issues in respect of testing, in view of the frail health of many residents, particularly those with cognitive impairment. Members noted the competing rights at stake due to the potentially lethal nature of the disease but hopes that new, rapid tests hold out the hope of a less invasive means of keeping residents safe.
23. At the time of writing, the Minister was seeking to introduce mass and rapid testing and roll out the vaccination programme, which the Committee sees as having transformative potential, particularly given the high numbers of asymptomatic cases.
Recommendations
Recommendation 7: The Committee recommends that, subject to rapid testing becoming available, care home workers should be tested daily8; those moving between homes be tested before entry to any home; and residents should continue to be tested as frequently as necessary and at least fortnightly.
Recommendation 8: Testing should be extended to all those entering care homes including visitors, care partners, residents returning from an external appointment, and all professionals entering homes; and should take place as often as necessary to take advantage of improvements in testing capabilities.
Recommendation 9: The Committee recommends that local capacity to undertake testing and process results should be increased to improve timeliness of results.
Recommendation 10: Pooled testing9 should be explored as a means of enhancing testing capacity.
Recommendation 11: Access to, and training in the use of, appropriate clinical equipment should be provided as a priority, to facilitate effective twice-daily symptom-monitoring; and compliance with guidance on symptom-monitoring should be included in regular checks.
Recommendation 12: Further research should be undertaken to establish the means by which the virus is getting into homes, whether via staff or deliveries etc.
Recommendation 13: The Committee recommends that further consideration be given to the capture and analysis of testing data, such as asymptomatic positive tests, to inform the pandemic response.
Recommendation 14: Guidance should be reviewed to ensure consideration of human rights issues around testing.
Discharge Policy
24. The Committee remains concerned that the discharge of COVID-19 positive patients to care homes presents an enduring risk, though it is also cognisant of the pressures on hospital beds and the challenges of providing isolation via step- down care, including the additional disruption and distress this could cause.
25. Members discussed the evidence that many homes struggle to isolate individuals, either for reasons of facilities and adequate staff resource or, equally importantly, residents' wellbeing and issues of understanding amongst the significant numbers of residents with cognitive decline.
26. The Committee noted with concern, research suggesting increasing recognition of the danger of discharging people directly from hospital into care homes, without ideally two negative tests within 24 hours, due to the risk of false negative tests, even in the case of those not originally hospitalised for COVID-19.
27. While it is hoped that news of vaccines and rapid-testing will transform the situation, in addition to twice-daily symptom monitoring, the Committee nevertheless makes the following recommendations.
Recommendations
Recommendation 15: The Committee recommends that no-one be discharged from hospital to a care home in which they are a resident, without having tested negative for COVID-19, unless the care home confirms that it has the staffing and facilities to ensure isolation for the required period; and that this is subject to monitoring and review.
Recommendation 16: New residents should not be admitted to a care home unless they have tested negative.
Recommendation 17: The Committee recommends that the potential benefits of step-down isolation facilities be explored.
Access to PPE
28. The Committee heard persuasive and consistent evidence of shortages of appropriate PPE in the early months of the pandemic, which caused real anxiety for staff. Independent providers struggled to source their own PPE given vast price increases and global pressures on supply. There were also concerns about communication and consistency across the HSC but, by May, stakeholders were reporting significant improvements, including the establishment of a single point of contact with Trusts, revised guidance on PPE use, as well as centralised procurement and provision free of charge to care homes, in line with practice in other countries identified in research.
29. The Committee welcomed these initiatives and the continuing, but temporary, commitment to carry on providing PPE without charge, but acknowledges that there is a longer-term question to be considered about procurement and payment, given increased cost-burden to providers and the additional PPE requirements associated with facilitating safe visiting, as considered elsewhere in this report.
30. Effective use of PPE has required additional training, consideration of changing areas and is linked to oversight of infection prevention and control10, more generally. It also begs questions about how to overcome adverse effects such as the additional challenges entailed in residents not being able to see the faces of loved ones and those who care for them, a particular issue for those with hearing impairment or cognitive decline. Guidance has been produced but further research may be beneficial.
Recommendations
Recommendation 18: The Committee recommends that during a pandemic, there should be centralised procurement and supply of PPE to care homes, without charge.
Recommendation 19: Further charges for PPE should not be imposed care homes without a review of the tariff.
Recommendation 20: Training remains critical and all staff should be able to access regular and prompt updates as new knowledge or innovations emerge.
Recommendation 21: Consistency in the use of PPE should continue to be monitored.
Funding
31. The degree to which COVID-19 exacerbated the pre-existing financial strain on the care home sector, is well documented. The pandemic response resulted in increased staffing costs, enhanced cleaning and other infection-control measures; and costs associated with facilitating visiting.
32. The Committee welcomes the Department's initiatives to support care homes including through block-booking of vacant beds; offering staff support from the HSC and providing significant additional funding allocations.
33. Questions remain, however, about the criteria and processes for making claims and the Committee was concerned to hear of significant under-spends as a result, but welcomed news that the Department was seeking to address these issues in relation to the latest tranche of funding allocated in October.
34. Consistent with other sections of this report, there is a sense that earlier and more intensive engagement with stakeholders in advance of making decisions, may have averted some of the difficulties.
Recommendations
Recommendation 22: The Committee recommends that streamlined processes be developed for administering funding, subject to audit and verification, but flexibly enough to allow care homes to meet their particular needs.
Recommendation 23: Funding for adult social care should be considered as a whole, including care packages and day-centre capacity which impact on care home pressures and bed-flow across the system.
Recommendation 24: The Committee recommends that work be prioritised to establish the 'true cost of care' as part of wider reform.
Staff Terms and Conditions
35. The Committee wishes to acknowledge the skill and value of the work in care homes; the particular personal qualities shared by many for whom it is a vocation rather than a job; and the need to look at recognition, reward and retention in what is a challenging environment.
36. Members also acknowledge the toll the pandemic has taken on staff in terms of their own health and wellbeing, including mental health, and welcomed the
extension to care home staff of access to the Trusts' mental health helpline.
37. There was also recognition of the differing financial impact that new requirements might have on care homes, given the variation in size and profitability; and acknowledgement that viability was in question in some cases. It is accepted that several recommendations may require a review of the tariff.
38. The Committee agreed that staff terms and conditions in the sector were problematic prior to the pandemic and that the lack of guaranteed sick-pay for many was not only unfair to staff but constituted a risk to wellbeing of staff and residents. Members therefore welcomed the Minister's decision to provide funding for sick-pay, noting with concern, however, that it was not back-dated to the start of the pandemic.
Recommendations
Recommendation 25: The Committee welcomes the Minister's commitment to progress reform urgently and calls for low pay and poor terms and conditions to be addressed as quickly as possible.
Recommendation 26: The Committee recommends that the Department set minimum standards for sick-pay in care home workers' contracts and that arrangements be put in place to ensure standards are adhered to.
Recommendation 27: In the interim, the Committee recommends that any additional funding provided to care homes should include conditions regarding fair pay and treatment.
Recommendation 28: The Committee recommends consideration of additional measures to make social care a more attractive career, including developing career pathways.
Staff Levels and Issues
39. The Committee recognises that staffing levels were a significant problem prior to the pandemic and heard repeatedly throughout recent months how this was exacerbated due to sickness absence, self-isolation, lack of childcare facilities during the first lockdown, and added caring responsibilities as day-centres were also closed.
40. In addition, the Committee heard convincing evidence of the greater demands placed on staff time for a range of reasons including testing, symptom-monitoring, increased IPC measures and additional care requirements as residents became unwell.
41. The use of agency workers, while unavoidable given the stated pressures, raised concerns about increased risk of transmission through staff movement between homes. The Committee acknowledged that its survey provided some encouraging evidence that this risk was recognised and that managers had sought to minimise staff movement between homes.
42. The Committee welcomed the support offered by Trusts to care homes, in terms of re-deploying HSC staff, but it was recognised that this created difficulties in the HSC. The service was also suffering pre-existing workforce shortages and was struggling in the second wave, given additional efforts to maintain HSC services, in tandem with the COVID-19 response.
43. Other initiatives were also welcomed such as regulatory change to facilitate rapid recruitment, subject to safeguards, and flexibility in staffing ratios, introduced by RQIA, as well as an app to allow RQIA to monitor staffing requirements across homes.
44. While additional training was made available and was welcomed, the Committee noted that in some cases, the pressure was such that staff could not be released to attend.
Recommendations
Recommendation 29: The Committee recommends that appropriate staff ratios for care homes be agreed in discussion with stakeholders.
Recommendation 30: Strenuous efforts must continue to be made to minimise staff movement between homes and, where possible, agency staff should work at one home only.
Recommendation 31: The Committee recommends that care home providers be required and supported to put in place robust measures to ensure the safety of BAME staff and other staff at increased risk from the virus.
Access to Health and Social Care
45. The Committee has been impressed with the rapid innovation and scaling up of the use of technology, to provide safe, timely and effective care during the pandemic; and acknowledges the enormous effort and dedication that this has required across the system.
46. Nevertheless, the Committee also recognises that there are limits to approaches such as 'virtual ward-rounds' and that, moving forward, the balance can be improved in terms of in-person care and also communication with loved ones who would ordinarily have been more closely involved in care.
47. The Committee was concerned to hear of the adverse impact on residents, of reduced access to podiatry, occupational health and other care. Evidence suggests one reason in-person access was limited, was due to inconsistent implementation of Departmental guidance which advises that appointments should continue where the relevant HSC professional deems it appropriate.
48. The Committee welcomes the ongoing work being led by the Chief Nursing Officer on an Enhanced Clinical Care Framework for care homes, including medical, nursing and multi-disciplinary care, to meet the higher degree of healthcare needs within care homes in recent years.
49. Advance Care Planning is another issue that was brought to the Committee's attention in recent months and the Committee acknowledges the sensitivity of such conversations and the importance of this matter being dealt with on an individual basis, supported by the appropriate professional and taking account of the unique needs, preferences and changing circumstances of the individual, ideally well in advance of a crisis. The Committee also notes that ACP goes well beyond circumstances where resuscitation is appropriate and covers a wide range of care and treatment preferences, in a variety of circumstances. The Committee notes the pressure felt by some care home staff to lead these important conversations for which they felt further training and medical input was required.
Recommendations
Recommendation 32: The Committee recommends that the Enhanced Clinical Care Framework should embed the principles of the acute care at home programme within care homes and should confirm GP participation.
Recommendation 33: There is a need for consistent implementation of the policy on in-person access to care homes, as deemed necessary by the HSC professionals concerned, and subject to testing and PPE requirements.
Advance Care Planning
Recommendation 34: Advance Care Planning should be discussed with each care home resident, on an individual basis, ideally ahead of any crisis; it should be led by the clinician who knows the individual best, with the input of other relevant professionals; and reviewed as necessary.
Recommendation 35: The Department of Health should clearly outline and communicate the rights of older people and families regarding end-of-life planning and this should reference the approach to treatment and care planning recommended under NICE guideline NG163.
Recommendation 36: Steps should be taken to ensure that relevant professionals have access to appropriate training in advance care planning.
Regulation
50. When it emerged in the spring that the Department had instructed the RQIA to suspend routine inspections and increase its emphasis on support and advice, the Committee considered the balance between regulation and assistance, enquiring about oversight, enforcement and shared characteristics of homes experiencing outbreaks.
51. The Committee recognises the strength of evidence expressing appreciation for the support and advice provided by RQIA, particularly during the first difficult months of the pandemic, including a first point of contact 'Service Support Team' and on-site support teams assisting homes to improve IPC. This is mirrored by concerns about the scaling back of the advice service during the autumn, as RQIA sought to increase inspections.
52. Members also acknowledge, however, concerns raised by stakeholders about the risks inherent in the lack of oversight when in-person inspections were reduced, particularly as it coincided with visiting restrictions. While some in-person inspections and virtual inspections continued, the Committee notes that virtual inspections were described as creating a greater administrative burden on homes, at a difficult time.
53. RQIA research identified a number of key characteristics associated with homes most at risk of an outbreak, including: larger homes (40+ registered places); homes run by larger providers; homes located in urban areas; services with more than two manager changes over the past year; and services registered within past 10 years. The Committee welcomes the RQIA's proposed move to a 'risk- based assurance framework' and the Minister's desire to see "change brought about so that, rather than just looking at an individual facility, a corporate provider can be inspected corporately".
54. Many stakeholders complained to the Committee of a lack of consistency in the implementation of Departmental guidance by care homes, convincing the Committee that there is work to be done in this area of regulation, as found by the RLI. The Committee recognises the link between this matter and issues raised frequently around communication of guidance.
55. The Committee was concerned by the resignation of the RQIA board in June and their criticism of the Department's approach. The Committee sought changes to the terms of reference for the subsequent inquiry, which were agreed to by the Minister. In this context, the Committee welcomes the ongoing review of regulation announced by the Minister in June.
Recommendations
Recommendation 37: The Committee recommends that additional resource be provided to ensure that routine inspections continue, subject to appropriate PPE and testing, in tandem with a high level of dedicated advice and support for care homes, during a pandemic.
Recommendation 38: Additional monitoring is required to ensure the consistent implementation of guidance and policy.
Recommendation 39: The Committee believes there must be consequences for failures of care and recommends consideration of models by which quality and delivery of care, and adherence to guidance and best practice, could be linked to funding and considered in future contracting arrangements, including the capacity to recoup public funds where poor service has been evidenced.
Recommendation 40: The Committee recommends that further work be undertaken to improve communication of guidance across the different tiers of the system, including with unions.
Pandemic Preparedness and Systemic Issues
56. There was virtual consensus on a number of significant points in relation to pandemic planning. It is uncontested that care homes, and the HSC, were already dealing with workforce shortages, especially in key roles including care home staff and nursing. Neither is there any dispute in relation to the inadequacy of PPE supplies at the start of the pandemic and the impact of the time required to build up testing capacity.
57. While the Committee recognises the enormous pressure under which HSC and Departmental staff were working at all levels, and the considerable volume of guidance developed and advice put in place, communication and engagement issues were central to criticisms raised. The Committee was concerned to hear, on several occasions, that initiatives had been introduced without prior engagement with providers or unions. The Committee finds that this undermined confidence, as gaps and questions arose that could potentially have been addressed through co-design of the policies. Communication was also one of the key issues raised by families, as set out earlier, particularly in relation to visiting and regulation.
58. The pandemic has had knock-on effects on mental health which will endure for some time; further work is needed to understand and mitigate the effects of the pandemic on the longer-term mental health of residents, families and care workers.
59. The Committee also considered the human rights issues arising due to pandemic restrictions on visiting and testing, particularly in respect of those with cognitive decline. The Committee found a need for greater support for providers and HSC workers in this area, including clarity around implementation of Deprivation of Liberty Safeguards in a pandemic context.
60. Having had initial discussions on best practice internationally, the Committee is not persuaded from its engagement with the Department, that adequate measures are in place to engage with, and learn from, countries that benefited from previous pandemic experience and have dealt best with COVID-19.
61. The Committee finds that the pre-existing strains on adult social care highlighted in the 'Power to People' report, have been exacerbated by the pandemic and that reform is urgently needed to address the range of issues identified in this report, from staff terms and conditions to regulation, funding and the costs and benefits of public or private provision of this vital public service.
62. The Minister's commitment to progressing adult social care reform is acknowledged and the Committee looks forward to engaging further with the Department as reform progresses.
63. Finally, the Committee acknowledges the many other settings, outside the scope of this inquiry, which were similarly impacted by the pandemic, such as domiciliary care and day-centres and trusts that there may be some useful read- across from this report.
Recommendations
Recommendation 41: The Committee recommends that the requirements of care homes are central to detailed pandemic planning for the future, including PPE, infection control and visiting facilities.
Recommendation 42: The Committee recommends that consideration be given to having ring-fenced funding available that could be accessed quickly by care homes in any future pandemic.
Recommendation 43: The Department should consider how to maintain streamlined systems such that, in any future pandemic, funds could more quickly and easily be released, ideally by a single nominated body, on the basis of fair and transparent criteria, and appropriately back-dated to the start of the pandemic.
Recommendation 44: The Committee recommends that future pandemic planning should factor in the central procurement and supply of PPE to care homes.
Recommendation 45: Pandemic planning should include consideration of the particular needs of those with cognitive decline and this should inform dedicated guidance, on testing, ability to isolate, application of deprivation of liberty safeguards, meaningful contact with family and access to health and social care services not based in the care home.
Recommendation 46: Dedicated efforts should be made to gather and learn from the breadth of international experience of pandemic planning and management.
Recommendation 47: The Committee notes the finding of the RLI that there is no recognised regional training on environmental cleanliness and endorses its recommendation that care home staff be provided with a 'freely accessible regional IPC training e-learning module'.
Recommendation 48: Each home should be required to appoint a designated and appropriately trained staff lead (other than the manager) for IPC, including disseminating guidance and training, with support from PHA.
Recommendation 49: A database should be established of designated IPC lead staff in care homes and this should be integrated into the regulatory and monitoring framework.
Recommendation 50: Effective engagement is required with all relevant stakeholders, including providers, unions and families, with policies developed on a co-design and co-production basis.
Recommendation 51: Robust communication plans must be put in place and monitored, to ensure families are promptly informed of key developments regarding the home in which their loved one resides, including staff shortages, infection outbreaks, inspection findings and changes to relevant guidance.
Recommendation 52: Pandemic plans should include ensuring rapid access for care homes to a single point of contact for advice and support, accessible twenty-four hours per day, seven days per week.
Recommendation 53: Guidance should be developed on consideration of human rights during a pandemic, including the right of residents to visits and communication with loved ones; and best practice on managing testing and self-isolation.
Recommendation 54: Bereavement and mental health support for staff, residents and families will be required beyond the short-term and should be resourced and promoted as required.
Introduction
64. At an informal planning meeting in July 2020, the Members of the Health Committee discussed the Committee's ongoing scrutiny role in relation to the
Department of Health's (DoH) response to the COVID-19 pandemic and how best the Committee could contribute to this work.
65. There was general consensus that the impact of COVID-19 on care homes was a matter of particular concern and was an area in which the Committee could potentially add value, particularly in advance of anticipated further surges of the virus. The Committee agreed to commission a research briefing paper to assist with its deliberations in relation to carrying out a focussed piece of work on care homes.
66. The Committee considered the commissioned research paper at its meeting on 10 September 2020 and agreed that it would conduct an inquiry into the impact of COVID-19 in care homes. The research paper can be found at Appendix 4.
Aim and Terms of Reference
67. The aim of the Committee's inquiry was to produce recommendations to mitigate and manage the impact of a potential second surge of coronavirus on care homes.
68. The terms of reference for the inquiry were to:
- identify the key issues impacting care homes as a result of the COVID-19 pandemic;
- identify domestic and international examples of best practice in arrangements to protect and care for residents of care homes during the pandemic; and
- report to the Assembly on its findings and recommendations by 13 November 2020.
Committee Approach
69. As the impact of COVID-19 had dominated the Committee's agenda for much of the year since March, the Committee agreed to review the evidence it had already gathered on care homes to identify the key issues of concern. This review was based on the evidence the Committee had heard from: care home sector representatives; the Commissioner for Older People (COPNI); the Regulation and Quality Improvement Authority (RQIA); Trade Unions; GPs; the Health Minister; Chief Medical Officer (CMO), Chief Scientific Adviser (CSA), Chief Social Worker (CSW) and Chief Nursing Officer (CNO).
70. The areas identified from the review, for further consideration, were:
- Discharge from hospitals to care homes;
- Access to PPE;
- Testing in care homes;
- Funding and increased costs for care homes;
- Staffing issues & levels;
- Staff pay and conditions;
- Visitors;
- Regulation: RQIA role, inspections & risk factors including public versus private ownership;
- Medical care within care homes and advance care planning; and
- Preparedness within the HSC and in care homes.
71. The Committee agreed that, due to the timescales within which it wished to complete the inquiry, it would not seek public evidence on the inquiry, but instead, would seek written submissions from a targeted group of key stakeholders on the areas of focus identified through its review. The Committee received 21 submissions from a range of organisations which are included at Appendix 3.
72. The Committee also held oral evidence sessions with a number of the key stakeholders as well as oral evidence sessions with senior Department of Health officials including the CNO and CSW. Hansards of the oral evidence sessions, including those that informed the Committee's key issue review, are included at Appendix 2.
73. The Committee further agreed that it would take account of existing reports, research papers and international best practice, as well as commissioning further research from RaISe to assist the Committee in its consideration of the discharge of care home residents from hospital and the experience of public versus private care home settings. An amended RaISe paper with the additional research requested by the Committee is included at Appendix 4 and the additional papers considered by the Committee are included at Appendix 6. Relevant papers and correspondence from the Department of Health that were considered by the Committee have been included at Appendix 5.
74. The Committee was also keen to learn directly from the experience of those most impacted, and considered ways in which it could safely engage with, and garner the views of, the residents of care homes, their families and care home staff. The Committee's engagement with these groups was carried out by holding a virtual informal meeting with family members of care home residents facilitated by the Patient and Client Council (PCC), COPNI and Age NI; and through an online survey seeking the views of owners/ managers (employers), staff and residents/family members. A report of the informal meeting has been included at Appendix 6.
75. The Committee's online survey was launched on 10 October 2020 and was promoted via Facebook and Twitter and emailed directly to key stakeholder groups. Twenty randomly selected care homes from each county were also contacted to encourage participation and ensure regional spread. The survey closed on 19 October 2020 with 691 respondents. A report on the survey findings is included at Appendix 6.
76. Shortly before the report was agreed, the HSC began to roll out the vaccination programme; while the Committee welcomes the enormous progress this represents, it offers its recommendations in a spirit of constructive engagement, pending full protection of the population and as a contribution to future pandemic planning.
Acknowledgements
77. The Committee wishes to put on record its gratitude to the organisations and individuals who participated in the inquiry through the provision of written and oral evidence, informal engagement and by taking part in the Committee's online survey. The Committee also wishes to thank the Committee staff team and acknowledge the input from RaISe and Engagement teams also.
Context for the Inquiry
COVID-19 and Care Home Statistics
78. The definition of care home, for the purpose of the inquiry, is one registered with the RQIA as a nursing home or residential care home, in accordance with the Health and Personal Social Services (Quality, Improvement and Regulation) (Northern Ireland) Order 2003.
79. As at 13 October 202011, there were 482 registered care homes in Northern Ireland, of which 434 (90%) were independently owned and operated and 48 (10%) were publicly owned and operated, as displayed in Table 1. The total number of registered beds was 16,110.
Table 1
| Nursing Homes | Residential Homes | Total | % | |
|---|---|---|---|---|
|
Independent |
243 |
191 |
434 |
90% |
|
Statutory |
5 |
43 |
48 |
10% |
|
Total |
248 |
234 |
482 |
100% |
80. Latest figures published on 1 January by NISRA showed that the total number of COVID-19 related deaths figure as of that date was 1,895 (including those registered up to and including 6 January). Of this total, 1,150 (60.7%) deaths took place in hospital, 607 (32.0%) in care homes, 10 (0.5%) in hospices and 128 (6.8%) at residential addresses or other locations. The 617 deaths which occurred in care homes and hospices involved 146 separate establishments.
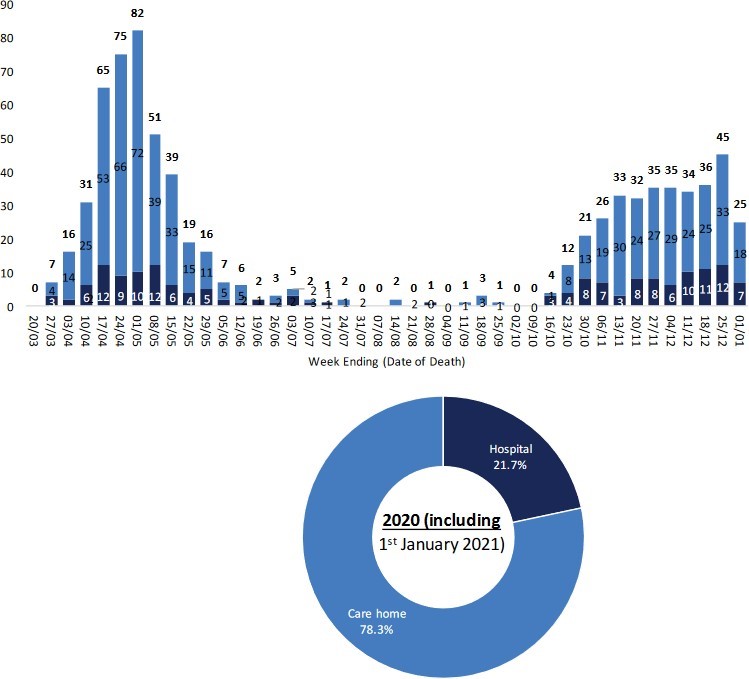
81. Further analysis, which includes deaths of care home residents in hospital, shows that of the 775 deaths of care home residents involving COVID-19 in 2020 and including 1 January 2021, which is 40.9% of all COVID-19 related deaths, 78.3% (607) occurred in a care home, with the remaining 168 occurring in hospital. Of the total deaths involving COVID-19 which occurred in hospital (1,150), 14.6% (168) were accounted for by care home residents.
82. Figure 1 profiles COVID-19 daily deaths of care home residents occurring by place of death, weekly and year-to-date 2020/2112.
Figure 1: Care home residents: COVID-19 deaths occurring by place of death, weekly and year-to-date 2020/21
Reform of Adult Care and Support
83. Every year in Northern Ireland, Health and Social Care Trusts (HSCT) spend over £900m on adult social care including day care, domiciliary care, residential and nursing home care.
84. In December 2016, an Expert Advisory Panel was established to provide an independent perspective on possible solutions to meet the challenges facing the adult care and support system and to develop proposals for reform. The Panel's 16 proposals are contained in the Report 'Power to People: proposals to reboot adult care and support in NI', (December 2017). An action plan based on the proposals is still being developed by a Departmental Reform Project Board and Project Team. This action plan will outline the DoH's proposed way forward for the reform of adult care and support and will form the basis of a public consultation.
New Decade, New Approach
85. The Northern Ireland Assembly entered a three-year deadlock in January 2017, when there was no Executive and no Minister of Health in place, which came to an end with the signing of the 'New Decade, New Approach' agreement in January 2020. In that document, the NI political parties agreed on a way forward for strengthening public services and tackling immediate challenges. In health, there was a particular focus on delivering the reform of health and social care.
Rapid Learning Initiative
86. DoH published the report of the 'Rapid Learning Initiative' (RLI) on 2 September 2020 on the experiences of care homes during the first surge of the COVID-19 pandemic.
87. The document identified 24 recommendations which the Health Minister said would help 'inform our approach as we face into a potentially very difficult autumn and winter.' The Minister went on to say that; 'Our care home sector was extremely fragile before the pandemic and the virus has exposed that. Northern Ireland is by no means unique in that regard. COVID-19 cruelly targets the oldest and most vulnerable citizens and care homes in many countries around the world have suffered devastating consequences.'
88. It was the view of the Health Committee that, whilst the RLI findings were helpful, they were high level in nature and the Committee thought it could add value. As a result, the Committee took the decision to continue with its inquiry into care homes, with a view to engaging more widely with those affected, for example, family members of residents.
Consideration of Evidence
Visiting
89. Restrictions on visiting has been perhaps the most emotive issue considered by the Committee as part of its inquiry. In the evidence considered by the Committee, there was widespread acknowledgement of the adverse impact that restrictions on visiting was having on care home residents and their families. There was also clear recognition of the importance of protecting care home residents, and a general acknowledgement that there were no easy answers to this issue. All contributors agreed that efforts should be made to restore meaningful contact between residents and their families by finding ways to mitigate the risk that visiting presents.
90. Both COPNI and the PCC advised the Committee that visiting was the issue of concern for which their respective offices had been contacted most frequently.
91. COPNI felt there was a need to facilitate some sort of safe visiting. This view was shared by Age NI, who advised, that compassion, person-centred care and judgement are all required when considering how to facilitate safe visiting during the pandemic. The British Association of Social Workers NI (BASW) and the Health and Social Care Board (HSCB) considered there was a need to balance risk with the emotional health and wellbeing of residents, while the South Eastern Trust acknowledged that providing that balance had been challenging for providers.
92. The Royal College of General Practitioners NI (RCGP) and BASW acknowledged the risks and difficulties associated with visiting, but called for consideration of the impact that no social contact was having on psychological wellbeing. These concerns were shared by the Royal College of Psychiatrists in NI (RCPsych), who highlighted the effects on carers, stating that reduced visiting had proved traumatic in many cases, particularly were there had been bereavement, and was likely to be reflected in stress and decreased mental wellbeing for years to come among carers and their families.
93. Marie Curie also acknowledged that restrictions on visiting in care homes, while absolutely necessary to tackle the spread of COVID-19, had taken its toll on residents and their loved ones.
94. About two-thirds of care home staff who responded to the Committee's online questionnaire also agreed that restrictions on visiting had impacted negatively on residents' wellbeing, although some 45%, felt it was worth the negative impact, and the overall majority of care home staff respondents were either supportive, or very supportive, of the return of virtual visits if necessary. Almost 80% of responses from residents and family members stated that the residents' wellbeing had been negatively impacted by the virtual visits; 42% believed that the benefit of the impact was not worth it, although a slightly larger group were supportive of a return to virtual/drive-by visiting if necessary (45%).
95. During the Committee's informal, virtual meeting with the families of care home residents, it was evident that visiting was the most important issue of concern to those who took part. Without exception, relatives related their distress in having restricted access to their loved ones and many described a deterioration in their family members' psychological, emotional and physical wellbeing as a result of social distancing measures and limitations on visiting.
96. The family members described the various visiting regimes that they had experienced since March 2020. These included: blanket bans, virtual visiting, window visits, weekly half-hour socially distant visits, and monthly 15-minute visits. The relatives also related many examples of the difficulties presented by the visiting rules in place when they were allowed to visit. Some of these included: communication difficulties caused by the use of PPE and social distancing arrangements for relatives with poor sight and hearing difficulties; the distress caused to relatives and residents by not being allowed any physical contact; and losing a precious visiting opportunity if their relative was sleeping during an allocated visiting time.
97. The evidence provided by the families was echoed by the PCC in its written submission to the Committee. PCC advised the Committee that the nature of the concerns its office had received had changed over time: initially families expressed frustration and anxiety about not being able to visit their relatives, and after restrictions were eased in July, some people continued to experience difficulties in gaining visiting access, but more commonly contacts to the PCC were made by people unhappy with the measures that had been put in place to enable visits, the lack of flexibility in visiting arrangements, and poor communication from the care home. The PCC advised the Committee that across a large majority of the contacts and cases it had reviewed, there was significant concern for the short and long-term impacts of isolation on residents' emotional and physical wellbeing.
Dementia specific issues raised
98. The Alzheimer's Society advised the Committee that visits for people affected by dementia are critical, and that family visitors play a huge role in their care. It highlighted the important advocacy role that family carry out, including the timely detection of changes in residents' health.
99. The Society emphasised the devastating impact of social isolation for people with dementia and highlighted concerns that this may be contributing to a premature deterioration in individuals' dementia, stating that 'without family and friends able to visit, people's symptoms have worsened much more quickly and connections
to their loved ones, sadly even those who play a vital caring role, have been lost.' This view was shared by a number of the relatives who took part in the informal virtual meeting with the Committee.
100. The Public Health Agency (PHA) also advised the Committee that although the evidence is not completely clear, a lack of visitors may be a factor in shortening the life of residents, particularly those with Alzheimer's disease, and stated that confining residents to their rooms also reduces physical activity, which is associated with more rapid decline. The RCPsych also noted that the disruption of routines and reduced opportunities for visiting is reported to have had a negative effect on the mental wellbeing of many patients and carers and, while acknowledging that it is unclear if effects will be lasting, the RCPsych stated that in the case of dementia, a life-limiting condition, any harm is likely to be irrecoverable.
101. Age NI also emphasised the importance of social contact for people with dementia and supported calls for more compassionate guidelines for this vulnerable group. In its submission, the Independent Health and Care Providers (IHCP) also acknowledged the impact of restricted visiting, especially on those with dementia or learning disabilities.
102. The HSCB recognised there were particular difficulties in relation to caring for people with dementia/cognitive impairment, and who struggled to understand the rationale behind the reduction or ban on visiting, and advised that its Regional Dementia Lead distributed guidance on support to people with dementia during the pandemic. BASW also highlighted the particular challenges around caring for residents with dementia including challenges relating to maintaining social distancing.
Visiting policy
103. In June 2020, the DoH confirmed that visiting policy was a matter for each home but that guidance had been supplied in March recommending that homes minimise footfall. By the time official guidance was issued on the 26 April 2020 advising that visiting should cease, it had been widely reported that most care homes had taken that step already. Modifications to the guidance in May 2020 relaxed restrictions, allowing family, friends or loved ones to be facilitated to safely visit dying patients.
104. In briefings to the Committee, officials acknowledged the balance that had to be struck between maintaining family contact and protecting a vulnerable population. The Chief Medical Officer (CMO) told the Committee on 30 June that he was 'profoundly concerned about the impact that the restrictions have had on residents in care homes and, indeed, other supported living environments for individuals with, for example, a learning disability.' He also referred to the prolonged grief reaction that could affect family members who have not been able to see their relatives before they die.
105. Revised visiting guidance was issued with effect from 6 July 2020, relaxing restrictions with advice that care home managers should decide on appropriate policy given the particular circumstances in each home at any time. Care home managers were expected to develop a visiting policy taking account of the guidance and communicate it to residents, families and other visitors. The PHA developed risk assessment and supporting policy documents to assist care homes with the reintroduction of visitors to care homes and in support of the implementation of the guidance.
106. As infections began to rise again in September 2020, the CMO expressed the hope 'that we can avoid getting into a situation in which we impose a blanket ban on visiting, because that is hugely detrimental to residents, many of whom are in the last months of life, and to relatives. It is something that we should try to avoid at all costs while managing and mitigating the risks of infection.'
107. Revised guidance came into effect on 23 September 202013 advising that in the circumstances pertaining at that time ('medium surge'), each resident should be facilitated in having one face-to-face visit for one hour each week from one designated family member or friend, provided there was no outbreak at the home. The document recognised that a blanket ban on visiting was inconsistent with the European Convention on Human Rights (ECHR) Article 8 right to private and family life. The Care Home Sector Surge Plan published in September 202014 also recognised that even when limiting non-essential footfall in homes, 'some contact must still be face-to-face.'
108. The Minister's statement of 23 September 2020 acknowledged the additional need for compassionate arrangements to facilitate visits where patients were receiving end-of-life care and indicated that one-hour daily visits should continue in hospices.
109. While briefing the Committee on 1 October, the Minister confirmed that the one-hour, one visitor per week approach was being implemented under level 4 'medium surge' arrangements. The guidance makes provision for this to change in line with higher or lower surge levels and for more restrictive arrangements in homes where there is an outbreak of COVID-19, such that in-person visits would only be permitted in exceptional circumstances (e.g. for residents approaching end of life) subject to strict infection prevention and control (IPC) measures and PPE.
110. While the guidance recognised the right of next of kin and carers to visit their loved ones, given the dangers of COVID transmission, it also set out conditions including risk assessment and communication obligations if a departure from the guidance is proposed. Virtual visiting was recommended where possible and if effective. Nevertheless, managers remained the decision-makers, based on dynamic risk assessment at local level (i.e. responsive to changing circumstances), facilities available etc.
111. Responding to issues raised in connection with the role of families, the revised guidance stated: 'Residents and relatives should be involved in the development of care home policy, and in the decision-making regarding the risks and benefits in facilitating visiting' and goes on to advise that decisions should involve residents and/or their loved ones and reflect individual considerations of risks, benefits and risk tolerance.
112. The Trusts' responsibilities for its clients placed with private providers was also set out, in terms of seeking assurance of the implementation of visiting guidance.
113. Marie Curie confirmed that it supported the guidance on visiting as an important step to protect vulnerable patients and stop the spread of COVID-19 and the NI Hospice advised that it had worked with the Deputy Chief Nursing Officer (CNO) to influence the guidance, suggesting that patients and families determine and agree which two people should be allowed to visit for a maximum of one hour, one at a time.
114. COPNI and RCGP NI welcomed the Department's most recent guidance but advised that care homes would need extra support and resources to facilitate
safe visiting. BASW also welcomed the Minister's announcement that Health and Social Care (HSC) facilities allow one face to face contact, but advised that it considered this a minimum provision.
115. Age NI suggested that there should be some flexibility in the approach taken and that there was an opportunity for a judgement and compassion piece around designating perhaps more than one family member, and that one hour could perhaps be allocated as two half-hours.
116. In its submission to the Committee, the Alzheimer's Society stated that action must be taken to support the role of informal carers who support people living with dementia by: allowing for at least one informal carer per care home resident to be a designated key worker, with access to training, COVID-19 testing/ vaccinations and PPE; and where care homes are unable to facilitate visits from loved ones, requiring them to notify national care inspectorates and seek to put in place suitable alternative arrangements to maintain appropriate contact.
117. The Royal College of Nursing NI (RCN) described as 'not viable' the proposal that homes facilitate one, one-hour visit per week in addition to care partner arrangements being split between two other relatives during the week (see overleaf) and called for regionally agreed policy & guidance addressing these matters. UNISON & RCN questioned whether a suggestion of twice-weekly, shorter visits could lead to an increased risk of transmission. RCN advised that the evidence would need to be examined and that it would be difficult to make decisions in respect of all care homes given their different circumstances.
118. The relatives of care home residents who met informally with the Committee expressed their concern that that visiting rules were not applied consistently across homes with one relative describing provision as a 'postcode lottery' and there were requests for a more consistent and uniform approach across the sector. Inconsistency in the application of the guidance, particularly in the independent sector, was also highlighted in the evidence from BASW and the Trusts and in the informal meeting with the families of care home residents.
119. A number of the submissions received by the Committee emphasised the need to provide appropriate support for residents and families at the end stages of life. Marie Cure emphasised the importance of palliative support for residents, to help address the emotional and mental health impact of being unable to see their loved ones as often as they would like, and bereavement support for the loved ones of care home residents, to help address any complex grief reactions arising from lack of opportunities to visit and say proper goodbyes. The Trusts also acknowledged the importance of visits at end of life stage and a number of relatives expressed their view that there should be exemptions to visiting restrictions for residents who are receiving palliative care.
120. The HSCB advised that, at all times, priority was given to ensuring that people nearing or at the end of life were supported by visits from their families, wherever possible, and confirmed that most homes were able to support families to visit, albeit in a restricted way at this very sensitive time.
Care Partners
121. The Department of Health's revised guidance on visiting, effective from 23 September 2020, introduced reference to 'care partners'. Care partners were described, in the guidance, as 'more than visitors. Care partners will have previously played a role in supporting and attending to their relative's physical and mental health, and/or provided specific support and assistance to ensure that communication or other health and social care needs are met due to a pre- existing condition. Without this input a resident is likely to experience significant and/or continued distress.'
122. The Department advised the Committee that care homes were asked to identify residents who might benefit from such arrangements and set out in their policies how the care partner arrangements would be agreed and facilitated with individual care partners in terms of the role and frequency /duration of visits. Up to two people per resident could take on the role, with one attending at a time.
123. Responding to criticism of a lack of engagement prior to announcing the care partner initiative, the CNO said engagement with care homes and families was ongoing to support care homes to facilitate it, that it was 'the right thing to do' and that she hoped the additional funding announced would help to address some of the difficulties highlighted.
124. There was general support for the care partner idea in the submissions considered by the Committee, however, support was frequently caveated with caution regarding the increased footfall in homes that this initiative would produce. The representatives of the care home sector advised the Committee that they had not been consulted by the Department on the care partner idea before publication of the guidance.
125. The 'care partner' role was generally welcomed by the relatives of care home residents that took part in the virtual meeting with Committee Members, however, there was a belief that there was reluctance on the part of the care homes to apply the new policy and some relatives expressed concern that there was no monitoring of implementation. Some family members felt the Department's guidance was aspirational and lacked clarity.
126. The families expressed their view that they should not be seen as 'visitors' as they provided a key role in providing care and support to their relatives who resided in care homes. Some relatives requested that one or two relatives of care home residents should be given 'key worker' status and others advocated for the implementation of the 'care partner' role. There was general acknowledgement that visiting should be conducted safely with infection control measures and testing in place. There was also acknowledgement that not all families wanted the same thing and one relative expressed concern about the risk that an increase in footfall in the care home would present.
127. BASW also supported the care partner concept, advising this would be an important role in maintaining a relative's physical and mental health. BASW concurred with the Department of Health's position that without this input, a resident was likely to experience significant and/or continued distress.
128. COPNI stated that while the care partner idea was good, much of the support role described was provided by families before the pandemic. COPNI was concerned that the care partner role would be difficult to introduce to any high degree because of the scale and threat of the pandemic and the amount of work involved.
129. There was acknowledgement across the Trusts of the concerns of providers about increased footfall. The Belfast Trust hoped that the care partner initiative would address the issue of inconsistency in practice regarding visiting across the care home sector, while the Western Trust recommended engagement and clarity with providers, with a tailored assessment implementation, rather than a blanket approach.
130. IHCP, RCN and UNISON advised the Committee that the care partner initiative had been announced without prior engagement with the sector. RCN and UNISON outlined concerns in relation to testing, insurance, liability, training, safeguarding, and the need for clarity about the role and criteria for designation. The unions also questioned whether there was an intention to use the initiative as a mechanism to address staff shortages.
131. In its written submission, the IHCP advised the Committee that the recent visiting guidance had caused concern particularly against a backdrop of the worrying increase in community transmission. It advised that there were many problems which were not foreseen, not least insurance and regulatory requirements. The IHCP told the Committee that it had flagged the issues that needed to be addressed in order to mitigate the risk of the increased footfall, including an increase in the frequency of testing and timely results and appropriate funding support and recognition for staff. Until these issues were addressed, IHCP advised that the care partner role was unlikely to be assessed as appropriate.
132. However, briefing the Committee in the early stage of the pandemic, on 19 March, IHCP had highlighted the risk of inadequate care due to staff shortages and ill-health, and stated that 'the bold decisions to be taken are around relaxation of regulations and the AccessNI basic checks. It is a matter of weighing up the risk of whether someone is going to be provided care against whether we can bring in a family member who has not had a basic check but is someone whom we know.'
Innovation including the use of technology
133. The Department's Rapid Learning Initiative (RLI), which reported in September 2020, acknowledged the strength of feeling across responses from residents, families, care home staff and managers, about the importance for residents and families of maintaining contact with each other. Consistent with the evidence heard by Committee, the Department found that the availability and success of virtual visiting had been patchy due to limited technology and suitability of this approach.
134. The DoH had announced an £11.7 million funding package on 2 June 2020, including £2.2 million for equipment which could be used to purchase devices to facilitate virtual visiting. The PHA assisted with the process to scope the need for tablet devices that were subsequently made available to care homes to support virtual visiting.
135. The HSCB advised the Committee that individual providers introduced local initiatives (dedicated visiting areas, visiting times, use of technology and regular telephone contact with families) which, while never substituting for direct contact with loved ones, went some way to reassuring families about the wellbeing of their loved one living in the care home. HSCB advised that the use of technology and localised initiatives within homes appeared to work well, but the long-term impact had yet to be seen. It stated that there was a need for regional discussion on the use of technology and a requirement for investment in equipment and a major training programme for staff and the general public.
136. The Trusts advised the Committee that they had also supported a number of approaches to ensure meaningful visits, including the use of technology for virtual visits, window/drive-through, and outside pods. Positive Futures stated that the use of technology had been vital in enabling the people it supported to maintain connections with their loved ones and vice-versa.
137. When briefing the Committee in May, IHCP advised the Committee that lots of methods and arrangements could be put in place and that there was a need for innovation. In later written briefing, IHCP confirmed that there had been a range of innovative ideas to assist with family visiting which include video, zoom calls, garden visiting and visiting pods. However, it pointed out that moving into colder weather would impact on the outdoor visiting solutions.
138. Age NI welcomed the focus on how technology could reduce levels of loneliness but was concerned that it would not be appropriate for all older people. This concern was shared by the family members who met with Committee Members, and Marie Curie, who highlighted that the high prevalence of neurodegenerative conditions, such as dementia, meant that the use of digital technology for contact was not always viable.
139. The RCPsych noted that technological solutions, such as video calls, were not comprehensively introduced in all care homes and there had been major inequities in approach. Moreover, extra consideration needed to be given to how to help families communicate with those with sensory or cognitive difficulties. RCPsych stated that the urgent development of infrastructure (e.g. Wi-Fi coverage) in some homes also required consideration. The RCPsych proposed that care homes be required and supported to provide daily telephone and video updates and visits, and that these should become the norm.
140. In its written submission to the Committee, the PCC highlighted examples of some of the difficulties families had experienced in relation to virtual visiting. It observed that there appeared to have been little thought about the complexities of communication, especially with elderly and sometimes cognitively limited people; and the restrictions as a result of poor Wi-Fi or internet connectivity. PCC suggested that whilst there has been financial investment by the Department of Health into these resources, assurances and accountability regarding the quality of the experience needed to be at the fore.
141. RCN outlined the additional burden on staff due to virtual visiting, since staff had to organise it and, often, remain present throughout. Again, RCN maintained there was a lack of engagement prior to public announcement and a degree of unmet expectation and damage to relationships between homes and families as a result.
142. A number of contributors including the Trusts, Age NI and the PCC, suggested that efforts should be made to identify and share good practice. AGE NI asked for a fact-finding exercise to be carried out that would identify effective innovation as well as the cost and practicalities of extending these, and BASW called for the family liaison service provided in the Northern Trust to be adopted by all of the Trusts.
143. The PCC recommended that care home providers should develop innovative visiting arrangements in collaboration with residents and their families which adhere to guidelines but which strike a balance between protecting staff and residents from COVID-19 and maintaining residents' quality of life and wellbeing. Such steps could ideally be tailored to individual residents, and were especially important for residents living with dementia or approaching their end of life.
Communication on visiting
144. The importance of good communication and engagement was a recurrent theme within the evidence considered by the Committee in relation to visiting. A number of the relatives of care home residents who spoke to the Committee described their frustration regarding the lack of communication from their relatives' care homes. IHCP, RCN and UNISON expressed their disappointment about the Department's lack of consultation and engagement with representatives of the care home sector in the development of policy and guidance, as referred to earlier in this section.
145. In its submission to the Committee, the PHA described efforts to capture the experience of residents, relatives and staff through its Lived Experience Project and advised that the key messages captured had been central to the 'Rapid Learning Initiative in Transmission of COVID-19 in Care Homes' and has informed the Surge plan for Care Homes. PHA advised that a key area of learning was the importance of developing open and transparent conversation between the residents, relatives, providers and decision-makers.
146. The PHA advised the Committee that it was working towards implementation of an online user feedback system to promote continuous feedback in the care home sector. Also, in collaboration with the PCC, the PHA was developing a system for residents and relatives and of Care Home to provide feedback on a regular basis on key topics, such as visiting.
147. In its written submission to the Committee, the PCC recommended the replacement of top-down decision-making on visiting restrictions with a creative ongoing engagement strategy, so that the perspectives of residents and their families are central in planning visiting arrangements which are safe, humane and acceptable to all stakeholders. PCC felt this would help to address the feelings of 'powerlessness' expressed by family members.
148. This view as supported by Age NI who reminded the Committee, in its written submission, that each care facility was the home of the residents who live there and that those residents and their families should be involved in decisions that affect them and their home life. On this issue, PCC suggested that care home providers should create and sustain ongoing regular engagement and communication with residents and families, by:
- providing information on the rationale for changes to visiting arrangements so that residents and their families can understand decisions;
- giving family members regular updates about each resident during periods of restricted visiting or contact, including information on health status, but also qualitative updates on how the resident is coping; and
- regularly updating residents and family members about the incidence and spread of COVID-19 within their care home.
149. PCC also referenced the need for clear communication regarding the status of 'guidance' which is advisory only for independent sector care homes. It was PCC's view that this may reduce confusion and frustration around the inconsistency in visiting arrangements between sectors, and between care homes.
150. PCC also asked that the rationale for decisions be provided so that care home providers, residents and their families can understand policy decisions. This view was supported by Marie Curie and a number of the Trusts. The Western Trust suggested that greater clarity and direction was needed, especially when the R rate increases, and homes are in outbreak status.
151. PCC also stated that steps to increase consistency in how care homes interpret, implement and adhere to visiting advice, would be welcome and advised that this could be achieved through more proactive communication and engagement with providers at the point of issuing guidance.
Testing
152. Concerns about the adequacy and efficacy of testing policy were raised by many representative bodies and organisations. Issues cited included concerns with capacity, the impact on a strained workforce and stretched financial resources – issues which pre-date the pandemic. Other challenges included frequency of testing, symptom monitoring and maintaining human rights and the dignity of residents, especially in obtaining consent from those with cognitive decline.
153. A recurring theme throughout evidence sessions, especially in the early months of the pandemic, was that limited capacity impacted on the ability of testing to be delivered effectively in the first wave of the pandemic. In particular, the Committee heard that the ability to make use of testing to best effect had been hampered by practical difficulties on the ground. COPNI said that care homes had reported delays of between four and eight days in the turnaround of tests and the Alzheimer's Society was unhappy with the length of time taken for couriers to collect tests and deliver results. The IHCP concurred with these views, and also made reference to issues with the IT system.
154. Concerns around testing capacity were also reflected in evidence presented by a number of the HSC Trusts who reported on delays in obtaining results from the National Testing Programme and flagged instances where positive results were not separated from negative results. NIC ICTU stated that test results were slower to be returned for staff in care homes compared with staff in Trusts, however, it noted that the situation had improved since the spring.
155. Describing the impact of such delays, BASW stated that given the significant pressure that social work was already facing, it could not afford to have staff self- isolating for longer than was necessary and described an example of a staff member who was unavailable for four days whilst waiting for what was then a negative result.
156. The Committee heard from the Minister and officials on a number of occasions before and during the inquiry on this issue. On 19 March, a written ministerial statement advised that HSC laboratories had increased their capacity five-fold from the start of the pandemic when 40 tests per day could be processed, to over 200 tests per day. In subsequent briefing to the Committee on 2 April, the Minister referred to the ongoing challenge of scaling-up testing and advised that the first priority was to test those admitted to hospital with COVID-type symptoms, the second being those in secured or cohorted living, including residential and nursing homes.
157. When briefing the Committee on 16 April, the PHA advised that it had scaled testing up from an initial approach of testing five residents in homes with two or more positive cases, to testing everyone in homes where there was an outbreak.
158. A week later, the Minister advised the Committee that capacity had increased to 1,700 tests per day and, as a consequence, testing was widened to include key workers; also work was ongoing to make use of MOT facilities and the SSE Arena as testing sites, under 'Pillar 2', the UK Government's national testing programme15. This was followed by a formal announcement by the Minister on 27 April, extending testing in care homes to all staff and residents when a home was identified as having a potential outbreak, rather than the previous approach of testing staff and residents who displayed symptoms.
159. The HSCB confirmed to the Committee that from 11 May, testing of all staff and residents in care homes had begun, with the support of NI Ambulance Service staff. The CMO updated the Committee on 30 June that the final two homes were to complete testing that day. Regional guidance was agreed and issued in respect of care home providers and continues to be kept under regular review.
160. However, a number of representative bodies and organisations set out their concerns about the timeliness of the roll-out of the testing regime. The IHCP welcomed the rolling programme of testing, but voiced concern that homes were in outbreak before either an initial test, or repeat positive tests, confirmed that (an outbreak is two symptomatic cases). Furthermore, the IHCP considered that allocation of care home staff to 'Pillar 2' accounted for a slower turnaround in tests.
161. UNISON concurred with this view, reporting that its members believed the introduction of testing into care homes occurred too slowly and incrementally. Also, UNISON reported on 'residents having contracted COVID-19 in May, but staff not being tested until June, contrary to the regional policy.'
162. The Alzheimer's Society drew attention to regular testing for staff and residents not being announced by the PHA until 3 August, by which time figures for deaths demonstrated a high proportion amongst care home residents.
163. The frequency of the care home testing programme was also a focus of discussion. The CMO advised the Committee on 20 May that a rolling programme had been agreed in principle but that the frequency was still to be determined.
164. When briefing the Committee on 4 June, COPNI suggested that two weeks between tests would be too long and proposed twice weekly tests for staff and residents. In their written submissions to the Committee, IHCP advocated that testing should be carried out on a weekly basis for staff and every two weeks for residents while Age NI called for testing to be reviewed as a matter of urgency in light of the increase in community transmission. COPNI also advised the Committee it had written to Health Minister on the matter.
165. Returning to the Committee on 3 September, the CMO advised that the frequency of repeat testing was being kept under review and explained the process under way, 'We use pillar 1, as opposed to pillar 2, for care homes where there are active outbreaks, but...we are now seeing the active case-finding as a result of the testing programme... If we see two or more positive results, we test everybody: residents and staff. We then test at day four, to, day seven, to make sure that we get on top of the outbreak. Again, that is everybody. Once the outbreak is confirmed as closed at day 14, we go back at day 28 and re-test everyone, just to be absolutely certain that we have closed down the outbreak efficiently and effectively.'
166. In oral evidence on 22 October, the CNO updated the Committee that testing through Pillar 1 was providing results usually within 24 hours whereas testing through Pillar 2 was being used for the regular testing programme and the care sector had complained in relation to turnaround times for results, but noted 85% of results were coming back within 72 hours.
167. On 3 November, the Health Minister announced his intention to increase the frequency of COVID-19 testing for staff working in care homes from once every two weeks to once a week.
168. The Committee heard throughout the course of the inquiry concerns regarding pressure on resources, including staffing. Collectively, the Trusts reported that they considered the testing programme to be both challenging and resource intensive and that as more homes experienced outbreaks this put further pressure on Trust staff. The RCN said the testing regime had been introduced without prior engagement, with little opportunity to prepare, and without additional funding. In further evidence, the IHCP reported to the Committee that feedback from their providers indicated that Trusts were experiencing capacity difficulties to complete repeat testing at day four to seven, due to resourcing issues, with a subsequent delay in the identification of positive cases.
169. In oral evidence to the Committee, the RCN described the testing regime as 'unsustainable', referring to the increased staff time and administrative burden entailed; and said a move to weekly testing would exacerbate current challenges. Added to that, RCN highlighted that some nurses were having to use their own time to travel for up to an hour to undertake a test, a situation it considered unacceptable.
170. Concern about staff training was a related concern. The IHCP reported a mixed approach in terms of some support offered by Trust nurses and some online training, to enable testing to be done by care home staff, but concluded that continuing support from NIAS and trained HSC nurses would be preferred. The Trusts noted that training has to be undertaken regularly to ensure skills remain effective, and that any turnover of staff, which can often be high, necessitates training to be repeated. Furthermore, the IHCP said there were risks associated with non-medical staff undertaking testing provision. Positive Futures concurred with this view.
171. With regard to symptom monitoring, the Trusts outlined how they had implemented such arrangements e.g. re-deploying staff; bringing mobile testing to homes; implementing rapid community response teams, to assist care homes with the daily recording of residents' symptoms by using the PHA Regional Care Home Monitoring Matrix; and providing clinical support and escalation as required.
172. The PHA advised that, as it learned more about COVID-19, the revised case definition was expanded to alert clinicians and care homes to the need for a higher index of suspicion regarding possible atypical COVID-19 presentations particular to older people. Subsequently, the PHA amended the COVID-19 guidance for care homes in response to the change in definitions, advising care home to treat all residents with atypical symptoms as probable COVID-19 positive and to manage these situations as potential COVID-19 outbreaks. Care home staff are supported in this process with information on a dedicated PHA website page.
173. The RCN advised, that in line with current guidance, staff report twice daily on temperature checks in respect of all staff and patients. Staff are also required to monitor twice daily the SAO2 (oxygen saturation) levels of patients. This was flagged as an additional burden on staff.
174. In September, the RLI undertaken by the Department of Health, reported findings of inadequate clinical equipment in 37% of homes and concluded that 'access to and training in the use of the required clinical equipment for monitoring of resident symptoms in particular within residential settings is vital.'
175. The NI Assembly research paper, included at Appendix 4, referred to the European Centre for Disease Prevention and Control (ECDC) advice that key to preventing and controlling outbreaks of COVID-19, is systematic monitoring of all residents and staff at a Long-term Care Facilities. ECDC advised, for example:
- Measurement of temperature, oxygen saturation, and respiratory rate at least once a day, or once every shift, to identify cases as early as possible and initiate testing.
- Patient records should be updated daily with this information; and whether a patient has received a COVID test; has been isolated due to COVID compatible symptoms; and /or required any other non-standard infection prevention and control (IPC) measures.
- Responsibility for this active monitoring must sit with an appointed, named staff member.
176. Furthermore, organisations and representative bodies raised the growing risk posed by asymptomatic cases (in which symptoms are not apparent), and which became increasingly evident as the pandemic progressed. In September, the Minister acknowledged that testing was revealing a high percentage of such cases.
177. As referenced in the Assembly research paper, testing programmes were expanded in care homes in other countries as the pandemic spread:
- In Denmark testing of all care home residents, regardless of symptoms, began on 27 April, 2020.
- Denmark and the Czech Republic initiated repeat testing for asymptomatic staff, or those with a negative test, at regular intervals (7-14 days).
- In the Republic of Ireland staff are required to have their temperatures measured twice a day.
- In Germany the recommendation is for at least daily documentation of clinical symptoms among both residents and staff.
- In Malta swabbing of healthcare professionals is mandatory prior to assuming duties within care homes.
178. Professor Ben Cowling, Head of Epidemiology and Biostatistics at the University of Hong Kong acknowledged that Northern Ireland had a testing programme in place at the start of the pandemic, noting the importance of such an approach to identify outbreaks and initiate intervention. Professor Cowling briefed the Committee on his current research into regular testing and suggested that Northern Ireland may wish to give consideration to pooled testing to derive greater benefit from existing capacity.16
179. A number of respondents, including the IHCP, highlighted the risks associated with increased footfall into care homes by other professionals and considered that this should fall within the routine testing protocol. Meanwhile, BASW called for social workers to be included in the testing programme to ensure continued access to care homes.
180. In its written evidence provided in October, the PCC wrote that testing is only as effective as the coverage it provided across settings. With the current challenges in the HSC workforce and in the care home sector, including the transience of staff across settings; the use of agency staff across services; and the ongoing regulation regime implemented by the RQIA, which necessitates visits into care homes by RQIA inspectors, routine testing of individuals on exit and entry to services is critical in minimising infection and spread of COVID-19.
181. The issue of residents' rights with regard to giving consent to testing, resonated throughout evidence brought to the Committee and was of significant concern. In oral evidence, RCN referred to challenges around consent, particularly in respect of those with cognitive difficulties. The RCPsych raised the potential trauma of applying swabs to residents with cognitive difficulties. Age NI stressed that consent had to be obtained correctly and that staff must be comfortable delivering tests.
182. HSCB reported to the Committee that the impact of the testing process in respecting the human rights and dignity of residents was an important point of discussion and debate that surfaced in its engagement with stakeholders. This included the ethical burden placed upon staff to determine the right of the individual's freedom of choice versus the right to safety in group settings.
183. The Committee wrote to the Northern Ireland Human Rights Commission (NIHRC) on this matter, which responded, indicating that the procedure engaged a number of human rights, but that not testing also engaged human rights. NIHRC articulated the balance of competing rights required, taking into account the seriousness of the disease, advising: 'Consideration should be given to ensuring the testing is no more obtrusive than necessary and that where possible individuals fully understand what is going to happen and why. The UN CRPD is also clear that reasonable accommodation should be made to ensure equal enjoyment of these rights (Article 5(3)). This requires consideration of what measures can be taken to ensure that the effect of the test is alleviated, particularly for those with a pre-condition that will only add to the stress of an already unpleasant procedure' and that 'arrangements for involving individuals and, where appropriate family members, should be taken to ensure assent wherever possible.'
184. The South Eastern Trust advised that it had encountered some resistance from residents and staff in relation to testing and had shared legal advice in relation to health and safety guidance. In conjunction with this, key workers reiterated messages to reinforce the importance of participation in testing for residents' benefit. Other Trusts reported the same concerns and had responded with a similar approach.
185. The IHCP reported that not all residents agreed to being tested and consequently had requested from the PHA, details of what monitoring system was in place to quantify the numbers of those untested. At the time of giving evidence to the Committee on this point, the IHCP advised it was awaiting a response.
186. The PCC advised that it had written to the CMO on the matter of consent. In referring to his response, the PCC said they had been advised that where residents had capacity, consent should be obtained, but a refusal must be respected. With regard to where residents did not have capacity, a care home must follow the process for a 'best interest' decision.
187. As part of the inquiry, the Committee sought the views, via an online survey, of owners/ managers, staff and residents/ family members into the impact of COVID-19 on care homes. Almost all residents and staff who responded to the survey stated they were being regularly tested for COVID-19, with consent sought. Furthermore, the majority of staff indicated that there was ongoing symptom-checking in their home, with almost two-thirds confirming that this was undertaken twice daily. More than three-quarters of respondents acknowledged that they understood the need/ reason for the testing taking place.
Discharge Policy
188. Concerns were raised repeatedly by representative bodies and social care professionals as to the effectiveness of hospital discharge policy, in mitigating the risk of infection being introduced into care homes by potentially COVID-19 positive patients.
189. As referenced in the NI Assembly research paper (at Appendix 4), most countries were prescriptive in relation to the minimum quarantine requirements for residents discharged from hospital back into care home settings. The paper stated that there was increasing recognition of the danger of discharging people directly from hospital into care homes without ideally two negative tests within 24 hours (due to the risk of false negative tests), even in the case of those not originally hospitalised for COVID-19. During the course of the inquiry, the Committee heard of practice in other countries, including Hong Kong. As referenced in the research paper:
'In Hong Kong any confirmed cases were quarantined for up to three months; those in close contact were in a separate quarantine centre for two weeks undergoing regular testing. All nursing homes had a trained infection controller involving training in simulated outbreaks so as to become a well-worn practice.'
190. As part of its inquiry, the Committee held an evidence session with a panel of academic experts. Professor Martin McKee,17 advised the Committee that as a result of capacity issues in hospitals, 'people were being taken out of hospital and put into care homes, feeding the infection there, and, more broadly, in the community at a time when the testing regime was not well established.' Professor McKee advised that older people were more vulnerable and many were in settings at particular risk of institutional amplification.
191. Reference was made specifically to guidelines in the Department of Health's discharge policy for patients to have had 'ideally' a COVID-19 test 48 hours beforehand, unless that home was the patient's previous residence. The Committee noted media reports18 that Trusts had received a letter from the Department of Health Permanent Secretary on 25 April 2020, requiring that hospitals continue to discharge 'COVID-positive' patients to care homes so long as they could be isolated there and; that Trusts should identify alternative accommodation for those where isolation cannot be provided.' The Permanent Secretary's letter reportedly stressed that prior testing 'must not hold up a timely discharge.'
192. In September the guidance19, was updated and made clear that homes may need to accept individuals with COVID-19 although it stated 'ideally, patients who are COVID positive or symptomatic, should not be discharged to a care home that has no symptomatic or COVID positive residents, unless that home was the patient's previous residence.' It also stated that discharge should not take place to the small minority of care homes that cannot provide isolation facilities for the resident on arrival.
193. In written correspondence of 17 November to the Committee, the Minister advised that the Permanent Secretary's correspondence dated 25 April set out testing arrangements at that time. It explained that the rationale for introducing arrangements for patients to be tested for COVID-19, 48 hours in advance of discharge from a home was to support providers and staff in the receiving care home to understand each resident's COVID-19 status, and to enable care homes to effectively plan for each resident's care needs.
194. Prior to this, on 12 November, the Health Minister welcomed the publication of a research study20 commissioned by the Department of Health and conducted by Dr Niall Herity, a consultant cardiologist at the Belfast Trust. In the statement issued by the Department on 12 November, it advised that the research looked at data for discharges, as well as considering if there was any correlation between discharges from hospitals and infection rates in care homes. The work could not identify any such correlation. In reference to the findings in the study, it noted that through the first surge of the COVID-19 pandemic, front-line clinical teams had more unoccupied beds available to them than usual, reflecting reduced attendances at emergency departments and reduced hospital admissions. Hence, there was less pressure to accelerate patients' discharge from hospital than is normally the case, other than to minimise the well-known risks associated with being in hospital.
195. The Department of Health's Chief Social Worker (CSW), advised that discharge was a clinical decision, made by a clinician knowing the setting to which a patient would be discharged. The CSW also emphasised that no-one should be in hospital any longer than necessary, referring to the decline in mobility seen, particularly in older or more frail patients, in hospital settings and the risk of hospital-acquired infection. Acknowledging concerns early in the pandemic about the risk of acute hospitals being overwhelmed, the CSW stated that the guidance issued on discharge made it absolutely clear that people should be discharged to care homes only where a care home could adequately manage the care of that patient, including capacity to provide barrier nursing. In its evidence, the RCN advised that it is extremely difficult to isolate patients within a care home because the environment and design will generally not facilitate this.
196. Whilst the introduction of a discharge policy was welcomed, UNISON raised concern that guidance was not available until the end of April. However, there was universal concern amongst representative bodies as to how promptly results were made available for those transferring from hospital to a care home in order to confirm whether a COVID-19 test was positive or negative before discharge; also in regard to a lack of a consistent policy on follow-up testing to identify the origin of a subsequent infection presenting in a care home i.e. to establish if had been contracted whilst in hospital.
197. Earlier in the pandemic the IHCP said testing had not been undertaken highlighting the risks inherent in 'bringing people from hospital who have not been tested into an environment where people are very weak and vulnerable.' In further evidence, the IHCP stated that not all Trusts had discharge pathways to accommodate those who had tested positive and either continued to test positive, or were medically fit for discharge, but remained in the infective period. As expressed by IHCP, there was therefore 'no safety net' for re-testing residents discharged after four to seven days. The IHCP advised further that as tests are not always available on discharge, care homes isolate all new residents for a period of 14 days.
198. The NI Hospice informed the Committee that it had asked referring units to undertake COVID-19 testing of patients prior to discharge to its facilities but as this was not always completed, the Hospice took the decision to swab all its patients on admission.
199. The RCN considered that discharge policy had been more easily implemented in the first wave as numbers were fewer but expressed concern about the possibility of homes being put under pressure to admit COVID-positive patients if Trusts faced bed shortages due to rising numbers of infections.
200. A palpable sense of pressure to admit patients who may have been COVID- positive was conveyed to the Committee by a number of respondents, including the IHCP. COPNI advised that it had recorded in its contacts with families that new residents had been moved into their relatives' care home at the start of the pandemic with no assurance of their COVID-19 status. COPNI was of the view that no patients should be discharged from hospital unless a negative result was obtained. RCN supported this position, saying that patients should only be discharged from hospital if they had tested COVID-19 negative. In its evidence, the RCGP concurred, saying that neither new residents, nor those discharged from hospital, should enter a care home unless they receive a negative test result.
201. Furthermore, Age NI said that it believes there should be more clarity around arrangements on testing prior to and post discharge from hospital settings, including in situations where an older person has, for example, attended an Emergency Department, but not been admitted to hospital, and then returned to their care home.
202. The PHA stipulated that guidance was developed to ensure the same conditions applied to people admitted to care homes from community settings as applied to people discharged from hospital to a care home. The PHA further described the support it provided to care homes making reference to regional guidance for nursing and residential care homes, which assists staff to identify when it may be appropriate to move someone to a different home or facility as well as reference to infection prevention and control (IPC) measures. In addition, the PHA advised that the care home sector is signposted to support and advice from their local HSC Trust and the RQIA.
203. In evidence submitted by the HSC Trusts, they advised they had worked in line with regional guidance to swab all patients 48 hours prior to discharge.
204. Trusts also communicated their concerns around the challenges presented by the 14-day isolation requirement. For instance, care homes were under greater staff pressures to provide more one-to-one care, especially to support those with dementia. In a similar vein, the RCN described the difficulties isolation poses, particularly if an individual has cognitive impairment, and pointed out also the deprivation of liberty issue arising in these situations. The impact on mental health and wellbeing was a key concern, with respondents underscoring that care homes were residents' actual homes.
205. Age NI took the position that 'decanting' care home residents to a designated facility, in the case of an outbreak, should only be considered as an option of last resort.
206. The pressure on acute care in hospitals was widely recognised and several organisations suggested consideration of a safe process for discharge with options available to support this, such as step-down facilities. The HSC Trusts outlined to the Committee arrangements put in place due to the pressures brought by the pandemic early on. Accommodation such as the Ramada Hotel was deployed initially, though with experience it was deemed that the management of infection prevention and control was more effective through a COVID-19 positive discharge pathway.
207. Examples were also given of bespoke COVID-19 positive discharge units in Northfield Residential Care home (a Trust managed residential home), Rosevale Nursing Home and Rainbow Unit (both independent sector facilities) with a total of 55 beds. These facilitated discharge from acute beds; admission from the community to prevent hospital admission; transfer of COVID-19 positive residents from another care home to prevent spread in that care home; or where care needs were such that hospital admission was not required, but were above what could be managed by the home at a time of crisis.
208. BASW considers there was a clear need for increased provision of step-down discharge hubs where patients could stay prior to returning to their care home, to minimise the risk of transmission of COVID-19. Nevertheless, BASW stressed that it was vital that social workers be provided with access to service users in any such step-down care facilities, to ensure the correct identification of assessments and that appropriate support services are put in place. BASW recognised the initial need to focus on acute care, but was concerned that there was insufficient attention on the discharge pathway for older people leaving hospital.
209. The RCPsych acknowledged that greater availability of interim and step-down placements, in general, may be helpful in improving hospital bed-flow but rapid patient moves from the acute to the care home sector, though necessary, were likely to have been distressing and to have carried some increased risk of mental and physical harm. The Patient Client Council reported that the negative impact in particular on people living with dementia, of moving into and out of care homes was raised by several of its clients.
210. The HSCB acknowledged that the usual actions undertaken on discharge had to be temporarily modified, such as the standard of care home close liaison with families and with the patient. This meant, in practice, that patients were discharged to the first available suitable bed; and, due to infection control measures, families were not able to visit in advance.
211. The CSW recognised that the infectiousness of coronavirus was not fully understood early on. The PHA advised that prior to April 2020, asymptomatic testing was not done. The RLI initiated by the Minister and led by the Department of Health, recognised the potential for asymptomatic patients to infect others and the PHA then facilitated retrospective whole-home testing in homes which had outbreaks prior to 24 April. The PHA also led on updated guidance on management of outbreaks in care homes, issued May 2020, that utilised the National Testing Programme to support a rolling programme for care home testing.
212. On 2 September, the Minister announced that Whiteabbey Hospital would become a second Nightingale Hospital and operate a 100-bed step-down facility. The next day he confirmed to the Committee that this would be for step-down from acute and social settings, though at this point it remains unclear whether this can be used where homes lack facilities to isolate residents returning from hospital.
213. The Rapid Learning Initiative report, led by the Department of Health, catalogued a range of concerns the Committee had also heard about including the difficulty in isolating residents due to the physical constraints of certain homes and staff ratios. It also highlighted the impact on residents' mental health and the particular challenges where residents had cognitive impairment.
214. As part of the inquiry, the Committee sought the views, via an online survey, of owners/ managers (employers), staff and residents/ family members into the impact of COVID-19 on care homes. Almost three-quarters of homes responding said they have continued to admit new residents since the start of the pandemic. Survey results also indicate an overall majority of residents discharged from hospital to a care home during that period were tested for COVID-19 prior to release, with almost half of homes insisting upon a further test upon admission to the care home. A significant majority of care homes isolated residents in private rooms upon discharge from hospital.
215. In October, the CSW advised the Committee that discharge policy would remain under review.
Access to Personal Protective Equipment
216. There was general consensus amongst the representative bodies and social care professionals with regard to the early difficulties that social care providers experienced in accessing personal protective equipment (PPE), with supplies prioritised for the Health and Social Care system.
217. Written evidence from both the IHCP and the BASW indicated that there was a lack of strategic leadership, communication and support by the HSC Trusts at the outset of the pandemic.
218. The IHCP documented that care home staff had been 'left feeling vulnerable' when observing the difference in the level of PPE provided to HSC staff. One worker referred to ambulance staff coming into homes 'kitted out like they were going to the moon', which exacerbated the feeling of exposure by care home staff.
219. Following a meeting between officials and the independent home care sector, on 23 March 2020, the Health Minister said he had heard 'loud and clear' the concerns across the HSC sector in relation to PPE and was taking concrete action to address supply issues.
220. It also became apparent to the HSCB that the independent sector required additional PPE and to be actively supported and closely monitored with regards to the availability of PPE.
221. The PHA, in consultation with the HSCB, addressed the PPE challenge by developing the COVID-19 Regional Surge Plan for the NI Care Home Sector (with a distinct section on PPE) in May 2020, which was subsequently updated frequently to reflect the changing needs of the sector.
222. This plan required HSC Trusts to co-ordinate and manage the supply of PPE to care homes within their geographical area, thus promoting security of supply.
223. In developing the September 2020 surge plan, consideration was given to recommendations from the RLI to establish a sustainable mechanism for supporting the supply of PPE to care homes in a pandemic.
224. Regional surge plans were supported by agreed metrics. Monitoring templates asked for feedback from care homes and Trusts with regard to existing supplies and delivery and sought a self-reported 'RAG'21 rating. Initially, a weekly return of the metric was requested and has been kept under review, with timelines changed to reflect changing need.
225. Whilst the HSCB and the PHA acknowledged that a regional process was challenging to embed, they considered that the system worked well, due to: frequent communication; different categories of need being considered; a standardised response to supply of PPE; review by key stakeholders; a multi- agency approach; and a change to work schedules, to support care homes in all areas.
226. NIC ICTU also acknowledged that 'eventually (and this happened with a great deal of support from us) the public sector was able to wrap its arms around the independent care sector, for both domiciliary care provision and nursing-home provision.'
227. The Alzheimer's Society, IHCP, Positive Futures and BASW all acknowledged the initial short supply but recognised that there were now systems and structures in place across all of the HSC Trusts, in relation to the sufficient provision of PPE.
228. All HSC Trusts now comply with regional guidance and have mechanisms in place to supply PPE free of charge. These mechanisms include: partner hubs (Northern Trust); designated senior PPE leads for domiciliary care and care homes ISPs (Southern HSC Trust); and named/ identified member of staff (Belfast, South Eastern and Western HSC Trusts). In addition, they have a single point of contact in the Trust for providers to address PPE concerns.
229. The Trusts have arrangements for modelling of PPE requirements in each home, with minimum/ baseline requirements used to inform the Business Services Organisation's (BSO) procurement strategy, and access to emergency supplies.
230. The Trusts also have centralised collection/ delivery points, with most stating they supply on a weekly basis. Belfast Trust reported that it had to acquire new premises for this purpose due to the volume being processed.
231. As became very evident, owing to supply and demand, the costs of PPE continued to increase, placing a significant financial burden on organisations, such as Positive Futures, which previously had little or no need to source PPE. To assist voluntary sector providers, the Association for Real Change (ARC) established a link with a local supplier which assisted in the central procurement of PPE at a more competitive cost.
232. The RCN and Age NI both called for a central procurement process to avoid homes competing against each other for PPE and to ensure both, sufficient stocks, and security of supply.
233. Some Trusts (Northern and Southern) suggested that the centralised purchase of PPE would lead to better value for money than individual care homes could achieve on their own and that BSO could take the lead for centralised procurement and delivery.
234. As referenced in the NI Assembly research paper, at Appendix 4, an initial review of practice in other countries highlighted that almost all countries have experienced shortages in PPE for their long-term care facilities, or difficulties in procurement (e.g. Belgium, Finland, Germany, Republic of Ireland, Malta and the United Kingdom). Several countries reported managing this challenge by centralising procurement of PPE for regions (e.g. the Czech Republic, Denmark, Estonia, Finland, Germany, Greece, and Malta). In Malta the procurement of PPE, medical equipment and all the requirements related to the pandemic response, took place through a single centre to ensure adequate planning for critical resources and accountability of utilisation. Others (Estonia, Italy) emphasised the need to streamline procurement for all private and public long- term care facilities with the procurement for health services.
235. DoH Guidance for Nursing and Residential Care Homes (26 April) placed obligations on Trusts to work directly with homes on PPE issues, including offering PPE to homes from Trust stocks, at no charge.
236. By 22 October, the CSW advised the Health Committee that PPE costing £14 million had been supplied to care homes free of charge. Whilst guidance22 at that point made clear that homes were not to be charged for PPE supplied from Trust stocks, it also stated that this was a time-limited approach. This was supported by evidence given by the Department, which confirmed that PPE continued to be supplied where necessary by HSCTs and there have been no recent concerns about availability. The Department stated 'we have been advised that the support to supply will continue but an assurance on the continuity of supply and how long this will last would be of benefit.'
237. UNISON stated: 'It is vital that PPE continues to be made available for all care homes in a consistent manner and that there is strong oversight by Trusts and the RQIA, not only in relation to the stocks of PPE that homes are holding, but in ensuring that staff have access to adequate PPE where it is required. UNISON would urge the Department to require all care homes to provide weekly updates to their named point of contact within the trust, as to their level of PPE stock. These should be shared with trade unions as representatives of staff within care homes.'
238. Trusts were confident of the security of supply, with the Northern HSCT reporting that it has received assurances from the BSO that the supply chain required to deliver PPE to care home partners was secure, particularly in the items of highest demand, i.e. aprons, face shield masks, gloves and visors.
239. The NIA research paper made reference to PPE in the context of funding and increased costs for care homes, noting 'a significant issue remains, however, in that homes will, for the foreseeable future, require much higher than normal volumes of PPE and costs have reportedly spiralled by thousands of percent.'
240. This viewpoint was reinforced by COPNI who stated that the priority now must be security of supply as we face a second wave. Furthermore, it was COPNI's view that PPE should be provided free of charge for the foreseeable future and until a review of the tariff.
241. According to Age NI, care homes cannot be expected to bear additional costs for COVID-19 measures under the current tariff. For example, as highlighted by the RCN, care homes must now provide nitrile gloves for all clinical procedures, at approximately five times the cost of vinyl gloves. As a result, it argued that the regional tariff should therefore be upgraded to reflect this increased cost burden for care homes.
242. Whilst arrangements are working well, several Trusts made the point that they cannot indefinitely be expected to supply to ISPs but that, ideally, they should be assisted to secure their own supply. For example, the Western HSCT called for evidence to be supplied to show that the ISPs cannot secure PPE items from existing suppliers, given the provision of DoH funding to support this. The Southern HSCT suggested there was a need for clarity in respect of exactly what ISPs should be providing in terms of PPE, versus what Trusts were expected to supply in addition.
243. On 2 April, the Health Minister alluded to concerns expressed by HSC staff about the guidance in terms of appropriate PPE for use in different situations and informed the Committee of a UK-wide rapid review of guidance. On 27 April, the Minister announced updated guidance on PPE.
244. In support of a standardised approach across both statutory and independent sectors, PHA Infection Prevention Control Cell, developed and distributed guidance posters that identified the correct PPE to use in particular circumstances, along with posters detailing how to don (put on), doff (remove) and dispose of PPE correctly. Training videos that could be accessed at any time, and interactive zoom sessions were delivered by the PHA and HSC Trusts using regionally agreed procedures.
245. In oral evidence on 23 April, the Health Minister was asked about guidance of 17 April 2020, from Public Health England (PHE), and asked to give a commitment that staff would never have to re-use PPE due to shortages. The Minister said 'I cannot give that reassurance, because I cannot, hand on heart, sit here and say that in two, three or four weeks' time we may not be in that position' but continued 'staff should never be placed in that position.' NI guidance23 at the
time of writing stated: 'PHE issued guidance on 17 April 2020 regarding the reuse of PPE. Advice issued by the Chief Medical and Nursing Officers on 19 April confirms this guidance has not been implemented in Northern Ireland at this point in time.'
246. UNISON stated 'we understand that a regional review is continuing into the possible reuse of PPE. UNISON has yet to be substantially engaged with by this review. However, at this stage we would reiterate our opposition to Northern Ireland adhering to the guidance published by Public Health England on PPE shortages and reuse.'
247. In oral evidence given on 20 October, RCN stated that there were ongoing issues with the supply of masks required for 'aerosol-generating procedures' (AGPs). These require fit-testing, which takes up staff time but, moreover, masks for which staff have been fitted are going out of stock, leading to what it described as 'a constant round of fit-testing.'
248. In addition to items of PPE, some Trusts reported that they also supplied training and support in the use of PPE and infection control. For example, the Southern Trust reported that it produced a suite of PPE videos to support donning and doffing techniques, as well as keeping providers up to date on the guidance from the Department of Health and the PHA.
249. Evidence submitted by the PHA stated that there was a need for more academic research into the optimum use of PPE in care homes. There were some potential adverse effects, in that residents cannot see the face of members of staff and may not recognise them when wearing a face mask. Face masks covering the mouth result in difficulty communicating effectively with people with hearing impairment or who are deaf. Guidance to highlight and support effective communication whilst wearing PPE equipment was developed to highlight the importance of communicating effectively with residents, thus promoting mental health and wellbeing.
250. A number of organisations – Age NI, COPNI, and RCGPNI – supported the RLI findings that infection prevention and control, and education and training in donning and doffing of PPE, was crucial. Furthermore, they all advocated that training and information on any new knowledge, innovations or use of PPE, should be delivered promptly.
251. In oral evidence provided by a number of families they asked 'why can the HSC Trusts not train families in the use of PPE to support visiting and infection control?'
Funding
252. The financial resilience of independent care homes was a cause for concern for both the Department of Health and care home providers early on in the pandemic.
253. In its evidence, the HSCB described independent sector care homes as 'a critical resource in the effective operation of the entire health and social care system in Northern Ireland.'
254. To prevent care homes from closing due to financial pressures, the Department instructed the Trusts to block purchase 80% of vacant beds in homes
where income was reduced by 20%, and to fill the beds as required over the next three months, where it was safe to do so.24
255. The Trusts sent a regionally agreed letter to all care homes on 7 April 2020, advising that an interim payment on account would be issued, which would bring the value of payments to a minimum of 90% of the pre-COVID-19 average payments (adjusted for a 2020/21 price uplift). The Trusts advised that this measure was intended to provide supported, consistent cash flows for the ICPs, as it was anticipated that the processing of the payments for the beds booked by the Trusts might be delayed. Between April and September 2020, £1.1m was issued in interim payments on account. However, the Western Trust commented that the 'guidance re 80% support re bed occupancy levels requires strengthening, as providers are receiving this element of assured funding, albeit with an option to claw back and review at a future stage.'
256. On 27 April, the Department announced that £6.5m would be released to care homes to help with additional staffing and cleaning costs. Under this support, each home received a grant payment depending on size as follows:
| No. of beds |
0-30 |
31-50 |
51+ |
|---|---|---|---|
| Amount paid (£) |
10,000 |
15,000 |
20,000 |
257. On 2 June, the Minister announced a further £11.7m package of support, including funding for sick-pay, specialised cleaning and additional equipment. The HSCB submission provides further details of the breakdown of this funding below. This funding was issued on a claim and reimbursement basis.
- Up to £3.05m to assist care homes to pay their employees at 80% of their pre-COVID-19 average salary if they had to shield, isolate or were ill as a result of COVID-19 for the period of claim June to August 2020.
- Up to £6.4m of support for care homes to increase their level of environmental cleaning hours.
- Up to £2.2m to allow Care Homes to purchase additional essential equipment (to include pulse oximeters, thermometers, and portable tablet devices to support video communications) and with Trusts procuring defibrillators and syringe drivers for providers.
258. On 22 October, another £27m of funding was announced by the Minister to support providers to meet sick-pay of 80% of salaries, and to guarantee this until the end of the 2020/2021 financial year. In addition, this funding was available to support additional staffing costs (for instance, because of more acutely unwell residents or the need to support individuals self-isolating) and to facilitate block booking of agency staff; to continue with enhanced cleaning; to support changes to the physical environment, including to support safe visiting and; to meet other increased costs, such as IT. As with the previous funding package, this was issued on a claim back basis.
259. The necessity for longer term financial support to allow providers to plan ahead was highlighted by the Western Trust who reported that providers found that the funding for equipment, for example, came too late for them to benefit from it. It described as its 'overwhelming recommendation' that the 'DoH is encouraged to make a decision that covers the next 6-month period as the frequent changes in approach require an intense amount of support from Trust teams to process and administer.'
260. The initial allocation of grants to care homes was welcomed by providers, who were concerned about the impact of rising costs for additional staff, PPE and increased cleaning and infection control measures, early on in the pandemic. As the situation developed, there were further demands on resources due to the routine testing process, visiting monitoring and supervision. These demands were compounded by reduced staffing levels due to staff self-isolating; and remaining at home to look after children in the absence of available childcare.
261. In oral evidence to the Committee on 19 March, the IHCP commented that the short and long-term economic impact of COVID-19 on the sector would be significant. IHCP stated they had given the DoH a proposal in relation to additional costs but that it had not engaged with IHCP in discussions on the matter, as it did not view the proposals as independent.
262. In further evidence to the Committee, IHCP drew attention to the difficulties experienced by providers in accessing the additional funding. In particular, the IHCP stated that not all care homes that were under-occupied as a result of COVID-19, had received payments and that there was a delay in sorting out the blockages in the system. One survey respondent commented that 'the sector is now experiencing significant empty beds. The intended funding for those that fall below 80% occupancy is needlessly complicated. Direct support for the sector needs to be looked at again as there will be homes who cannot continue to financially survive for the second wave.'
263. In addition, IHCP highlighted the difficulties providers experienced in accessing funding from the £11.7m announced in June, concluding that time restrictions, bureaucracy and a lack of flexibility around what the funding could be used for, resulted in an underutilisation of the funding package. This evidence was supported by the RCN who stated that the administration and audit process required to secure the funding proved to be a deterrent, and that some providers had been unable to draw down funding due to the rigid criteria and tight timeframes.
264. Other stakeholders also commented on the lack of flexibility regarding the use of the funding: The Western Trust commented that some providers would have preferred to use the money to improve Wi-Fi rather than buy devices, or provide more one-to-one staffing for residents, but the prescriptive nature of the funding did not permit this. Similarly, the IHCP remarked that a care home that did not need additional technology to help with visits, but needed to create a different access area to the home which required them to build steps and a handrail, would not be able to avail of this funding for this. The IHCP further commented
that 'the fact that it was underspent did not at all mean that the money was not needed; it is just that it was impossible to claim all of it because of the system and the red tape that was put around it.'
265. The significant extent of the underspend was reported in written evidence from the HSCB on 20 October 2020, which indicated that, at that point, the level of claims from care homes was in the region of £1.3m. Together with Trust equipment procurement, the overall spend was currently approximately £2.1m. All Trusts reported that a number of care homes in each of their areas had not made a claim for reimbursement under the £11.7m funding package, and that some providers had not provided sufficient evidence in respect of claims made. In addition, Trusts reported that £1.1m of the initial £6.5m funding package was not allocated, and that the HSCB was in discussions with the DoH in relation to this. Of those who responded to the survey, the majority of care home owners and managers said that they had received some financial support during the pandemic.
266. In oral evidence to the Committee on 22 October, DoH officials stated that feedback from the IHCP regarding the eligibility criteria and the claim-back process had been listened to, and that subsequently the £27m envelope had widened the criteria to include funding for changes to the physical environment of a care home. The first tranche of this funding (£9m) was made available as a grant to support testing, visiting and the management of overheads. Providers were required to complete a pro-forma confirmation that they will carry out testing and support visiting, including care partner arrangements before payment. The balance of the funding has not been released to date, but the DoH has indicated that this will be issued on a claim-back basis. Providers have expressed concern that there is not sufficient flexibility around the use of this funding and that it is difficult to produce the required evidence of spend retrospectively.25
267. The need for audit and governance measures was acknowledged by stakeholders including IHCP and the RCN, as well as the Trusts and HSCB. As outlined in written evidence by the Belfast Trust, the initial £6.5m was subject to 'light touch' governance, where care home providers were expected to maintain a clear record of how the funds were applied. Also, they were required to complete a template confirming the application of the grant on COVID-19 related costs, with a sample subject to audit review and verification. However, subsequent funding was provided on a claim and reimbursement basis, and whilst stakeholders highlighted the difficulties with the processes, they acknowledged the need for governance and audit controls. In particular, UNISON called for routine audit and verification of spend, and expressed concerns that resources allocated by the Minister to support care home staff had not been uniformly drawn down, or passed on to staff.
268. The precariousness of the care home sector, pre-pandemic, was noted by stakeholders, including IHCP and Age NI, who commented that 'COVID-19 has exposed the fragility and inadequate resourcing of the social care system.' Care homes were already experiencing difficulties with staff recruitment and retention, coupled with a lack of planning and investment, reflecting the true cost of adult social care. In a press release on 13 May 202026, the Minister acknowledged that 'the social care sector has been struggling for years and as a whole is not fit for purpose.' Prior to the COVID-19 outbreak, the DoH had already appointed an expert advisory panel to report on areas of the sector in need of reform. The Power to People27 report was published in 2017, and included the need to establish a 'true cost of care' among its recommendations. In the same press release on 13 May, the Minister went on to announce his intention to move ahead with reform and investment plans, which will include training and terms and conditions for care home staff being standardised and improved. This announcement was welcomed by IHCP, whose Chief Executive expressed a willingness to work with the DoH in taking the reforms forward, whilst noting that it was 'unfortunate that it took a pandemic to highlight the pressures the sector had been under prior to the pandemic.'
269. Outside of the independent care home sector, other providers suffered financial difficulties, but were unable to access additional funding from the DoH. In evidence to the Committee, Positive Futures (which provides support for the learning disabled, including some residential respite care) reported that PPE, cleaning and other infection control measures were adding to financial strain. Whilst some funding was provided by the Department for Communities, this was not available for the purchase of technology to facilitate vital virtual support to families at a time when services were otherwise unavailable to them. The Northern Ireland Hospice reported that it had incurred £200k of COVID-19 related costs. At the same time, it experienced a reduced footfall in its shops and a significant decrease in donations.
Staff Terms and Conditions
270. In its written submission to the Committee, COPNI referenced its 'Home Truths' report recommendations (2018), which made clear the COPNI perspective on care home staff, from adequate staffing levels to employment terms and conditions. It was the view of COPNI that there was pressure on the availability of nurses in care homes prior to COVID-19, which was only
exacerbated by the fact that residential homes were not required to have nurses in their staff cohort. Furthermore, COPNI observed that caring for older people in care homes was a difficult job which was still not well paid, and challenged society to ask 'is this how we value the roles and jobs of people who care for our older relatives? Is it really OK?'
271. As evidenced by the Belfast HSCT, existing staff pay and conditions in the care home sector was a significant factor in the ability of homes to achieve a sustainable, skilled workforce, which undoubtedly impacted on recruitment and retention. Belfast HSCT expressed the view that this was an area that required reform to ensure staffing requirements, qualifications, training and development opportunities and equitable pay and conditions are in line with the public sector, concluding 'There is a need for the care home sector to be recognised as a unique area of practice with terms and conditions set to reflect this.'
272. Written evidence by Marie Curie reinforced that put forward by both COPNI and Belfast HSCT, concurring that challenges in securing the social care workforce predated the pandemic and included pay, terms and conditions and career progression. In its evidence, Marie Curie emphasised the importance of progressing the reform promised by the 2017 Power to People report.28
273. Age NI stated that now is the time to make a concerted effort to recruit, train and retain social care staff 'as we move into this period of increasing infection rates and winter months.'
274. As reflected by Belfast HSCT in its evidence to the Committee, a key risk during the first wave of the pandemic was symptomatic staff refusing to be tested or returning to work while symptomatic, as they were not paid for COVID-19 related absence. This was supported by the IHCP who acknowledged that there was considerable pressure and cost to address issues such as those off work isolating or needing to remain at home because their children are isolating.
275. As a result, on 13 May 202029, the Minister announced new measures to support care homes. He said 'I am therefore proposing to move ahead with reform and investment plans, subject to the necessary financial support being provided by the Executive. As an early priority, I want to see training and terms and conditions for care home staff being standardised and improved.'
276. Further to the DoH announcement on 2 June, Trusts implemented the regional package of support for nursing homes to enable staff pay to be guaranteed. This involved introducing a claims process to assist care homes to pay their employees at 80% of their pre-COVID-19 average salary if they had to shield, isolate, or were ill, as a result of COVID-19. The period of claim confirmed by DoH was from June to August 2020. On 3 September, the Minister confirmed that sick-pay funding was being extended 'while the funds are there' but remained a temporary measure. It remains unclear when/ if this will be mainstreamed into terms and conditions.
277. The RCN firmly believed that all care home staff should receive full pay for any COVID-19 related absences. This view was supported by the Alzheimer's Society, which stated that in homes where staff receive sick-pay, there are lower levels of infection in residents, 'perhaps because staff without sick-pay cannot afford to stay away from work, even if they are unsure about their own health.'
278. Written evidence from the IHCP stated that staff terms and conditions vary from employer to employer and that, whilst support to top up Statutory Sick Pay (SSP) was made available to staff in the care home sector, it was limited to a time specific period (3 June – 31 August 2020). The IHCP explained that it has sought to address the inequality between staff in homecare services and care home staff, and also the inequality of compensating those in care homes that were off in the latter part of the pandemic but not those at the peak.
279. This disparity in treatment was also referenced by Belfast HSCT who commented that retrospective payment to 1 April would have been more helpful to providers as this is when most of their staff were absent. It is worth noting that Positive Futures submitted claims to the HSCTs some months ago but, as of 16 October, no payments had been received.
280. The RCN highlighted that the independent sector generally experienced difficulties in recruitment as it is largely incapable of competing with the terms and conditions of employment offered by HSC Trusts.
281. According to the HSCB, it became apparent early in the pandemic that variations in the terms and conditions of employment across the care home sector were having a negative impact both on recruitment, retention and staff willingness, or ability, to adhere to specific guidance e.g. staff were reluctant to move to self-isolate as this meant a significant reduction in earnings. Similarly, staff who became unwell were dis-incentivised from going on sick leave as they were only entitled to the minimum SSP. Staff working on the frontline were also reporting challenges in accessing the correct PPE and keeping up to date with the Infection Prevention and Control (IPC) advice.
282. UNISON welcomed the DoH's initiative to fund the extension of sick-pay but also criticised the DoH for initiating the cover from 1 June and not back-dating it to cover March to May when many staff had to take leave. UNISON formally requested that the Minister secure the necessary funding required to backdate the extension of sick-pay to recognise the hardship care home staff faced during this period.
283. It also needs to be understood that whilst providers were paying staff who were absent due to sickness or isolation, they were also meeting the cost of a replacement worker, often needing to be supplied by an agency at a significant premium. In recent correspondence from the Western HSCT it states that: 'salaries of staff whose costs are supported by HSC funding provided under the contract should continue to be paid, even in circumstances where employees are required to self-isolate or work from home.'
284. Additional funding was made available to pay staff working overtime or additional hours to cover for colleagues who were ill or self-isolating. Staff were able to access additional training and support through on-line or e-learning platforms such as Project ECHO, organised through the PHA.
285. As referenced in the NI Assembly research paper 'COVID-19 and care homes, an international perspective'30, an initial review of lessons learned from other countries relating to care home staff terms and conditions highlighted:
- France offered a bonus for care workers during the COVID-19 pandemic.
- In England £1.6bn was provided to local authorities to backfill shifts.
- Germany increased care workers' wages with some of the federal states announcing one-off payments for staff working during the pandemic.
286. Evidence submitted by the RCPsych noted that its membership perceived a 'great deal of stress' on care home staff during the pandemic. Whilst they acknowledged that caring for people with cognitive problems is 'stressful at the best of times', the impact of staff isolating has had a significant impact. Responding to concerns about the impact of the pandemic on the mental health of staff, the Minister confirmed to the Committee that care home staff in the independent sector have access to the psychological support helpline staffed by Trust psychologists and psychological therapists. Positive Futures also acknowledged that there has been significant investment, across the sector, in a range of training and supports to strengthen resilience and support positive mental health.
287. It was the view of the RCN that care home staff did not generally have the same levels of access to occupational health services as was the case for HSC Trust staff. It believed that, given the current challenging circumstances, care home staff required additional emotional support and access to counselling services to enable them to maintain their mental health and wellbeing. Despite this, evidence submitted by the IHCP stated that support has included the psychological support services from Trusts being available to the independent sector. Whilst the IHCP was unsure of the uptake levels, it confirmed that Trust psychological support teams provided additional support to the care homes that faced multiple COVID-19 related bereavements.
288. In its written evidence to the Committee, the PHA documented how, in support of staff health and wellbeing, it led a project that saw the distribution of Rainbow Room resource boxes to each care home across Northern Ireland. Each box was filled with information and advice on health and wellbeing issues to support staff as well as activity packs, toiletries, biscuits etc. The Rainbow Rooms idea was adopted from the rainbow symbol of solidarity used by the NHS/ HSC during the current pandemic. The initiative was delivered through collaboration with the HSCB, ICPs, the PHA, HSC Trusts and the Healthy Living Centre Alliance, as a gesture of support to help strengthen the relationships between the care homes and the local voluntary and community sector.
289. The Northern Ireland Hospice stated that it has always had a culture of supporting staff wellbeing and personal resilience given the abnormally high levels of exposure to death and the emotional impact of supporting others through grief and loss. This has continued to be a fundamental consideration of the Hospice management team throughout the pandemic, which documented the following staff initiatives it provided:
- Help with food essentials, free meals, drinks and alleviating concerns for staff experiencing symptoms and/ or self-isolating
- A Hybrid Working Policy to ensure staff working remotely did not feel isolated; new laptops procured with webcams and broadband boosted for remote workers; flexible working introduced
- Ongoing confidential talking therapy and counselling service through a partnership with INSPIRE
- A 'Wobble Wall' was created by Hospice clinicians as a space for staff to write down their feelings and talk about them, if they wished.
- Peer-to-peer staff support and random acts of kindness
- Staff given up to two days' pro rata additional wellbeing leave in recognition of their effort and to promote resilience.
290. The Southern HSCT informed the Committee that it has provided IPC advice and guidance to individual care homes, as well as making care homes aware of regional guidance. Indeed, through its IPC contact, the Trust has offered advice in respect of how best a care home could set-up 'donning and doffing' areas to achieve best effect and to make best use out of PPE, ensuring that safe practice is supported.
291. According to the IHCP, care homes have worked hard to ensure the IPC measures around uniforms and PPE wearing are adhered to. This has required a review of areas in care homes where staff can safely have space so as to achieve good compliance. In some care homes, bedrooms have been taken out of use to accommodate donning and doffing. This approach was supported by the RCN which believed that, ideally, there should be changing and showering facilities for all staff in all homes.
292. In its written submission, UNISON argued that its members were at the frontline in dealing with the pandemic, yet their voices were not strongly enough heard due to a lack of trade union recognition in the private care home sector. Describing provision in the sector as 'almost entirely provided by the private sector for profit,' UNISON advised that terms and conditions vary across the multiplicity of providers. It stated that 'the vast majority of providers do not voluntarily recognise UNISON as a trade union representing staff' so while they will deal with unions on individual issues, there is no forum in which to discuss workforce terms and conditions, sick-pay and related issues.
293. UNISON estimated that between one-third and forty per cent of workers in the sector are in a union and stated that UNISON had active membership in 150 homes. The GMB union agreed with the points made on engagement and advised that it was difficult to be sure of total numbers due to a lack of information from private providers.
294. UNISON also argued that additional funding provided to care homes should include conditions requiring fair pay and treatment.
Staff Levels and Issues
295. There was general acknowledgement amongst the representative bodies and social care professionals with regard to the long-term challenges in securing the social care workforce that Northern Ireland needs. In written evidence, Marie Curie highlighted that these issues had existed for a long time prior to the COVID-19 pandemic. Positive Futures supported this view, stating that the sector is simply not competitive enough which 'has resulted in organisations experiencing real difficulties in the recruitment and retention of staff, resulting in organisations carrying significant vacancies.' Indeed, at the onset of the pandemic some organisations had up to 50% of their posts vacant and were heavily reliant on agency workers.
296. Root-and-branch reform was advocated in the Power to People report31 which stated that 'a low paid, high turnover and undervalued workforce is a poor way to ensure the quality of care we demand.' This sentiment was echoed by Age NI who believed 'a joined-up health and social care system, which values and adequately resources social care services, is vital if we are to respond effectively to the threat posed by COVID-19.' Reinforcing this, the BMA stated that 'crucially, care homes need to be supported and resourced, not just when an outbreak occurs but consistently throughout the pandemic and beyond.'
297. As referenced in the NI Assembly research paper 'COVID-19 and care homes, an international perspective'32 staff shortages were raised with the Committee, and acknowledged by the Department,33 as early as 19 March. As stated by the CSW, 'care homes and domiciliary care providers are likely to face challenging staff shortages...ongoing family support will be crucial as we co- ordinate staff resources and look to deploy volunteers, where it is safe and
effective to do so.'
298. As part of its inquiry, the Committee sought the views, via an online survey, of owners/ managers (employers), staff and residents'/ family members into the impact of COVID-19 on care homes. One individual who responded to the survey stated 'staff have been very dedicated but I am very concerned about future workforce planning as it is impossible to recruit sufficient relief staff quickly enough to cover absenteeism. There was a workforce shortage prior to the pandemic within the Care Home sector and now with fear of COVID-19 it has compounded recruitment issues. From mid-March it has been very difficult to keep up to date with routine governance.'
299. The RCN identified significant staff shortages within nursing and residential care homes in Northern Ireland in its 2015 report 'Care in Crisis'. They informed the Committee that the position has further deteriorated during the last five years, with care homes generally having minimal staffing levels and no pool of staff to call upon in order to address shortages.
300. On 23 April 2020, the Minister briefed the Committee on making Trust staff support available to care homes, confirming that redeployments would be voluntary and that there had been prior engagement with the unions which was ongoing. He advised Members that there had been a good response from HSC staff and volunteers. Furthermore, in response to the staffing issues raised, legislation34 was also enacted in April to allow new recruits to start work before vetting was complete, after a 'barred list' check, Northern Ireland Social Care Council (NISCC) register check and subject to supervision and other safeguards.
301. The IHCP, in its written evidence, acknowledged this positive development, advising the Committee 'on 19 March, I mentioned regulations and registration. That was about being able to recruit people quickly. All those issues were addressed very promptly with the NISCC and various other bodies. We are now able to recruit quite quickly into the workforce.' This approach to relaxing registration requirements was also supported by Positive Futures.
302. On 13 May 202035, the Minister announced an increase in staff support from the HSC sector to the care home sector, building on existing partnerships with GPs, district nurses, Allied Health Professionals (AHPs) and social care colleagues, to deliver specialist care in the home, including via virtual ward- rounds where appropriate.
303. The Minister briefed Members, on 20 May, that professional staff returning from retirement to the HSC, were being prioritised for deployment to care homes, subject to suitable skills and experience. He also advised that agreement had been reached with local universities to bring forward the qualification date for social workers, allowing them to enter the workforce several weeks earlier than would have otherwise been the case.
304. On 17 June36, the Minister announced plans for a new Surge Planning Strategic Framework for nursing, medical and multidisciplinary in-reach into care homes. In written evidence, the PHA acknowledged this Framework and its specific reference to the need for adequate contingency plans in the event of increased staff absence as a result of COVID-19 infections among care home staff.
305. According to written evidence submitted by the HSCB, the CSW directed HSC Trusts to work with providers to develop Mutual Aid Plans (contingency arrangements) to respond to the pandemic. This included the provision of staff and other supports to the sector. HSCB staff developed a 4-stage model to assist providers to identify when, and in what circumstances, they should contact the Trusts for help. In addition to the development of a Mutual Aid approach, regional meetings facilitated an exchange of ideas and learning and helped provide some level of consistency across all Trusts, clarified issues and improved communication.
306. Where Care Homes did not have adequate and safe staffing resources they were therefore able to link with the HSC Trusts, who were able to offer support, mainly by redeploying Trust staff. All five HSC Trusts provided evidence to reflect that they had from the spring effectively supported many local nursing and residential care homes through redeployment of staff, both nursing and healthcare assistants. However, by the autumn, the Western HSCT emphasised that 'we have exhausted our pool of volunteers and there are significant workforce pressures in acute and community sectors which will impact on our ability to provide staff to care homes. In addition, we have less staff in the system to be able to redeploy to care homes if we are not standing down services.' Furthermore, the Southern HSCT stated: 'whilst the Trust responded to the majority of requests, there was particular difficulty responding to requests for registered nurses...there continues to be a lack of registered nurses available for such duties.'
307. The South Eastern HSCT explained that it would be considerably more challenging to provide support should it be required in a second surge for a number of reasons:
- increased testing and contact tracing is resulting in significant numbers of staff not available to the workforce reducing the overall pool of staff available to draw from;
- a number of staff who supported care homes in the first surge are now back working in their own service as it attempts to re-build;
- requirements to staff other initiatives, such as the Nightingale hospitals, are all competing for staff; and
- redeploying HSC staff to support independent sector homes remains a voluntary arrangement and staff can refuse.
308. As evidenced by the RCN, 'one of the clear lessons of the 'first wave' is that nursing and residential care homes simply will not be able to function without staffing support from the respective HSC Trust. Trusts are managing staff cover through redeployment from stood down Trust services, workforce appeal, bank/ agency arrangements and staff willing to work additional shifts in care homes. Trusts find this challenging as they are experiencing staff shortages, particularly registered nurses. Despite best efforts, some Trusts are not able to meet demand.'
309. In the experience of the IHCP, not only was shortage of staff an issue, but also additional tasks had been added to existing staff workloads, such as routine testing, visiting, additional monitoring, assurance, surveys and audits. According to the BHSCT, staff from Trust Patient Client and Support Services were deployed to work within five care homes to support cleaning requirements during the first surge.
310. Further evidence submitted from the IHCP highlighted that concerns had been raised about agency staff and student nurses moving from care home to care home and to Trusts. The NHSCT, in its written submission, asserted that the movement of staff is strictly monitored, with tight controls in place to minimise staff working between different facilities. However, the SHSCT acknowledged that 'whilst it was desirable to manage staff allocations on the basis that, where possible, staff would not work across more than one care home and statutory setting, due to the lack of staff, in practice this proved very difficult.'
311. RQIA advised care home providers in terms of managing staffing levels and ratios safely, in keeping with the regulatory expectations. As a result of this flexibility with regard to staff ratios, the SHSC Trust reported that it managed to employ staff safely and efficiently from the Workforce Appeal lists throughout the pandemic.
312. Written evidence provided by the RQIA detailed how the organisation launched the Regional Care Homes Status App, in mid-April 2020, to facilitate the collection of information. The App required each care home to rate their current workforce and PPE status and to provide: current numbers of staff and residents who have been tested; numbers of staff and residents who are symptomatic; numbers of staff and residents testing positive; whether the home is in need of additional nursing or care staff; and whether the home requires a terminal clean. This information was then shared with the DoH, PHA, HSCB and the five HSC Trusts to assist in the HSC's joint response to the COVID-19 pandemic and to ensure that duplication in reporting was minimised and reporting was regionally consistent. The collection of this information via daily status updates from care home providers/ managers has been crucial to the HSC in determining which care homes are most at risk and in need of support during the pandemic.
313. According to the RCN, there was currently no dependency tool or agreed staffing ratio that would enable the sector to determine the staffing levels that are required to deliver safe and effective care. Phase eight of the Department's Delivering Care normative staffing framework, relating to nursing homes, was due to be completed in March 2020. In January 2020, however, the PHA held a meeting with independent sector representatives and informed them that it would, instead, be introducing the Telford model in March 2020. This is simply a mechanism for converting shift-level staffing plans into a calculation of the number of staff that are required to fill the daily staffing rota, making allowances for annual leave and sickness absence. The RCN had previously stated its concerns about the introduction of the Telford model without an associated dependency tool and its belief that the Telford model does nothing to secure or promote safe staffing. It was the view of the RCN that it fails to address the question of how evidence-based decision-making around staffing requirements could be supported, which is what providers require and expect.
314. As detailed in its written submission, the PHA provided a strategic leadership role in providing guidance and supporting implementation of guidance by initiating and informing the training of the care home workforce. Initiated by PHA nursing experts, a diverse range of COVID-19 training courses for care home staff to support symptom management, infection control and supporting their mental health and wellbeing, was implemented on virtual platforms to reach 2,695 nursing and residential home staff and, via 251 ECHO sessions to 8,408 residential, nursing and domiciliary care home staff.
315. The Southern HSCT reported to the Committee that it was the Trust's view that it was important to prepare and support staff allocated to work in care home settings and therefore an induction programme was agreed for such staff. This was seen as essential for staff who had no previous experience of working in the independent care home sector. Staff working in these settings were made aware of the standards and guidelines that applied to these specific settings and, where possible, staff were allocated to care homes through a buddying arrangement, whereby two staff were allocated together. Training was tailored to individual care homes, to ensure staff were as well prepared as possible. A similar approach was also adopted by the South Eastern and Northern HSCTs.
316. According to evidence submitted by Marie Curie, the COVID-19 pandemic has further exposed long-standing issues with the levels of training and experience in palliative care in some care homes in Northern Ireland. They stated: 'many care homes provide excellent palliative and end of life care for their residents, but this is not universal and where gaps do exist, the root of the problem tends to be structural – with high staff turnover, inadequate staffing levels and lack of access to training due to time pressures and funding issues all making it difficult to equip care home staff with the skills they need to provide complex care to dying residents.'
317. The Belfast HSCT stated that the COVID-19 pandemic had highlighted the need to consider the care home sector as an area of specialist practice with a specific career pathway, qualifications and training and terms and conditions reflecting this. There was a need for further definition and enhancement of management and leadership roles, and a structure that provides visible leadership over seven days. Enhanced responsibilities such as those for adult safeguarding, infection prevention and control, a dementia champion and tissue viability, are examples of essential roles to ensure the safe and effective delivery of care. Staff therefore required a level of training that reflected the responsibility and expertise of these roles. This approach was also supported by the RCN who were of the view that it was essential to develop a career progression pathway for care home staff that embraced the same levels of access to training and professional development as that available to colleagues working within the HSC.
318. The Department's RLI into the transmission of COVID-19 into and within Care Homes, which reported in September, identified learning in advance of a predicted second surge of the virus. Despite discussing the enhanced cleaning requirements in care homes, the RLI report admitted, however, that there is no recognised regional training on environmental cleanliness and recommended that care home staff be provided with a 'freely accessible regional IPC training e- learning module'.
319. In evidence to the Committee on 22 October, the CSW pointed out that videos and training, through the Clinical Education Centre and NISCC, focusing on infection prevention and control and PPE, as well as clinical skills such as care of respiratory patients, were being made available without charge to all care home staff. He also alluded to leadership training developed for care home and Trust staff.
Access to Health and Social Care
320. The Committee heard a number of concerns on access to ongoing medical care and other health services, planning of advanced care and the delivery of care at end of life. Practical challenges cited by representative bodies and organisations included access to GPs and other healthcare professionals, and the pressures on already stretched staff. Stakeholders described the need for a holistic approach to 'wrap-around' care that is centred on the wellbeing of individuals.
321. The effectiveness of employing virtual ward rounds to access medical care during the pandemic, and the appropriateness of relying on them as a level of oversight, was raised consistently by stakeholders. Age NI commented that 'some of the concerns that came to our door included the view that, if GPs were not able to visit, care home staff had to take a photograph and send it to the surgery.' It considered that this was an unfair burden to staff who are not clinically trained.
322. The NI Hospice said it was difficult to ensure a holistic approach given GPs increasing use of telephone consultations. It stressed that delivering care in a cohorted environment for all patients was underpinned by two fundamental principles: firstly, doing everything to make people feel safe and, secondly, treating people as individuals. Age NI added that GP and other healthcare services must become part of the team to support an older person stay well and as independent as possible. Marie Curie concurred with the concern around reduced access to GPs for care home residents, specifically highlighting reduced opportunities for Advance Care Planning conversations (discussed further below). COPNI said it had little information on whether virtual ward rounds were sustainable in the longer term, but understood that the approach helped in the first wave of the pandemic.
323. IHCP noted that, whilst each Trust had a COVID-19 response plan in the first surge of the pandemic, the interface with residents' own GPs, who know them best, was almost non-existent. On an operational basis, the IHCP highlighted the difficulties care homes experienced in the early days of the pandemic with basic supplies of paracetamol, oxygen and antibiotics, as care homes could not store medicines and could only hold prescribed medicines for individual residents, which could not be used by others.
324. The RCGP sought to provide reassurance on access to medical care by
confirming that 'subject to clinical need, GPs will still tend to patients face-to-face as necessary, taking appropriate precautions including use of PPE and adhering to distancing and infection control measures as much as possible.' The RCGP drew attention to UK-wide guidelines on 'Top Tips for GPs Caring for Care homes'37, published May 2020, advising GPs to maintain good communications, especially with professionals closest to the patient. It said also, that digital technology was enabling more co-ordinated, multi-disciplinary support for patients.
325. The HSC Trusts advised that medical care in care homes is provided by GPs under the General Medical Services (GMS) contract and advised that Trusts liaised with GPs to support virtual ward rounds. In written submissions, Trusts outlined the clinical support provided to care homes, via 'in-reach' and support teams who referred to Enhanced or Acute Care at Home teams as required. Where care could not be managed, residents were referred to acute services or admitted to hospital. In addition, other support was provided, for example by AHPs including dieticians, speech and language therapists, and from Trust geriatricians.
326. The HSCB made reference to the development of Surge Plans in May 2020, implemented regionally, which advised of the need for medical care to be available both virtually and on the ground, to provide clinical assessment and management in care homes. The plans were supported by agreed metrics, which were developed with stakeholders, with assurances provided by Trusts to the HSCB and the PHA. Emerging challenges were identified and incorporated into regional documentation to develop a standardised response to the pandemic and develop support needs of care homes, including for advance care planning.
327. In its evidence, the PHA confirmed that dedicated care home support teams had either been established or enhanced from 2018 through Transformation funding. In each of the five HSC Trusts, a team of clinical staff are employed with the aim of enhancing the competence of care home staff to facilitate discharge from hospital and prevent inappropriate hospital admission.
328. The RCPsych felt that a regional policy on medical support to care home patients in time of pandemic would be useful and bridge the potential problems of boundary issues and differing guidance coming from Care Homes, Trusts and Primary Care providers.
329. In a written submission, the BMA outlined its involvement in discussions with stakeholders and experts to review the healthcare needs of residents in care homes during the pandemic. A potential outcome from a range of options considered, is that each care home will be linked to one practice. The BMA commented that 'COVID-19 has highlighted the need for us all to work together, to provide a more proactive and dedicated service for care homes which will include advance care planning, education and peer review and a consistence for all homes in terms of contact and management.' The RCGP advised that, in principle, it supports the proposal to align one GP practice with each nursing home but urged consideration of a 'plan B' where a home is not near a practice; it also stated that training of care home staff should be considered.
330. When questioned on 20 May in Committee about residents' deaths in care homes rather than hospitals, the CMO explained that residents, families, GPs and care home staff were involved in discussing the most appropriate care in individual circumstances. Assuring Members that, where hospital care was required, a resident would be transferred, he recalled the Minister's announcement38 that acute care at home was being extended to care homes, saying the Department had 'worked with hospital trusts, the acute care at home teams, the enhanced care at home teams, general practice and respiratory nurse specialists, doing virtual ward rounds and telephone consultations.' The RCGP NI, in its evidence to the Committee, was supportive of the Acute Care at Home programme being embedded within care homes as standard.
331. The Committee is cognisant that, on 17 June, recognising the long-term increase in acuity of healthcare need in care homes, exacerbated by the pandemic, the Minister announced39 that the CNO would lead work to co-design a new framework for nursing, medical and multidisciplinary in-reach to care homes.
332. The RLI report, led by the Department and published in September 2020, acknowledged that residents had raised the lack of access to medical support and management during the spring, but reported on a positive experience where Trust support teams had been able to offer in-reach support, in line with evidence heard by the Committee.
333. The IHCP described how normal life for residents had been greatly impacted by isolation, infection control requirements and by reduced services such as podiatry and occupational therapy.
334. BASW drew attention to DoH guidance which stated that in-person appointments should continue where the relevant HSC professional deems it to be appropriate, contrasting this with patchy implementation by care homes. In highlighting their members' concerns that some residents had not had social work contact for several months, BASW said that while it was not questioning the care being provided in care homes, it considered that the role of social workers to take both a holistic approach and to safeguard human rights, was being severely hampered as a result. Specific concerns were raised regarding Mental Capacity Act Deprivation of Liberty Assessments being incorrectly conducted where GPs had refused to complete Form 6 of the assessment process; however, BASW flagged this had been an existing problem that had worsened since the onset of the pandemic.
335. The Alzheimer's Society raised issues pertinent to those residents with dementia. In particular, they drew attention to the use of antipsychotic medication to sometimes treat behavioural and psychological symptoms of dementia patients in care homes. Referencing data from NHS Digital for England that the percentage of patients with dementia prescribed antipsychotics had risen from a stable 9.4/9.5% in the eight months prior to March 2020, to 10% in the six weeks leading up to April 2020, it suggested any increase in the use of such medication should be investigated as a possible effect of lockdown. They also advised that usage should be monitored to identify trends with a view to undertaking action as required.
336. Furthermore, the Alzheimer's Society advocated that there should be a UK- wide strategy to enable those with dementia to recover from the effects of the pandemic, including rehabilitation, support for mental and physical health, and speech and language therapy.
Advance Care Planning
337. A key theme in the evidence presented was Advance Care Planning (ACP). Marie Curie stated that the COVID-19 pandemic has highlighted the importance of sensitive and compassionate conversations around ACP, to allow patients and their loved ones to consider ceilings of treatment, issues such as resuscitation and end of life preferences, including whether to be admitted to hospital. COVID- 19 has made these conversations much more difficult and challenging under social distancing measures and restrictions on in-person visiting. Marie Curie advised that, given the rapid decline seen in COVID-19 patients, especially if living with other complex comorbidities, as is the case with many care home residents, the timeliness of ACP conversations is now even more important. Marie Curie voiced its support for the treatment and care planning under National Institute for Health and Care Excellence (NICE) guideline NG16340, highlighting key elements as follows: the need to discuss risks and likely outcomes; development of an escalation treatment plan; need to establish if an ACP is in place; and document and record.
338. COPNI stressed that conversations should be handled sensitively and with full engagement between the individual, the clinician and their family, or their next of kin, where appropriate. There was a sense that the pandemic had crystallised the significance of ACP and that it should not, in effect, be left to be considered during a crisis situation.
339. The RCGP emphasised to the Committee that ACPs must be developed on an individual basis and should not be applied to a group of people. They also stressed that ACP is a much wider conversation than the circumstances where DNAR would be appropriate. Echoing this, the PHA stated that ideally everyone in a care home should have an ACP, with all decisions documented and, which should accompany them in the event of a hospital admission.
340. Marie Curie acknowledged that public trust and confidence in the ACP process may have been diminished by media stories in the early months of the outbreak which alleged that local patients were pressured to sign Do Not Resuscitate orders (DNR) - or as they are increasingly known Do Not Attempt Cardiopulmonary Resuscitation (DNACPR) orders - without consultation with them or their families. Marie Curie suggested that a public messaging campaign could address negative perceptions. The Alzheimer's Society flagged reports of a lack of consultation with families. Equally, these concerns were referred to by Age NI who requested that this does not become a feature of any future waves of infection. Age NI was of the view that the Department of Health should clearly outline and communicate the rights of older people and families to support stating the sensitive conversation about end of life, at a time and place that suits the individual, family and their doctor with the wishes of the resident and family recorded.
341. Specifically with regard to DNACPR policy, Marie Curie advised that the Palliative Care in Partnership Programme (PCiP)41 which provides support to care homes caring for people at end of life during the COVID-19 pandemic, submitted an updated DNACPR policy to the Department of Health for consideration and approval in December 2017. A new work plan for the development of an overarching ACP policy, which will include DNACPR, is under way and is due for completion by May 2021. The PHA, which advised it has an active role within the PCiP programme confirmed that the Regional Palliative Medicines Group (RPMG) working with the NI Specialist Palliative Care Pharmacy Group and, supported by the PCiP programme, has developed specific management guidance for those with COVID-19 at end of life care.
342. The IHCP said that the commitment to completing ACP for all residents has not been fully achieved. In practice, Marie Curie said it was their view that ACP had been hampered in some cases by the lack of a regional recording and reliance on paper-based systems, exacerbated by different teams working across different systems. Also, some GPs may record ACP as part of a patient's Key Information Summary (KIS) but not all patients have this as KIS is not universally adopted in NI and, even where it is in place, it can only be accessed by the person's GP. Marie Curie said that it is hoped that the Encompass IT system may have the capability to address this; however, pending it becoming operational, Marie Curie suggests that the patient portal for those with dementia, initially launched in 2018, may provide an alternative route in the interim. Furthermore, Marie Curie cited, as an example of best practice, the 'Co-ordinate My Care' 42system currently operating in London which makes ACPs accessible to a wide range of HSC providers, including care homes and ambulance staff; after a GP referral, a registered nurse works with an individual, their loved ones and care home staff, by phone, to complete the ACP.
343. On that point, RCGP said in its evidence that it believed GPs were frequently the best placed to take the lead on ACP but 'would support ACP being carried out by the multidisciplinary team member who knows the individual best.' RCN highlighted that additional training and medical input was required to undertake the lead role and took the view that GPs should be required, under a clear regional policy, to participate in DNACPR decisions alongside the patients, relatives and the care home.
344. The Trusts concurred that the responsibility for ACPs rests primarily with GPs and should be completed with the resident and any family carers as appropriate. The challenges associated with proactive advance care planning were acknowledged, including communicating with multiple GP practices and difficulties with arranging site visits.
345. Discussing palliative care, the NI Hospice emphasised that continuous communication and shared decision-making with patients and families, are fundamental principles of delivering palliative care. Furthermore, it was essential in supporting patients to make informed choices around DNACPR, and who they wished to be with them at end of life. The Hospice highlighted that access to social workers and the pastoral care team helps to support the anticipatory grief of families and enhances emotional, spiritual and psychological care. The Trusts advised that they had provided bereavement and psychological support for families and staff.
346. Marie Curie, given its experience of providing increased levels of support for local care homes during the pandemic, believed this underlined the urgency of ensuring greater palliative and end of life care in-reach to care homes, including both medical and nursing care for patients. In the specific context of COVID-19, palliative care had been shown to play an important part in managing the distressing symptoms caused, including breathlessness, anxiety and agitation.
347. Marie Curie said it was clear that some homes needed greater support due to heightened workforce pressures in the sector. However, the need for greater provision of palliative care is for all those requiring it at end of life, not only related to COVID-19, and this need was evident even before the pandemic. As such, Marie Curie advised the Committee that it is currently engaging with the care home sector to assess palliative and end of life support needed by providers.
348. On 3 December 2020, the Health Minister wrote to the Committee to advise that work had commenced on the development of an ACP policy for adults in Northern Ireland and that an early stakeholder engagement process is planned to begin shortly. The development of the policy was intended to support ongoing work to implement a public health approach to palliative care. The Minister said that, importantly, a public health approach also recognises and promotes the need for community-based support for people with palliative and end of life care needs and the importance of ACP for future care, including wishes and preferences for care, Advanced Decisions to Refuse Treatment and decisions around cardiopulmonary resuscitation.
Regulation
349. In the early days of the pandemic, providers asked for flexibility around regulations, staff rules and responsibilities in the form of changes to NISCC registration requirements and the RQIA's inspection process, in order to expedite the employment of additional staff to fill the gaps left by workers who were off sick, self-isolating or unable to work due to caring responsibilities. On 20 March, the Department of Health instructed the RQIA to reduce the frequency of its statutory inspections and to suspend its non-statutory inspection activity and review programme, in order to reduce the risk of spreading the disease and to permit it to take on more of an advisory and support role. In addition, new regulations43 were made on 2 April 2020 to allow new recruits to begin work after a cleared barred check, whilst other vetting and registration procedures completed.
350. RQIA was instructed by the DoH to establish a Service Support Team (SST), to provide guidance and act as the first point of contact for nursing homes, residential care homes, domiciliary care agencies, and supported-living providers during the pandemic. This support was provided by a help-desk, which in the early days of the pandemic operated daily from 8am to 6pm. This service was welcomed by care home staff and other stakeholders such as Positive Futures, IHCP and the RCN, who reported that it provided invaluable support to its members. Providers also welcomed RQIA's flexibility around the staff ratios permitted.
351. In addition to the SST, the RQIA worked with the HSCB to redeploy some RQIA inspectors to support care home experiencing staff shortages or IPC concerns. On-site support teams were deployed to strengthen IPC measures in home that were COVID free. The HSCB reports that this service ran from May to early July, and supported 13 care homes by providing one-off on-site visits. However, HSCB noted that, although feedback from these care homes indicated that the visits were useful, there was no opportunity to follow up if the advice provided had been adhered to. The HSCB also reported that there was some confusion over the RQIA's role in providing this support, as providers did not distinguish the RQIA's visits in this supportive role from its regulatory visits.
352. In mid-April 2020, RQIA introduced the Regional Care Homes Status App to facilitate the collection of information from care homes. Care homes logged information regarding the health status of its residents, staff levels, PPE levels and other issues. The Department, PHA, HSCB and Trusts were able to see from the app (which was later developed into a web portal) where problem areas lay, and take remedial action by directing resources or other support. However, some care home managers found the daily input of information to be a burden, while the South Eastern Trust reported that the information was not always accurate where providers omitted data or did not update their returns.
353. The DoH's instruction to the RQIA to scale back on-site inspections of care homes and to focus on support in the early stages of the pandemic was a matter of some contention. In correspondence of 3 June 2020 to the Committee, RQIA advised that 'normally, when an outbreak occurs in a care home, RQIA inspections do not occur for the duration of the outbreak to minimise the risk of inadvertent onward transmission.' Concerns were raised by families and other stakeholders that on-site inspections had been scaled back at a time when family visitors and other observers were prevented from entering care homes. In evidence to the Committee on 14 May, RQIA advised that they had continued to inspect where issues were raised with them or where, through their advice and support role, they became concerned about a home. It reported that 22 on-site inspections and 13 remote assessments took place between April and May (as compared with 148 during the same period in 2019) and a further 25 inspections were completed during June. Enforcement actions were taken where necessary, with a failure to comply notice issued to a nursing home in Belfast, due to findings from an RQIA inspection in mid-May 2020. The RQIA also advised that this reduction in regulatory inspections during the height of the pandemic was in common with the practice of other regulators across the UK and in the Republic of Ireland.
354. On 22 June, the non-executive Board of the RQIA resigned, citing the Department's decisions to scale back inspections and to redeploy senior RQIA staff without consulting the Board, as reasons for the mass resignation. In a statement to the press, former Board Members said 'in the Board's view these decisions diluted the RQIA's independence and critical function as a regulator to maintain the protection of vulnerable adults in residential and nursing homes during the COVID-19 crisis.'44 The Committee expressed its concerns around the resignation of the Board members to the Minister; in response the Minister announced that he would conduct a review into the matter. This review was due to complete in December 2020.
355. The decision to repurpose RQIA was rescinded on 22 June; in a press release, the Department stated that it was able to lift the restrictions due to the decrease in community transmission. In evidence to the Committee on 22 October, the Chief Executive of RQIA acknowledged that lessons had been learned from the early days of the pandemic and that the organisation was moving towards a risk-based assurance framework, where resources would be directed to areas of higher risk. The Chief Executive described this as a 'blended approach' that might involve a variety of interventions, ranging from support and advice, or specific interventions, such as comprehensive or focused on-site inspections, remote inspection involving staff and service user interviews, contact by phone or video link, manager self-assessment submission or materials of self- declaration, or meetings with the provider or with the Trusts.
356. Stakeholders, including IHCP, were initially supportive of the decision to scale back regulatory inspection, as a means to reduce the burden on providers and to reduce footfall in the homes, but later commented that virtual visits were more resource intensive than on-site. The Chief Executive acknowledged that there was a balance between the risk of lowering safeguarding through fewer inspections, and preservation of life, but that preservation of life must come first. Similarly, Positive Futures commented that 'whilst inspections provide a certain level of assurance, efforts need to continue to identify other ways of providing assurances.' Other stakeholders, such as COPNI and Age NI, recognised the importance of on-site inspections in providing assurance to families and the public that care homes residents are safe and well cared for; they expressed concerns that the lack of connection through reduced visiting, 'have caused some to worry about the risk of abuse and neglect.' COPNI recommended that regulatory inspections need to recommence at normal levels of frequency and UNISON called for the decision to scale back the inspections to be revisited. Age NI suggested that, while paperwork could be done remotely, RQIA should be considered part of the essential services which enter a home, commenting that 'perhaps the focus could be more on the observations of the quality of life, the practice of care and PPE.'
357. The Belfast HSCT took the view that there was a 'detrimental impact of the standing down of RQIA routine inspections and statutory care reviews', which created difficulties in maintaining oversight. The requirement for care homes to reduce footfall for all routine visits, including Trust staff visits, resulted in a number of care homes refusing any on-site visit. The Trust commented that, although the statutory care homes were subject to the same guidance and restrictions as the independent sector, the Trust was able to maintain effective oversight of the quality of care and governance in these homes throughout the pandemic. Whilst it acknowledged the need to balance the risk of infection transmission with the need to ensure the safety of residents was not compromised, the Trust stated that it would be keen to maintain staff visiting homes in line with its governance arrangements and for RQIA enhanced inspections to continue. The Southern Trust also made the point that any direct engagement with care homes was in line with previously agreed regulatory standards and agreements.
Communication
358. Stakeholders were generally supportive of the RQIA's role in acting as a conduit for help and support in the early days of the pandemic; this service was reduced during the summer months to the disappointment of stakeholders, such as Positive Futures and RCN, who called for it to be reinstated during a second surge. This issue was addressed by the Chief Executive of RQIA, who confirmed in October that the help desk had resumed a seven-day service. However, some stakeholders, including providers and families of residents, complained that communication around guidance was not always clear, and that there were inconsistences in the application of the guidance.
359. BASW reported that, while it recognised that RQIA continued to provide support to care homes and inspect where necessary, there was a failure to communicate this ongoing work to social workers; as a result, BASW NI members felt regulatory functions had been informally delegated to social workers, who were unable to access residents except by telephone. In addition, BASW members felt that poor communication regarding Mental Capacity Act assessments left staff unsure if they were expected to undertake such assessments or if the requirement had been suspended.
360. UNISON advised the Committee that it was seeking agreement on a protocol for information-sharing between itself and the RQIA in relation to social care settings, as it felt it would be helpful to have a direct means of communicating issues of concern to the regulator.
361. The Western HSCT reported that feedback from providers indicated that RQIA should communicate more effectively in a proactive supportive way with providers, with clear guidance and updates, alongside Trust colleagues.
362. Stakeholders raised the issue of a lack of consistency in the application of regionally agreed guidance between care home providers. UNISON described variations in the implementation of testing policies, and the PCC advised that 'the lack of consistency in visiting across different care homes was universally cited as a significant source of frustration for families '. Inconsistencies in the application of guidance between the independent and statutory care home sectors in particular was noted; the PCC reported that families questioned why visitors were still allowed in Trust-run care homes while they were unable to visit their loved ones in their independent sector home. The RLI report concurred with some of the complaints heard by the Committee in relation to consistency of approach, conceding 'whilst much good has been achieved, there has been variance in application of the policy and practice changes across the Care Home sector and HSC Trusts '.
363. In its evidence to the Committee, RQIA emphasised the risk-based approach to inspections it had now adopted, following the first wave of the virus. The Chief Executive described how the RQIA was analysing the data it held to identify the shared characteristics of homes most at risk of an outbreak, which included: larger homes (40+ registered places); homes run by larger providers; homes located in urban areas; services with more than two manager changes over the past year; and services registered within past 10 years. UNISON expressed concern that having numerous different providers in the care sector would lead to difficulties in coordinating best practice, and maintaining effective oversight to control the virus.
364. The future of regulation post-pandemic was raised by a number of stakeholders. In a press release on 2 June, the Minister stated 'A review of regulation is ongoing and is of crucial importance ... I am keen to explore ways of strengthening accountability when care home providers repeatedly fall short of regulatory standards across a number of different homes under their control.' In evidence to the Committee, the Chief Executive of RQIA commented that the 'blended approach may represent the future of regulation in a post-COVID world.'
365. In relation to the pandemic, the RCPsych commented that the need for rapid action risked infringing the rights of the individual, and suggested that consideration should be given to how this might be accommodated. The RCPsych further recommended that standards assessed by RQIA should incorporate areas of pandemic planning beyond infection control; it suggested that mandatory anticipatory care planning, visitation planning and end of life care planning might safeguard the needs of patients better in a rapidly evolving situation such as the pandemic.
Pandemic Preparedness and Systemic Issues
366. The evidence presented to the Committee identified a number of risk factors and learning that may be helpful in planning for a further surge, or another pandemic. There is also useful read-across from other sections of this report in terms of future planning.
Pandemic preparedness
367. In response to Committee concerns around specific planning for care homes in the early stages of the pandemic, the Department referred to the guidance and surge plans that it had produced in February and March; the CSW stated to the Committee in June that the Department had begun to consider additional support for care homes on the same day it had activated plans for acute hospitals.
368. The Committee took evidence on pandemic and surge planning from bodies including the HSCB, the PHA and the HSC Trusts. Trusts reported their arrangements for increased support to care homes through dedicated teams (e.g. Care Review and Support Teams, Link Workers) and named individuals. For instance, the Southern Trust held weekly Zoom conferences with ISP Care home representatives to disseminate guidance and take feedback, which in turn was shared in weekly meetings with key stakeholders - the DoH, PHA, HSCB, RQIA and Trust Regional Directors.
369. The HSCB described how it co-ordinated and standardised Trust activity to support individual care homes, using existing professional networks, and worked with the PHA on the Regional Surge Plan. The PHA advised that, in its view, 'the established relationships between care homes and Trusts provided a firm foundation that enabled emergency measures to be put in place rapidly and often without the usual engagement and attention to co-production that we would aspire to.' The PHA also referred to pre-pandemic efforts to establish Care Homes Support Teams home through the Trusts, and the provision of engagement workshops within each Trust and Care Home Provider with the aim of identifying a range of priorities that would enhance patient and resident care.
370. Both the IHCP, which represents the private care home sector, and COPNI voiced concerns around the resourcing and implementation of Surge plans. COPNI commented that 'It is clear much planning and preparation has gone on within the HSC organisations. It is not always clear how plans will be implemented; whether there will be sufficient resources to ensure robust implementation (both human and financial).' The IHCP commented that 'We are concerned that the resourcing and funding to deliver on the surge plan is not in place across all stakeholders.'
371. Engagement across the HSC and stakeholder organisations was a recurring theme in terms of pandemic management, as reflected in various sections of this report. Positive Futures said there was a lack of a joined up approach to pandemic planning for the social care sector, stating 'From where we sit, each part of the HSC system e.g. HSCB, Trusts and the Department, appear to be operating in their own silos. There appears to be a lack of accountability and clarity around roles and responsibilities and little evidence of a joined-up approach to the management of COVID-19.'
372. A number of organisations and representative bodies outlined the particular challenges they faced around stakeholder engagement to develop Surge Plans and communication and the subsequent dissemination of advice and operational guidance of those Plans. Indeed, the Department of Health led RLI, acknowledged the need for guidance to be clear and consistent.
373. In evidence given to the Committee in March, the IHCP alluded to the fact that the Department had not at that stage engaged with providers on surge plans and stressed how important it was for them to be included. In later evidence, the Chief Executive referred to the Care Home Surge Plan as the Department's overarching document which connects all stakeholders in the safe and effective management and delivery of care, and emphasised the need for the providers' views to be addressed. IHCP welcomed that the Health Minister had spoken about equal partnership, saying from their perspective 'there is merit in engaging with care home owners earlier in looking at possible solutions, because those people working on the ground know whether or not things actually work.'
374. IHCP cited the need for timely and consistent guidance to be applied across the Healthcare Trusts, the PHA, the RQIA and the DoH. On occasion they only received notification of plans via receipt of press releases and did not have the opportunity to input to proposals in advance. Furthermore, they called for a 24/7 answer service and clear points of contact to answer questions from the sector promptly.
375. UNISON, which represents the majority of staff in private care homes, described engagement as 'sporadic and inconsistent at points.' Examples of this included the 'Safe at Home' pilot which involved staff living at or near the care home for a period; also the Care Partners Initiative, which, according to both UNISON and the RCN, appeared in guidance without prior consultation. Consequently, UNISON called for strengthened and sustained engagement prior to future policy being developed.
376. NIC ICTU said the voice of unions should be heard more fully in long-term strategic decision-making, and expressed concerns around the Department's level of engagement with the unions and the workforce on the newly established Health and Social Care Management Board.
377. In consideration of evidence by the Trusts, Belfast Trust pointed out it would have welcomed further consultation around key decisions and timely communication, with appropriate lead-in times, highlighting that the first wave of the pandemic saw policy decisions and guidance issued at short notice. On a practical operational basis, it said key changes requiring urgent action across the sector should be avoided at the end of the week, as implementation fell to a reduced complement of staff at weekends.
378. HSCB considers that the size and variability within the care home area made communication with front line staff very challenging. Moving forward, it believed there was a need to develop alternative clear lines of communication that enable front line staff to contribute more effectively to strategic planning and decision making.
379. With regard to relatives' concerns, limited communication with families was a recurrent theme, cross-cutting all areas examined by the Committee in this inquiry, that led to particular frustration and distress. Both families and representative organisations expressed concern about the lack of information available from care homes on residents' health and wellbeing, especially with restrictions on visiting. The evidence provided to the Committee by the PCC and referenced in the visiting section of this report, makes a number of suggestions for care home providers to create and sustain ongoing regular engagement and communication with families.
380. The Committee also heard evidence around the potential longer-term impact of the pandemic and sectors particularly badly affected.
381. Drawing attention to the impact on mental health, the RCPsych stated that 'in the longer term, the COVID-19 pandemic has been a significant source of stress, anxiety and trauma to Northern Ireland society. Citizens lived with the actuality or fear of life-threatening illness, separation from loved ones and, in too many cases, grief, in partial or total isolation. The effect of this trauma will require many years to fully manifest itself and be fully understood.' This was echoed by Age NI, who said that 'bereavement and mental health support for staff, other residents and staff should continue to be resourced and promoted.'
382. The Alzheimer's Society expressed concerns that those living with dementia have been disproportionally affected by issues in care home with devastating consequences, and called for the Department of Health's Surge Planning Strategic Framework to show how people living with dementia have been accommodated.
383. Issues explored around scaling up testing and contact-tracing, set out in other sections of this report, also pointed to lessons for the longer term.
Infection Prevention and Control
384. In addition to issues documented earlier in relation to access to PPE, the Committee also asked questions about pandemic stores of PPE and heard evidence on lessons learned around infection prevention and control.
385. In particular, the Committee asked how the Department had responded to recommendations from Nervtag45 in terms of stockpiling PPE between 2016 and 2020. In its response, the Department advised that the Nervtag recommendations were made in preparation for an influenza pandemic, and were responded to directly by DHSC, with each of the devolved regions having an opportunity to review the volume of supply for its own jurisdiction. The IHCP expressed frustration to the Committee around the sourcing of PPE, which it considered failed to take account of the sector's needs. Also, the HSCB commented that the standards for Infection Prevention Controls for care homes that were initially applied were not sufficient for COVID-19.
386. Furthermore, the Belfast Trust said that IPC was not adequate in some areas in care homes, e.g. the majority of care homes lacked automated washers for effective decontamination of toileting equipment, or industrial standard laundry machines, capable of appropriate laundry disinfection at lower temperatures, and noted that the wrong gloves were sometimes used for personal care. They outlined the benefit of all homes having a dedicated IPC staff member. The South Eastern Trust had in fact dedicated two senior IPC nurses to provide support, supplemented by a team member from the PHA. In turn, their IPC nurse worked closely with the Trust Link Worker, whose role it was to provide ongoing advice and support to care home managers.
387. The NI Hospice shared in its evidence the measures it took on infection prevention control, to protect patients, visitors and staff. These included rigorous cleaning procedures for staff, to take account of all equipment used, or that they had come into contact with, all areas accessed such as office space, showers and other personal facilities. Also, a secure cohort of four beds was created for COVID-19 positive patients. Staff working in that zone did so in 12-hour shifts and worked in pairs to assist with 'donning and doffing' PPE.
388. The RLI report acknowledged there is no recognised regional training on environmental cleanliness and recommended that care home staff be provided with a 'freely accessible regional IPC training e-learning module'.
389. The PCC reported that a number of families had asked why HSCTs could not train families in the use of PPE to support visiting and infection control as they were willing to do so but this had not been put forward as an option.
Benchmarking with other countries
390. The Committee heard from international academics who described how other countries, particularly Hong Kong, had prepared for a pandemic. Professor Ben Cowling advised that, as Hong Kong had experienced a SARS outbreak in 2003, there was an enormous investment in preparation for any future pandemic. He described how, since 2003, hospitals stepped up their infection control and laboratories increased capacity to carry out more testing. He reported that the Centre for Health Protection in Hong Kong, has built capacity in infectious disease epidemic control, through contact-tracing, and wider quarantining, e.g. of people who are contacts of cases, which has all contributed to Hong Kong's success in controlling COVID-19. In addition, Hong Kong also had stockpiles of PPE, and staff who were very well trained in using it. Significantly, he advised that ever since SARS in 2003, enormous attention has been paid to infection control in hospitals, care homes and other parts of the community. In elderly homes, they have designated staff for infection control, which has been important in controlling the spread of COVID-19.
391. The Committee is aware that representative bodies, in giving evidence on Care Homes, made reference to other settings. Consideration of pandemic preparedness and infection control in the wider community is out-with the scope of this inquiry, though the potential read-across from this report is recognised. The Chief Executive of the IHCP drew attention to the overlap in the care home and homecare sectors in terms of forward planning. Age NI highlighted that most older people are cared for in their own homes and rely on care staff and families to help them retain their independence. It described COVID-19 as exposing difficulties inherent in the planning, commissioning and delivery of social care to the most vulnerable in society. Positive Futures raised concern that there had been no specific guidance for the Learning Disability sector saying 'in the absence of any specific guidance, our sector has had to find its own way through a myriad of, on many occasions, conflicting advices and guidance, to put in place guidance appropriate to the services which we provide.'
Systemic Issues
392. The Committee heard evidence that systemic failings in healthcare provision were considered to have been exposed and exacerbated by the COVID-19 pandemic.
Reform of adult social care
393. UNISON stated that the Power to People report published by the Department in 2017 had 'raised significant concerns about a social care workforce that was underpaid, undervalued and exploited.' RCN underscored this perspective, referring to their 2015 paper which had warned about the viability of nursing homes due to staff shortages, an issue which had deteriorated further since that time, according to RCN in evidence to Committee. The RCN further pointed out that patients in nursing homes have much more complex needs than was previously the case, arguing for a review of the skill-mix in homes between registered nurses and healthcare assistants. Age NI said 'We need to encourage people coming out of university into the social care field to feel that they are in a valued, valuable and caring profession, and we do that by structuring the workforce and career paths to show the value. '
394. Furthermore, Age NI made reference to the lack of integrated systems of health, care and support; an undervalued workforce; reliance on family carers; complex eligibility criteria on accessing and charging for social care support; and the need to progress work on the 'true cost of care'.
395. The Committee is cognisant that the Department had already embarked on reform with the establishment of the Expert Advisory Panel and the publication of the Power to People Report. Many of the issues identified by stakeholders in their evidence, such as staff shortages, underfunding and lack of training are addressed in the Report, and the Minister has accepted the need for progress on these matters to be expedited. Both UNISON and RCN referred to the Minister's acknowledgement on 13 May 2020 that: 'The social care sector has been struggling for years and as a whole is not fit for purpose.'
396. The CSW expressed his view that 'social care is an essential component of health and social care and should be valued in its own right, but it is also inextricably linked to the performance of our healthcare system. The sector has experienced many years of underinvestment. We really have to revisit our
attitude, our approach and our funding to the sector.'
397. On 13 May, the Minister announced new measures to support care homes. One of the three key commitments given was on investment and reform and the Minister said he was finalising a paper to Executive: 'I am therefore proposing to move ahead with reform and investment plans, subject to the necessary financial support being provided by the Executive. As an early priority, I want to see training and terms and conditions for care home staff being standardised and improved.'
Consideration of Human Rights
398. The consideration of human rights was a key issue emerging throughout the evidence, particularly with regard to the rights of the individual in relation to visiting and testing and also within advance care planning. This was especially pertinent to those care home residents with cognitive impairment.
399. In its evidence, the RCPsych said further clarity is required around the recently introduced Deprivation of Liberty Safeguards (DOLS) of the Mental Capacity Act 2016 to address concerns regarding, for example, patients who are incapable of self-isolation through choice or cognitive or other problems, or those who decline testing, or are incapable of consenting to testing.
400. The RCPsych also said that certain aspects of capacity assessment are resource-dependent (e.g. translation services, optimising communication and assessment) and suggested that the ability to provide these safely and effectively during pandemic conditions should be considered.
401. The Committee wrote to the NIHRC seeking its advice on issues around consent and testing; the advice46 outlined the human rights engaged and the need to balance rights effectively to take into consideration the risk of serious illness or death from the virus versus the invasive and unpleasant nature of the test.
Findings and Recommendations
Visiting
402. The Committee heard compelling evidence around the importance of family contact with residents; the negative and sometimes traumatic impact of visiting restrictions on the physical and mental wellbeing of residents – and on the mental health of carers; and the vital role families play, in the care of their loved ones.
403. Members recognise that facilitating safe visiting is closely linked to issues around testing and PPE; and that there are resource implications. The Committee welcomed indications that the latest funding could be used for infrastructure upgrades including the installation of visiting pods.
404. The Committee was struck by how frequently communication issues were raised across the various strands of the inquiry but particularly in relation to decision-making around visiting. Members were moved by testimony given by family members at an informal meeting, where they described the impact of recent months on their loved ones and their families and the lack of input they had into decisions around visiting.
405. It is noted that the most recent guidance on visiting confirms that care home managers are expected to make decisions based on a dynamic risk assessment of conditions in their community, taking account of the guidance.
406. Evidence gathered by the Committee also highlighted, however, that individual circumstances including health needs, determine what is feasible and desirable in terms of visiting. For some residents with cognitive decline, or significant sensory impairment, virtual visiting is simply not workable.
Recommendations
Recommendation 1: The Committee recommends that safe and meaningful visiting be facilitated and resourced through the identification, development and implementation of innovative measures.
Recommendation 2: The Committee recommends that residents and families be involved directly in decision-making around visiting, to ensure that the particular needs and circumstances of each resident is considered, including their, and their family's, attitude to risk.
Recommendation 3: The Committee recommends further work in the area of messaging and communication around visiting, COVID-19 outbreaks in homes, including direct communication with families in respect of their loved ones and wider developments affecting the home in which their family member resides.
Recommendation 4: The Committee calls for the implementation of the care partner initiative to be expedited, supported by urgent work with unions and providers to resolve issues raised, including safeguarding, insurance, role specification and testing.
Recommendation 5: PPE must be provided as required to facilitate safe visiting.
Recommendation 6: The Committee recommends that the implementation of visiting guidance be monitored across care homes to ensure consistency and compliance with best practice.
Testing
407. The Committee noted that the context had changed significantly since the outbreak of the pandemic, in terms of testing capacity, increased frequency of testing, regular symptom-monitoring and new approaches.
408. Members also recognised, however, the resource implications of increased testing, in terms of the impact on staff time and additional training requirements.
409. Consistent with the findings of the Rapid Learning Initiative, the Committee was concerned by evidence that care homes do not necessarily have all the required equipment, or adequately trained staff, to undertake symptom- monitoring in line with guidance.
410. The Committee sought particular advice on human rights and consent issues in respect of testing, in view of the frail health of many residents, particularly those with cognitive impairment. Members noted the competing rights at stake due to the potentially lethal nature of the disease but hopes that new, rapid tests hold out the hope of a less invasive means of keeping residents safe.
411. At the time of writing, the Minister was seeking to introduce mass and rapid testing and roll out the vaccination programme, which the Committee sees as having transformative potential, particularly given the high numbers of asymptomatic cases.
Recommendations
Recommendation 7: The Committee recommends that, subject to rapid testing becoming available, care home workers should be tested daily47; those moving between homes be tested before entry to any home; and residents should continue to be tested as frequently as necessary and at least fortnightly.
Recommendation 8: Testing should be extended to all those entering care homes including visitors, care partners, residents returning from an external appointment, and all professionals entering homes; and should take place as often as necessary to take advantage of improvements in testing capabilities.
Recommendation 9: The Committee recommends that local capacity to undertake testing and process results should be increased to improve timeliness of results.
Recommendation 10: Pooled testing48 should be explored as a means of enhancing testing capacity.
Recommendation 11: Access to, and training in the use of, appropriate clinical equipment should be provided as a priority, to facilitate effective twice-daily symptom-monitoring; and compliance with guidance on symptom-monitoring should be included in regular checks.
Recommendation 12: Further research should be undertaken to establish the means by which the virus is getting into homes, whether via staff or deliveries etc.
Recommendation 13: The Committee recommends that further consideration be given to the capture and analysis of testing data, such as asymptomatic positive tests, to inform the pandemic response.
Recommendation 14: Guidance should be reviewed to ensure consideration of human rights issues around testing.
Discharge Policy
412. The Committee remains concerned that the discharge of COVID-19 positive patients to care homes presents an enduring risk, though it is also cognisant of the pressures on hospital beds and the challenges of providing isolation via step- down care, including the additional disruption and distress this could cause.
413. Members discussed the evidence that many homes struggle to isolate individuals, either for reasons of facilities and adequate staff resource or, equally importantly, residents' wellbeing and issues of understanding amongst the significant numbers of residents with cognitive decline.
414. The Committee noted with concern, research suggesting increasing recognition of the danger of discharging people directly from hospital into care homes, without ideally two negative tests within 24 hours, due to the risk of false negative tests, even in the case of those not originally hospitalised for COVID-19.
415. While it is hoped that news of vaccines and rapid-testing will transform the situation, in addition to twice-daily symptom monitoring, the Committee nevertheless makes the following recommendations.
Recommendations
Recommendation 15: The Committee recommends that no-one be discharged from hospital to a care home in which they are a resident, without having tested negative for COVID-19, unless the care home confirms that it has the staffing and facilities to ensure isolation for the required period; and that this is subject to monitoring and review.
Recommendation 16: New residents should not be admitted to a care home unless they have tested negative.
Recommendation 17: The Committee recommends that the potential benefits of step-down isolation facilities be explored.
Access to PPE
416. The Committee heard persuasive and consistent evidence of shortages of appropriate PPE in the early months of the pandemic, which caused real anxiety for staff. Independent providers struggled to source their own PPE given vast price increases and global pressures on supply. There were also concerns about communication and consistency across the HSC but, by May, stakeholders were reporting significant improvements, including the establishment of a single point of contact with Trusts, revised guidance on PPE use, as well as centralised procurement and provision free of charge to care homes, in line with practice in other countries identified in research.
417. The Committee welcomed these initiatives and the continuing, but temporary, commitment to carry on providing PPE without charge, but acknowledges that there is a longer-term question to be considered about procurement and payment, given increased cost-burden to providers and the additional PPE requirements associated with facilitating safe visiting, as considered elsewhere in this report.
418. Effective use of PPE has required additional training, consideration of changing areas and is linked to oversight of infection prevention and control49, more generally. It also begs questions about how to overcome adverse effects such as the additional challenges entailed in residents not being able to see the faces of loved ones and those who care for them, a particular issue for those with hearing impairment or cognitive decline. Guidance has been produced but further research may be beneficial.
Recommendations
Recommendation 18: The Committee recommends that during a pandemic, there should be centralised procurement and supply of PPE to care homes, without charge.
Recommendation 19: Further charges for PPE should not be imposed care homes without a review of the tariff.
Recommendation 20: Training remains critical and all staff should be able to access regular and prompt updates as new knowledge or innovations emerge.
Recommendation 21: Consistency in the use of PPE should continue to be monitored.
Funding
419. The degree to which COVID-19 exacerbated the pre-existing financial strain on the care home sector, is well documented. The pandemic response resulted in increased staffing costs, enhanced cleaning and other infection-control measures; and costs associated with facilitating visiting.
420. The Committee welcomes the Department's initiatives to support care homes including through block-booking of vacant beds; offering staff support from the HSC and providing significant additional funding allocations.
421. Questions remain, however, about the criteria and processes for making claims and the Committee was concerned to hear of significant under-spends as a result, but welcomed news that the Department was seeking to address these issues in relation to the latest tranche of funding allocated in October.
422. Consistent with other sections of this report, there is a sense that earlier and more intensive engagement with stakeholders in advance of making decisions, may have averted some of the difficulties.
Recommendations
Recommendation 22: The Committee recommends that streamlined processes be developed for administering funding, subject to audit and verification, but flexibly enough to allow care homes to meet their particular needs.
Recommendation 23: Funding for adult social care should be considered as a whole, including care packages and day-centre capacity which impact on care home pressures and bed-flow across the system.
Recommendation 24: The Committee recommends that work be prioritised to establish the 'true cost of care' as part of wider reform.
Staff Terms and Conditions
423. The Committee wishes to acknowledge the skill and value of the work in care homes; the particular personal qualities shared by many for whom it is a vocation rather than a job; and the need to look at recognition, reward and retention in what is a challenging environment.
424. Members also acknowledge the toll the pandemic has taken on staff in terms of their own health and wellbeing, including mental health, and welcomed the extension to care home staff of access to the Trusts' mental health helpline.
425. There was also recognition of the differing financial impact that new requirements might have on care homes, given the variation in size and profitability; and acknowledgement that viability was in question in some cases. It is accepted that several recommendations may require a review of the tariff.
426. The Committee agreed that staff terms and conditions in the sector were problematic prior to the pandemic and that the lack of guaranteed sick-pay for many was not only unfair to staff but constituted a risk to wellbeing of staff and residents. Members therefore welcomed the Minister's decision to provide funding for sick-pay, noting with concern, however, that it was not back-dated to the start of the pandemic.
Recommendations
Recommendation 25: The Committee welcomes the Minister's commitment to progress reform urgently and calls for low pay and poor terms and conditions to be addressed as quickly as possible.
Recommendation 26: The Committee recommends that the Department set minimum standards for sick-pay in care home workers' contracts and that arrangements be put in place to ensure standards are adhered to.
Recommendation 27: In the interim, the Committee recommends that any additional funding provided to care homes should include conditions regarding fair pay and treatment.
Recommendation 28: The Committee recommends consideration of additional measures to make social care a more attractive career, including developing career pathways.
Staff Levels and Issues
427. The Committee recognises that staffing levels were a significant problem prior to the pandemic and heard repeatedly throughout recent months how this was exacerbated due to sickness absence, self-isolation, lack of childcare facilities during the first lockdown, and added caring responsibilities as day-centres were also closed.
428. In addition, the Committee heard convincing evidence of the greater demands placed on staff time for a range of reasons including testing, symptom-monitoring, increased IPC measures and additional care requirements as residents became unwell.
429. The use of agency workers, while unavoidable given the stated pressures, raised concerns about increased risk of transmission through staff movement between homes. The Committee acknowledged that its survey provided some encouraging evidence that this risk was recognised and that managers had sought to minimise staff movement between homes.
430. The Committee welcomed the support offered by Trusts to care homes, in terms of re-deploying HSC staff, but it was recognised that this created difficulties in the HSC. The service was also suffering pre-existing workforce shortages and was struggling in the second wave, given additional efforts to maintain HSC services, in tandem with the COVID-19 response.
431. Other initiatives were also welcomed such as regulatory change to facilitate rapid recruitment, subject to safeguards, and flexibility in staffing ratios, introduced by RQIA, as well as an app to allow RQIA to monitor staffing requirements across homes.
432. While additional training was made available and was welcomed, the Committee noted that in some cases, the pressure was such that staff could not be released to attend.
Recommendations
Recommendation 29: The Committee recommends that appropriate staff ratios for care homes be agreed in discussion with stakeholders.
Recommendation 30: Strenuous efforts must continue to be made to minimise staff movement between homes and, where possible, agency staff should work at one home only.
Recommendation 31: The Committee recommends that care home providers be required and supported to put in place robust measures to ensure the safety of BAME staff and other staff at increased risk from the virus.
Access to Health and Social Care
433. The Committee has been impressed with the rapid innovation and scaling up of the use of technology, to provide safe, timely and effective care during the pandemic; and acknowledges the enormous effort and dedication that this has required across the system.
434. Nevertheless, the Committee also recognises that there are limits to approaches such as 'virtual ward-rounds' and that, moving forward, the balance can be improved in terms of in-person care and also communication with loved ones who would ordinarily have been more closely involved in care.
435. The Committee was concerned to hear of the adverse impact on residents, of reduced access to podiatry, occupational health and other care. Evidence suggests one reason in-person access was limited, was due to inconsistent implementation of Departmental guidance which advises that appointments should continue where the relevant HSC professional deems it appropriate.
436. The Committee welcomes the ongoing work being led by the Chief Nursing Officer on an Enhanced Clinical Care Framework for care homes, including medical, nursing and multi-disciplinary care, to meet the higher degree of healthcare needs within care homes in recent years.
437. Advance Care Planning is another issue that was brought to the Committee's attention in recent months and the Committee acknowledges the sensitivity of such conversations and the importance of this matter being dealt with on an individual basis, supported by the appropriate professional and taking account of the unique needs, preferences and changing circumstances of the individual, ideally well in advance of a crisis. The Committee also notes that ACP goes well beyond circumstances where resuscitation is appropriate and covers a wide range of care and treatment preferences, in a variety of circumstances. The Committee notes the pressure felt by some care home staff to lead these important conversations for which they felt further training and medical input was required.
Recommendations
Recommendation 32: The Committee recommends that the Enhanced Clinical Care Framework should embed the principles of the acute care at home programme within care homes and should confirm GP participation.
Recommendation 33: There is a need for consistent implementation of the policy on in-person access to care homes, as deemed necessary by the HSC professionals concerned, and subject to testing and PPE requirements.
Advance Care Planning
Recommendation 34: Advance Care Planning should be discussed with each care home resident, on an individual basis, ideally ahead of any crisis; it should be led by the clinician who knows the individual best, with the input of other relevant professionals; and reviewed as necessary.
Recommendation 35: The Department of Health should clearly outline and communicate the rights of older people and families regarding end-of-life planning and this should reference the approach to treatment and care planning recommended under NICE guideline NG163.
Recommendation 36: Steps should be taken to ensure that relevant professionals have access to appropriate training in advance care planning.
Regulation
438. When it emerged in the spring that the Department had instructed the RQIA to suspend routine inspections and increase its emphasis on support and advice, the Committee considered the balance between regulation and assistance, enquiring about oversight, enforcement and shared characteristics of homes experiencing outbreaks.
439. The Committee recognises the strength of evidence expressing appreciation for the support and advice provided by RQIA, particularly during the first difficult months of the pandemic, including a first point of contact 'Service Support Team' and on-site support teams assisting homes to improve IPC. This is mirrored by concerns about the scaling back of the advice service during the autumn, as RQIA sought to increase inspections.
440. Members also acknowledge, however, concerns raised by stakeholders about the risks inherent in the lack of oversight when in-person inspections were reduced, particularly as it coincided with visiting restrictions. While some in- person inspections and virtual inspections continued, the Committee notes that virtual inspections were described as creating a greater administrative burden on homes, at a difficult time.
441. RQIA research identified a number of key characteristics associated with homes most at risk of an outbreak, including: larger homes (40+ registered places); homes run by larger providers; homes located in urban areas; services with more than two manager changes over the past year; and services registered within past 10 years. The Committee welcomes the RQIA's proposed move to a 'risk-based assurance framework' and the Minister's desire to see "change brought about so that, rather than just looking at an individual facility, a corporate provider can be inspected corporately".
442. Many stakeholders complained to the Committee of a lack of consistency in the implementation of Departmental guidance by care homes, convincing the Committee that there is work to be done in this area of regulation, as found by the RLI. The Committee recognises the link between this matter and issues raised frequently around communication of guidance.
443. The Committee was concerned by the resignation of the RQIA board in June and their criticism of the Department's approach. The Committee sought changes to the terms of reference for the subsequent inquiry, which were agreed to by the Minister. In this context, the Committee welcomes the ongoing review of regulation announced by the Minister in June.
Recommendations
Recommendation 37: The Committee recommends that additional resource be provided to ensure that routine inspections continue, subject to appropriate PPE and testing, in tandem with a high level of dedicated advice and support for care homes, during a pandemic.
Recommendation 38: Additional monitoring is required to ensure the consistent implementation of guidance and policy.
Recommendation 39: The Committee believes there must be consequences for failures of care and recommends consideration of models by which quality and delivery of care, and adherence to guidance and best practice, could be linked to funding and considered in future contracting arrangements, including the capacity to recoup public funds where poor service has been evidenced.
Recommendation 40: The Committee recommends that further work be undertaken to improve communication of guidance across the different tiers of the system, including with unions.
Pandemic Preparedness and Systemic Issues
444. There was virtual consensus on a number of significant points in relation to pandemic planning. It is uncontested that care homes, and the HSC, were already dealing with workforce shortages, especially in key roles including care home staff and nursing. Neither is there any dispute in relation to the inadequacy of PPE supplies at the start of the pandemic and the impact of the time required to build up testing capacity.
445. While the Committee recognises the enormous pressure under which HSC and Departmental staff were working at all levels, and the considerable volume of guidance developed and advice put in place, communication and engagement issues were central to criticisms raised. The Committee was concerned to hear, on several occasions, that initiatives had been introduced without prior engagement with providers or unions. The Committee finds that this undermined confidence, as gaps and questions arose that could potentially have been addressed through co-design of the policies. Communication was also one of the key issues raised by families, as set out earlier, particularly in relation to visiting and regulation.
446. The pandemic has had knock-on effects on mental health which will endure for some time; further work is needed to understand and mitigate the effects of the pandemic on the longer-term mental health of residents, families and care workers.
447. The Committee also considered the human rights issues arising due to pandemic restrictions on visiting and testing, particularly in respect of those with cognitive decline. The Committee found a need for greater support for providers and HSC workers in this area, including clarity around implementation of Deprivation of Liberty Safeguards in a pandemic context.
448. Having had initial discussions on best practice internationally, the Committee is not persuaded from its engagement with the Department, that adequate measures are in place to engage with, and learn from, countries that benefited from previous pandemic experience and have dealt best with COVID-19.
449. The Committee finds that the pre-existing strains on adult social care highlighted in the 'Power to People' report, have been exacerbated by the pandemic and that reform is urgently needed to address the range of issues identified in this report, from staff terms and conditions to regulation, funding and the costs and benefits of public or private provision of this vital public service.
450. The Minister's commitment to progressing adult social care reform is acknowledged and the Committee looks forward to engaging further with the Department as reform progresses.
451. Finally, the Committee acknowledges the many other settings, outside the scope of this inquiry, which were similarly impacted by the pandemic, such as domiciliary care and day-centres and trusts that there may be some useful read- across from this report.
Recommendations
Recommendation 41: The Committee recommends that the requirements of care homes are central to detailed pandemic planning for the future, including PPE, infection control and visiting facilities.
Recommendation 42: The Committee recommends that consideration be given to having ring-fenced funding available that could be accessed quickly by care homes in any future pandemic.
Recommendation 43: The Department should consider how to maintain streamlined systems such that, in any future pandemic, funds could more quickly and easily be released, ideally by a single nominated body, on the basis of fair and transparent criteria, and appropriately back-dated to the start of the pandemic.
Recommendation 44: The Committee recommends that future pandemic planning should factor in the central procurement and supply of PPE to care homes.
Recommendation 45: Pandemic planning should include consideration of the particular needs of those with cognitive decline and this should inform dedicated guidance, on testing, ability to isolate, application of deprivation of liberty safeguards, meaningful contact with family and access to health and social care services not based in the care home.
Recommendation 46: Dedicated efforts should be made to gather and learn from the breadth of international experience of pandemic planning and management.
Recommendation 47: The Committee notes the finding of the RLI that there is no recognised regional training on environmental cleanliness and endorses its recommendation that care home staff be provided with a 'freely accessible regional IPC training e-learning module'.
Recommendation 48: Each home should be required to appoint a designated and appropriately trained staff lead (other than the manager) for IPC, including disseminating guidance and training, with support from PHA.
Recommendation 49: A database should be established of designated IPC lead staff in care homes and this should be integrated into the regulatory and monitoring framework.
Recommendation 50: Effective engagement is required with all relevant stakeholders, including providers, unions and families, with policies developed on a co-design and co-production basis.
Recommendation 51: Robust communication plans must be put in place and monitored, to ensure families are promptly informed of key developments regarding the home in which their loved one resides, including staff shortages, infection outbreaks, inspection findings and changes to relevant guidance.
Recommendation 52: Pandemic plans should include ensuring rapid access for care homes to a single point of contact for advice and support, accessible twenty-four hours per day, seven days per week.
Recommendation 53: Guidance should be developed on consideration of human rights during a pandemic, including the right of residents to visits and communication with loved ones; and best practice on managing testing and self-isolation.
Recommendation 54: Bereavement and mental health support for staff, residents and families will be required beyond the short-term and should be resourced and promoted as required.
Appendix 1 - Minutes of Proceedings
Please note that the links below contain extracts from minutes of proceedings which relate to the inquiry into COVID-19 and its impact on care homes. The full version of Minutes of Proceedings are available on the Committee's Minutes of Proceedings page.
Extracts of Minutes related to the Inquiry:
- 10 September 2020
- 17 September 2020
- 24 September 2020
- 8 October 2020
- 13 October 2020
- 15 October 2020
- 20 October 2020
- 22 October 2020 (Chief Nursing Officer and Chief Social Worker)
- 22 October 2020 (Independent Health and Care Providers)
- 22 October 2020 (Regulation & Quality Improvement Authority)
- 12 November 2020
- 19 November 2020
- 26 November 2020
- 3 December 2020
- 8 December 2020
- 15 December 2020
- 17 December 2020
- 14 January 2021
- 21 January 2021
Appendix 2 - Minutes of Evidence
Minutes of Evidence are written transcriptions of evidence sessions during Committee meetings. The following Minutes of Evidence contain evidence sessions relevant to the inquiry.
- 5 March 2020 - Reform of Adult Social Care and 'Power to People' Report: Department of Health
- 12 March 2020 - Minister of Health
- 19 March 2020 - Independent Health & Care Providers (IHCP) & Positive Futures
- 2 April 2020 - Minister of Health
- 2 April 2020 - Belfast Health and Social Care Trust
- 16 April 2020 - Public Health Agency
- 23 April 2020 - Minister of Health
- 7 May 2020 - COVID-19 Disease Response: Public Health Agency
- 14 May 2020 - Regulation and Quality Improvement Authority (RQIA)
- 14 May 2020 - Expert Panel
- 20 May 2020 - Minister of Health
- 21 May 2020 - Independent Health and Care Providers (IHCP)
- 3 June 2020 - COVID-19 Disease Response: Mr Robin Swann MLA, Minister of Health; and Professor Ian Young, Chief Scientific Adviser
- 4 June 2020 - Commissioner for Older People for Northern Ireland
- 11 June 2020 - Northern Ireland Committee - Irish Congress of Trade Unions (NIC-ICTU)
- 11 June 2020 - Safe at Home Pilot Project: Trade Unions
- 18 June 2020 - Royal College of Nursing
- 25 June 2020 - Chief Social Work Officer
- 23 July 2020 - Chief Nursing Officer
- 3 September 2020 - Minister of Health
- 24 September 2020 - Professor Ben Cowling
- 13 October 2020 - Commissioner for Older People for Northern Ireland
- 15 October 2020 - Public Health Agency and Department of Health
- 20 October 2020 - Trade Union Representatives
- 22 October 2020 - Chief Nursing Officer and Chief Social Work Officer
- 22 October 2020 - Regulation and Quality Improvement Authority (RQIA)
- 22 October 2020 - Independent Health and Care Providers (IHCP)
Appendix 3 - Written Submissions
- Age NI
- Alzheimer's Society NI
- Belfast Health and Social Care Trust
- British Association of Social Workers NI
- British Medical Association NI
- Commissioner for Older People for Northern Ireland
- Health and Social Care Board
- Independent Health and Care Providers
- Marie Curie
- Northern Health and Social Care Trust
- Northern Ireland Hospice
- Patient and Client Council
- Positive Futures
- Public Health Agency
- Regulation and Quality Improvement Authority
- Royal College of General Practitioners Northern Ireland
- Royal College of Nursing
- Royal College of Psychiatrists
- South Eastern Health and Social Care Trust
- Southern Health and Social Care Trust
- Western Health and Social Care Trust
Appendix 4 - RaISe papers
RaISe papers are briefing papers prepared by the Assembly's Research and Information Service (RaISe) at the request of Committees. The following papers were prepared to assist the Committee with its inquiry:
- COVID-19 and Care Homes – an International Perspective (Amended to include further analysis into discharge policy/ practice and public versus private care home settings) (PDF, 30 pages, 841KB)
- Results of the Survey undertaken as part of the Committee for Health Inquiry into the impact of COVID-19 on Care Homes (PDF, 5 pages, 620KB)
Appendix 5 - Department of Health memoranda and correspondence
- Public Health Agency / Health and Social Care Board - Northern Ireland COVID-19 Regional Action Plan for the Care Home Sector (September 2020 onwards) (PDF, 3 pages, 452KB)
- Department of Health News Release, 12 November 2020 - Research highlights decrease in discharges to care homes (PDF, 55 pages, 1.83MB)
- The Rapid Learning Initiative Into The Transmission Of Covid-19 Into And Within Care Homes In Northern Ireland - Report of the Task & Finish Group (PDF, 36 pages, 1.28MB)
- COVID-19: Guidance For Nursing And Residential Care Homes In Northern Ireland (PDF, 57 pages, 483KB)
- Minister of Health correspondence on Advance Care Planning policy, 03 December 2020 (PDF, 1 page, 41.9KB)
- Minister of Health correspondence regarding Discharge to Care Homes policy, 17 November 2020 (PDF 3 pages, 64.3KB)
- Visiting Guidelines (revised) including Summary - 23 Sept 2020 (PDF 37 pages, 487KB)
Appendix 6 - Additional papers considered by the Committee
- Northern Ireland Human Rights Commission (NIHRC) reply to the Committee regarding COVID-19 testing in care homes (PDF, 8 pages, 312KB)
- Pooled testing as an efficient approach for regular testing to protect residential care homes for the elderly - Benjamin Cowling, Martina McMenamin (HKU School of Public Health) (PDF, 2 pages, 147KB)
- The Impact of COVID-19 on Care Homes in Northern Ireland February 2020 to July 2020 - The Regulation and Quality Improvement Authority (RQIA) (PDF, 24 pages, 2.25MB)
You may re-use this publication (not including images or logos) free of charge in any format or medium, under the terms of the Open Northern Ireland Assembly Licence. To find out more about this licence visit: http://data.niassembly.gov.uk/license.aspx. This Report can be made available in a range of formats including large print, Braille etc. For more information, please contact:
Éilis Haughey, Clerk Committee for Health Northern Ireland Assembly
Room 419, Parliament Buildings Ballymiscaw
Stormont Belfast BT4 3XX
Telephone: 028 90 520348
Email: committee.health@niassembly.gov.uk
Twitter: @niahealth
Footnotes
1 Mr Jonathan Buckley replaced Mr Alex Easton with effect from 2 November 2020.
2 Mr Alan Chambers replaced Mr John Stewart with effect from 10 February 2020.
3 Ms Cara Hunter replaced Mr Colin McGrath with effect from 14 December. Mr McGrath replaced Ms Sinéad Bradley with effect from 23 March 2020.
4 Mr Pat Sheehan replaced Ms Jemma Dolan with effect from 16 March 2020.
5 This date was subsequently amended due to Committee business pressures.
6 Health and Social Care Board - Care Homes FAQ
7 NISRA Weekly Deaths Bulletin, 1 January 2021
8 i.e. on any day on which an individual works.
9 'Pooling samples means that testing may be conducted more frequently hence further reducing the time until the outbreak is detected. For instance, if the availability of tests dictates that screening staff across all nursing homes could be implemented monthly, pooling samples into groups of 4 would allow for weekly testing instead, and pooling samples of 14 would allow for testing every two days, using the same number of tests.' Benjamin Cowling & Martina McMenamin, Pooled testing as an efficient approach for regular testing to protect residential care homes for the elderly, HKU School of Public Health, September 2020.
10 See findings and recommendations on Pandemic Preparedness and Systemic Issues.
11 Health and Social Care Board - Care Homes FAQ
13 COVID-19: Regional Principles for Visiting in Care Settings in Northern Ireland
15 'Pillar 1' is the Northern Ireland testing system run by the HSC.
16 'Pooling samples means that testing may be conducted more frequently hence further reducing the time until the outbreak is detected. For instance, if the availability of tests dictates that screening staff across all nursing homes could be implemented monthly, pooling samples into groups of 4 would allow for weekly testing instead, and pooling samples of 14 would allow for testing every two days, using the same number of tests.' Benjamin Cowling & Martina McMenamin, Pooled testing as an efficient approach for regular testing to protect residential care homes for the elderly, HKU School of Public Health, September 2020.
17 Professor of European Public Health at the London School of Hygiene & Tropical Medicine and Research Director of the European Observatory on Health Systems and Policies.
18 Irish News, 11 June 2020, Seanín Graham, 'Hospitals were told to admit COVID-19 cases to care homes'
19 COVID-19: Guidance for Nursing and Residential Care Homes in NI, Sept 2020, Para 26.
20 Department of Health - Clinical Analysis Discharge Patterns HSC Hospitals Northern Ireland
21 Red / amber / green
22 COVID-19: Guidance for Nursing and Residential Care Homes in Northern Ireland
23 COVID-19: Guidance for Nursing and Residential Care Homes in Northern Ireland
24 Department of Health COVID-19: Guidance For Nursing and Residential Care Homes in Northern Ireland, 17 March 2020.
25 Correspondence from the Chief Executive of the IHCP to the Health Committee, 10 December 2020.
26 Department of Health - Minister underlines extensive programme to support care homes
29 Department of Health - Minister underlines extensive programme to support care homes
30 COVID-19 and care homes, an international perspective', RaISe research paper, September 2020 (updated October 2020).
32 COVID-19 and care homes, an international perspective', RaISe research paper, September 2020 (updated October 2020).
33 Social care will play vital role during severe Covid-19 challenges, Sean Holland, 18 March
34 The Establishment and Agencies (Fitness of Workers) Regulations (Northern Ireland) 2020.
35 Department of Health - Minister underlines extensive programme to support care homes
36 Department of Health - New Framework Planned for Nursing and Medical input to Care Homes
37 RCGP Top Tips for GPs Caring for Care homes.
38 Department of Health - Minister underlines extensive programme to support care homes
39 Department of Health - New Framework Planned for Nursing and Medical input to Care Homes
40 National Institute for Health and Care Excellence (2020), COVID-19 rapid guideline: Managing symptoms (including at the end of life) in the community. [NG163]
41 The Palliative Care in Partnership Programme is responsible for enhancing palliative and end of life care services across Northern Ireland. It includes representatives from NI's five Health and Social Care Trusts, the Department of Health, HSCB and PHA, NIAS, hospice and independent palliative care providers, community and voluntary sector representatives, ICPs, primary care representatives and service users and carers.
43 The Establishment and Agencies (Fitness of Workers) Regulations (Northern Ireland) 2020.
45 New and Emerging Respiratory Virus Threats Advisory Group.
46 See section on testing above and full text in Appendix 6
47 i.e. on any day on which an individual works.
48 'Pooling samples means that testing may be conducted more frequently hence further reducing the time until the outbreak is detected. For instance, if the availability of tests dictates that screening staff across all nursing homes could be implemented monthly, pooling samples into groups of 4 would allow for weekly testing instead, and pooling samples of 14 would allow for testing every two days, using the same number of tests.' Benjamin Cowling & Martina McMenamin, Pooled testing as an efficient approach for regular testing to protect residential care homes for the elderly, HKU School of Public Health, September 2020.
49 See findings and recommendations on Pandemic Preparedness and Systemic Issues.



