Committee for Health, Social Services and Public Safety - 2007-2011 Mandate
Report on the Health and Social Care (Reform) Bill (NIA 21/07)
Report on the Health and Social Care (Reform) Bill.pdf (2.54 mb)
Session 2008/2009
First Report
Committee for Health, Social Services and Public Safety
Report on the Health and Social Care (Reform) Bill (NIA 21/07)
TOGETHER WITH THE MINUTES OF PROCEEDINGS, MINUTES OF EVIDENCE
AND WRITTEN SUBMISSIONS RELATING TO THE REPORT
Ordered by The Committee for Health, Social Services and Public Safety
to be printed 13 November 2008
Report: 10/08/09R (Committee for Health, Social Services and Public Safety)
This document is available in a range of alternative formats.
For more information please contact the
Northern Ireland Assembly, Printed Paper Office,
Parliament Buildings, Stormont, Belfast, BT4 3XX
Tel: 028 9052 1078
Membership and Powers
The Committee for Health, Social Services and Public Safety is a Statutory Departmental Committee established in accordance with paragraphs 8 and 9 of the Belfast Agreement, section 29 of the Northern Ireland Act 1998 and under Standing Order 46.
The Committee has power to:
- Consider and advise on Departmental budgets and annual plans in the context of the overall budget allocation;
- Consider relevant secondary legislation and take the Committee stage of primary legislation;
- Call for persons and papers;
- Initiate inquiries and make reports; and
- Consider and advise on any matters brought to the Committee by the Minister for Health, Social Services and Public Safety
The Committee has 11 members including a Chairperson and Deputy Chairperson and a quorum of 5.
The membership of the Committee is as follows:
Mrs Iris Robinson MP (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan Mrs Carmel Hanna
Dr Kieran Deeny Mr John Mccallister
Mr Alex Easton Mrs Claire McGill1
Mr Tommy Gallagher Ms Sue Ramsey
Mr Sam Gardiner2
1 with effect from 20 May 2008 Mrs Claire McGill replaced Ms Carál Ní Chuilín.
2 with effect from 15 September 2008 Mr Sam Gardiner replaced Rev Dr Robert Coulter.
Table of Contents
Clause by clause consideration of the Bill
Minutes of Proceedings
Minutes of Evidence
Written Submissions
Written Evidence and other Correspondence considered by the Committee
List of Witnesses
Executive Summary
1. The stated purpose of the Bill is ‘to provide the legislative framework within which the proposed new health and social care structures can operate’. Prior to the introduction of the Bill the Committee heard evidence from a number of the organisations likely to be affected by the provisions. Following its introduction a total of 30 organisations responded to the Committee request for written evidence. The Committee took further evidence from a number of key organisations before undertaking a formal clause by clause scrutiny of the Bill.
2. During the clause by clause consideration the Committee raised a number of concerns with the Department including issues highlighted in the oral and written evidence to the Committee. The Committee agreed that it was content with clauses 2 and 3, clause 7, clauses 10 to 12, clauses 15 to 17, clause 19, clauses 22 to 35, and schedules 1, 3, 4 and 7.
3. The Department agreed to a proposal from the Committee to change the name of the ‘Regional Support Services Organisation’ to the ‘Regional Business Services Organisation’ in clause 14 and throughout the Bill. The Department agreed that the acronym “RAPHSW” be replaced with the term “Regional Agency” in clause 1 and throughout the Bill.
4. The Department accepted a number of amendments proposed by the Committee to clauses relating to consultation. It accepted amendments to clauses 4 and 6 relating to the requirement of the Department to consult in relation to its power to determine priorities and objectives and to issue directions. The Department agreed to strengthen the consultation provision in clause 5 on the production of a framework document for all health and social care bodies and the provision in clause 9 about consultation to be undertaken by the Local Commissioning Groups. The Committee welcomed the proposal by the Department to amend clause 8 to provide for joint sign-off of the commissioning plan by the Regional Board and the Regional Agency.
5. The Committee was divided on the merits of a separate regional agency for public health and social well-being set out in clause 12. Most members supported the proposed agency arguing that a much stronger public-health message is needed. A number of members argued that setting up a separate agency would create another layer of bureaucracy and that its functions could be dealt with by the regional board. The Department accepted drafting amendments to clause 13 relating to the functions of the regional agency.
6. The Department accepted an amendment to clauses 18 to strengthen the duty on health and social care bodies to take account of the views of the Patient and Client Council and an amendment to clause 20 about taking account of comments submitted in response to a consultation. The Department accepted an amendment to clause 21 to place a duty on trusts to exercise their functions with the aim of reducing health inequalities. The Committee had concerns around the principle of public-private partnerships and suggested the inclusion of a reference to ensuring the long term financial viability and value of any public-private partnership schemes. Following consideration the Committee agreed the clause as drafted. The Committee questioned the procedures for making subordinate legislation set out in clause 29 and after consideration agreed to the clause as drafted. The Department accepted a minor correction to schedule 2 and advised the Committee of drafting amendments to be made to schedules 2, 5 and 6.
Introduction
1. The Health and Social Care (Reform) Bill (NIA 21/07) (the Bill) was referred to the Committee for consideration in accordance with Standing Order 33(1) on completion of the Second Stage of the Bill on Tuesday 1 July 2008.
2. The Minister for Health, Social Services and Public Safety (the Minister) made the following statement under section 9 of the Northern Ireland Act 1998:
“In my view the Health and Social Care (Reform) Bill would be within the legislative competence of the Northern Ireland Assembly.”
3. The Explanatory and Financial Memorandum states that ‘the rationale behind the reform of the health and social care system is to put in place structures which are patient-led, patient-centred and responsive to the needs of patients, clients and carers as well as being more effective and efficient (releasing resources for investment in front line health and social care).’ The stated purpose of the Bill is ‘to provide the legislative framework within which the proposed new health and social care structures can operate.’
4. During the period covered by this Report, the Committee considered the Bill and related issues at ten meetings. The relevant extracts from the Minutes of Proceedings for these meetings are included at Appendix 1.
5. The Committee had before it the Health and Social Care (Reform) Bill (NIA 21/07) and the Explanatory and Financial Memorandum that accompanied the Bill.
6. On referral of the Bill to the Committee after Second Stage, the Committee wrote on 4 July 2008 to key stakeholders and inserted advertisements in the Belfast Telegraph, Irish News and News Letter seeking written evidence on the Bill by 22 August 2008.
7. A total of 30 organisations responded to the request for written evidence and a copy of the submissions received by the Committee is included at Appendix 3.
8. Prior to the introduction of the Bill the Committee was briefed by the Minister on 6 March 2008 about the proposals for the reform of the health and social care system. The Committee took evidence from the Health Promotion Agency on 22 May 2008 and evidence from the Institute for Public Health and the Northern Ireland Local Government Association on 19 June 2008 about the proposals. The Committee took evidence from the Mental Health Commission on 3 July 2008. Following the referral of the Bill for Committee Stage the Committee took evidence from Departmental officials on 11 September 2008 about the policy behind the Bill and its general provisions. The Committee took evidence from the Central Services Agency on 18 September 2008; from the Health and Social Services Boards, the Health and Social Services Councils, and the Regulation and Quality Improvement Authority on 25 September 2008; from the Royal College of Nursing, the British Medical Association (NI), and the Allied Health Professions Federation on 2 October 2008. The Minutes of Evidence are included at Appendix 2.
9. The Committee began its clause by clause scrutiny of the Bill on 2 October 2008 and concluded this on 6 November 2008 – see Appendix 2.
Extension of Committee stage of the Bill
10. On 3 November 2008, the Assembly agreed to extend the Committee Stage of the Bill to 5 December 2008.
Report on the Health and Social Care (Reform) Bill
11. At its meeting on 13 November 2008, the Committee agreed its report on the Bill and agreed that it should be printed.
Consideration of the Bill
12. The Department issued its ‘Proposals for Health and Social Care Reform’ for consultation on 18 February 2008 with a closing date for submissions of 12 May 2008. Following this consultation period, and prior to the introduction of the Bill, the Committee took evidence from a number of organisations. The Committee took evidence from the Health Promotion Agency and the Institute of Public Health in Ireland on 22 May 2008 and 19 June 2008 respectively. The Health Promotion Agency argued that public health and health improvement are complex issues that require collaboration and partnership working and that “current structures do not easily facilitate those partnerships or local working”. The Health Promotion Agency described the current restructuring proposals as offering “a major opportunity for change” and argued that “any proposed new organisations should make public health, particularly health improvement, a priority”.
13. The Institute of Public Health welcomed the proposed regional public health agency as “a major opportunity to bring together the different aspects of public health and to give public health a much stronger voice”. The Institute stated that “the agency must be multi-sectoral. Public health is not about just the health service, … but about other areas such as housing, education, agriculture, transport and rurality. This organisation must be outward looking and forward looking. There is here a fantastic opportunity to create in Northern Ireland something that is truly world class”. The Institute argued that “there must be strong links between the [regional health and social care] board and the proposed regional public health agency, but it is not clear how those links would be taken forward”. The Institute also called for the regional public health agency to have a stronger function relating to research and information.
14. The Northern Ireland Local Government Association (NILGA), in evidence to the Committee on 19 June 2008, welcomed “the proposals for a much stronger and closer role for local government” and said it would mean that “the local community will have ownership of the services, feel more involved, have better feedback, and enjoy an improved sense of well-being”. NILGA called for local government to be seen as “an organisation that, in conjunction with partners, can deliver health improvement. It has responsibilities for environmental health, heath improvement through the provision of leisure and open spaces, community development, good relations, economic development, and so forth”. NILGA also recognised that capacity building for local councilors needed to be addressed and that council members working on health bodies must be properly supported and briefed in their work. NILGA was strongly supportive of the proposal for a regional public health agency.
15. The Bill provides for the dissolution of the Mental Health Commission and the transfer of its functions to the Regulation and Quality Improvement Authority. The Committee took evidence from the Mental Health Commission on 3 July 2008. The Commission argued that it should be retained as a separate organisation but, recognising that this was unlikely, made a number of suggestions about how its functions, particularly those relating to the Mental Health (Northern Ireland) Order 1986, should be delivered within the Regulation and Quality Improvement Authority. The Committee took evidence from the Regulation and Quality Improvement Authority on 25 September 2008 when it reported that “over the summer we took a strategic approach on an operational level to discuss and plan how the services will come together, if the legislation comes into effect from 1 April 2009”. The Regulation and Quality Improvement Authority reported that the Authority and the Mental Health Commission established a project board to develop an action plan and full agreement has been reached on how the work in the action plan will be taken forward.
16. Departmental officials briefed the Committee on 11 September 2008 on the general provisions in the Bill. The Committee recognised the tight timescale to deliver the proposed changes by 1 April 2009 and noted that the purpose of the Bill is to provide a legislative framework for the proposed new healthcare structures. The officials explained that
“The Bill seeks, either in the body of the document itself or by securing the powers to make subordinate legislation, to establish parameters within which each of those health and social care bodies will be permitted to operate; what is expected of them; and the necessary governance and accountability arrangements that would support the effective delivery of health and social care in Northern Ireland.”
17. The officials reported on the outcome of the consultation and stated that there was broad support for the thrust of the proposals. They said that there was much support for the establishment of a regional board and a regional agency for public health and social well-being and indicated that the name of the regional agency “was chosen to try to get across the message that the agency will adopt a comprehensive approach to the public health and social well-being of the entire population”. They indicated that comment on the regional support services organisation was limited while there was “overwhelming support” for the proposed patient and client council model.
18. Officials reported that among the concerns raised during the consultation were the relationship between the regional board and the regional agency, representation of the voluntary and community sector, and the level of social care representation on the local commissioning groups. The Committee questioned the inclusion in the Bill of a provision relating to public-private partnerships and the officials explained that legal clarification on the issue was needed and stated that “It is simply a permissive provision, and it provides the legal clarity that a PPP scheme can be used if it is required and is judged appropriate in individual cases.” In response to a question about deficiencies in performance management identified in the Appleby Report the officials explained that a proposed definitive framework for performance management was being prepared and would be published shortly.
19. The Committee took evidence from the Central Services Agency on 18 September 2008. The Agency outlined its current role and indicated that its replacement by the proposed Regional Support Services Organisation would represent a natural progression with the new organisation providing a wider range of services. Among the additional functions which will move to the new body are the health and personal social services superannuation scheme, some payment functions relating to GPs, with ICT and IT services transferring in the medium term and, in the longer term, accounts services and human resources and recruitment are areas under consideration. The Central Services Agency made a case that the name of the new body should be changed to the ‘Regional Business Services Organisation’ to better reflect the business and business-support functions it will provide.
20. The Committee took evidence from the Health and Social Services Boards on 25 September 2008. The Boards welcomed the general thrust of the proposals and particularly the enhanced profile for public health and well-being. The Boards recognised that “there is a particular challenge in bringing together [those] different interfaces, particularly those between the regional health and social care board and the regional agency for public health and social well-being”. The Boards stressed the importance of the Framework Document under Clause 5 in providing the checks and balances on accountability between the various bodies.
21. The Committee also took evidence from the Health and Social Services Councils on 25 September 2008. The Councils welcomed the clear line of management responsibility in the structures from the Minister and the Department, through the commissioning board, and to the providing trusts. They stated that “the accountability of trusts to the regional health and social care board is a key strength of the proposed structures”. The Councils welcomed the creation of the patient and client council and recognised “the importance of having a single co-ordinated organisation to formulate and express diverse local views”. However, they also had some concerns about how local representation will be preserved and maintained.
22. The Councils argued that the regional agency for public health and social well-being should be accountable to the regional board. They acknowledged that concerns about the separation of functions between the two bodies had been addressed by the Minister’s “commitment to the production of a framework document that makes abundantly clear the respective functions and interrelationship of the new health and social care organisations”.
23. The Royal College of Nursing, in evidence to the Committee on 2 October 2008, supported “the Minister’s stated intention to put the public-health agenda at the heart of the health and social care system”. They shared the concern echoed by others that “how the local commissioning groups, the regional health and social care board and the regional agency for public health and social well-being work together is central to the delivery of those objectives”. They called for the language in the Bill to be strengthened and that “all plans should be signed off jointly by the local commissioning groups, the board and the agency. In that way no one body has primacy over the others. We believe that that will provide checks and balances that will help to ensure that good local decisions are made”.
24. The RCN welcomed the involvement of local voices in the commissioning of services but had some concerns about the weight that will be given to the local representatives and professionals involved. It stated “if commissioning is to be truly local, an agreed level of authority must sit with local commissioning groups; otherwise, groups will be relegated to no more that debating chambers”.
25. The British Medical Association (NI), in evidence to the Committee on 2 October 2008, strongly welcomed the establishment of a regional health and social care board and the slimming down of the Department but stressed that this reduction in bureaucracy must produce savings which will be released into front-line patient care. The BMA welcomed the creation of a new regional support services organisation but had concerns about the size of the organisation and particularly how it will be structured. The BMA also welcomed in principle the establishment of a regional agency for public health and social well-being but was “slightly concerned about the lack of clarity on how the organisations will communicate with one another”.
26. The BMA expressed major concerns about the top-down approach to managing commissioning and argued that “an opportunity will be lost if we create local commissioning groups, but ignore the potential for further development at a community level”. The BMA questioned whether the proposed local commissioning groups with populations of 300,000 would be so very different from the existing health boards and argued for structures to operate at a level of 50,000 patients or fewer. They recognised that under the proposed structure this is not precluded but would wish to see it encouraged. The BMA also expressed opposition to the inclusion of elected local representatives on the local commissioning groups arguing that if they are included “the scrutiny and accountability of local councils may be eroded”.
27. In evidence to the Committee on 2 October 2008 the Allied Health Professions Federation, while welcoming the creation of a single regional health and social care board, had reservations about the representation of allied health professions on the board. The Federation also welcomed “the emphasis that the regional agency for public health and social well-being will place on health promotion and protection”. The Federation expressed some concerns about the proposed commissioning arrangements. These included the need for the allied health professional on each local commissioning group to have access to adequate support and advice structures and the need for clarification on the extent of the financial controls. The Federation argued that “care is also needed to ensure that there is no duplication between the regional board’s role and that of the LCGs. … … Regional commissioning must have a local flavour – localities must have an input into what is commissioned regionally”.
Clause by clause consideration of the Bill
28. The Committee undertook its clause by clause scrutiny of the Bill on 2, 9, 16, 23 October and 6 November 2008 – see Minutes of Evidence in Appendix 2.
Clause 1 – Restructuring of administration of health and social care
29. The Committee raised two concerns relating to this clause. The first related to the use of the acronym “RQIA” in subsection (2)(b) and throughout the Bill to refer to the Health and Social Care Regulation and Quality Improvement Authority. The Committee suggested that “Health and Social Care RQIA” be used. However, following consideration the Department did not accept the proposal arguing that
“as the purpose of an acronym is to provide a shortened version of the full name, “Health and Social Care RQIA” is not felt to be appropriate. In addition, “RQIA” is a recognised and accepted acronym for the organisation and therefore it is considered that it should remain.”
After further consideration the Committee agreed to the use of ‘RQIA’.
30. The second concern related to the use of the acronym “RAPHSW” in subsection (5)(b) and throughout the Bill which the Committee considered cumbersome and unwieldy. Following consideration the Department proposed that “Regional Agency” be substituted for “RAPHSW”. The Committee agreed to clause 1 as drafted subject to the proposed amendment to subsection (5)(b).
Proposed amendment, clause 1(5)(b), “leave out ‘RAPHSW’ and insert ‘the Regional Agency’.
Clause 2 – Department’s general duty
31. The Committee agreed to clause 2 as drafted.
Clause 3 – Department’s general power
32. The Committee agreed to clause 3 as drafted.
Clause 4 – Department’s priorities and objectives
33. The Committee noted that clause 4 will make it a statutory requirement for the Department to determine its priorities and objectives for the provision of health and social care. The Department can revise those priorities and objectives but before doing so it must consult with such bodies or persons as it thinks appropriate. The Committee had concerns that section (3) releases the Department from the obligation to consult “where because of the urgency of the matter” it is necessary to act without consultation. The Committee proposed that the provision be modified by the inclusion of the word “extreme” before “urgency” and that where no consultation takes place a report will be submitted to the health and social care body concerned. Following consideration the Department did not accept the proposed inclusion of the word “extreme” arguing that
“this creates a difficulty in attempting to define and justify what type of situation is “urgent” as compared to one that is “extremely urgent”. In addition, the use of the term “extremely urgent” would mean that the Department would be required to consult in instances where the circumstances were just “urgent” and this would appear to defeat the purpose of the provision”.
After further consideration the Committee accepted section (3) as drafted.
34. The Department accepted the need for a report to be submitted to the health and social care body concerned where because of the urgency of the matter no consultation takes place and agreed to amend the clause accordingly. The Committee agreed to clause 4 as drafted subject to the proposed amendment to section (3).
Proposed amendment, clause 4(3), “leave out subsection (3) and insert:
(3) Where the Department is of the opinion that because of the urgency of the matter it is necessary to act under subsection (1) without consultation—
(a) subsection (2) does not apply; but
(b) the Department must as soon as reasonably practical give notice to such bodies as it thinks appropriate of the grounds on which the Department formed that opinion.”
Clause 5 – The framework document
35. The Committee noted that clause 5 provides a statutory requirement on the Department to produce a ‘framework document’ for all health and social care bodies. This is intended to clearly specify to each body what is expected of it and the procedures it must follow to perform certain functions. The Department is required to keep the document under review and to revise it as and when necessary. The clause also provides that the Department should consult with each body in respect of its functions and may consult with any other bodies that it considers appropriate. The Committee was concerned that the provision in subsection (5)(b) that the Department “may consult any other bodies or persons the Department considers appropriate” was too weak and proposed that ‘may consult’ should be replaced by ‘will consult’. Following consideration the Department accepted the proposal and agreed to amend the clause. The Committee agreed to clause 5 as drafted subject to the proposed amendment to subsection (5)(b).
Proposed amendment, clause 5(5)(b), “leave out ‘may’ and insert ‘’will’.
Clause 6 – Power of Department to give directions to certain bodies
36. The Committee noted that clause 6 will give the Department power to issue general or specific directions to the regional board, the regional agency and the regional support services organisation in carrying out their functions. The Committee had concerns that subsection (3)(a), similar to the provision in clause 4(3), enables the Department in cases of urgency to issue a direction without first consulting the health and social care body concerned. The Committee proposed similar amendments as in clause 4, that is, to insert ‘extreme’ before ‘urgency’ and to report retrospectively where action is taken without consultation. Following consideration the Department did not accept the proposal to insert the word “extreme” before the word “urgency” but did accept the need for a report to be submitted to the health and social care body concerned where because of the urgency of the matter no consultation takes place and agreed to amend the clause accordingly. The Committee agreed to clause 6 as drafted subject to the proposed amendment to section (3).
Proposed amendment, clause 6(3), “leave out subsection (3) and insert:
(3) Where the Department is of the opinion that because of the urgency of the matter it is necessary to act under subsection (1) without consulting the body concerned—
(a) subsection (2) does not apply; but
(b) the Department must as soon as reasonably practical give notice to that body of the grounds on which the Department formed that opinion.
(3A) Where the Department is of the opinion that (for any reason other than the urgency of the matter) it is not reasonably practical to comply with subsection (2)—
(a) that subsection does not apply; but
(b) the Department must as soon as reasonably practicable give notice to the body concerned of the grounds on which the Department formed that opinion.”
Clause 7 – The Regional Health and Social Care Board
37. The Committee noted that clause 7 establishes a Regional Health and Social Care Board to replace the existing four Health and Social Services Boards. The Committee agreed to clause 7 as drafted.
Clause 8 – Functions of the Regional Board
38. The Committee noted that this clause sets out the functions of the regional board which are chiefly those transferred to it from the existing four Health and Social Services Boards and any other function that the Department directs. The Committee also noted that section (3) requires the Board to draw up an annual commissioning plan and in doing so it must consult the Regional Agency and have due regard to the views of the Agency. Uncertainty about the relationship between the various bodies and particularly the Regional Board and the Regional Agency has been a recurring theme of the written submissions received by the Committee. The Committee acknowledges that to some extent those concerns may be addressed in the framework document to be drawn up under clause 5. However, the Committee recognises the importance of the role of the two main bodies in drawing up the commissioning plan. The Committee, therefore, welcomes the proposal by the Department to amend this clause to provide for joint sign-off of the commissioning plan by requiring the prior approval of the Regional Agency to the contents of the plan. The Committee agreed to clause 8 as drafted and supports the proposal to amend section (3) requiring the Regional Board and the Regional Agency to jointly sign-off the commissioning plan.
Clause 9 – Local Commissioning Groups
39. The Committee noted that clause 9 provides for the establishment of the Local Commissioning Groups and that the Department is proposing five such groups to align with the existing trust boundaries. The Committee raised concerns, highlighted by the Royal College of Nursing, calling for the provision in subsection (4)(b)(i) relating to consultation with the regional agency, to be strengthened. Following consideration the Department accepted the need to amend the subsection and has proposed a revised text. The Committee agreed to clause 9 as drafted subject to the proposed amendment to subsection (4)(b)(i).]
Proposed amendment, clause 9(4)(b)(i), “leave out ‘consult RAPHSW’ and insert ‘work in collaboration with the Regional Agency’.
Clause 10 – Power of Regional Board to give directions and guidance to HSC trusts
40. The Committee noted that clause 10 gives the Regional Board power to give directions to trusts about the carrying out of their functions. It also places a duty on trusts to comply with those directions. The Committee agreed to clause 10 as drafted.
Clause 11 – Provision of information, etc. to Regional Board by HSC trusts
41. The Committee agreed to clause 11 as drafted.
Clause 12 – The Regional Agency for Public Health and Social Well-being
42. The Committee noted that clause 12 provides for the establishment of a separate regional agency for public health and social well-being. A number of members questioned the merits of setting up a separate agency arguing that it creates another layer of bureaucracy, that it is contrary to the aim of creating more efficient structures, and that its functions could be dealt with by the regional board. Other members strongly supported a separate agency arguing that a much stronger public-health message is needed.
43. The Department explained that one of the driving factors underpinning the current reform proposals was the need to address existing inequalities in morbidity and mortality and that to do this the profile of public health and social well-being needed to be much higher up the agenda and issues dealt with in a more focused manner. The Department argued that
“another important issue was the need to develop improved partnerships, not only with local government but with the full range of public-sector stakeholders and others who have a strong influence and a role to play in improving public health and social well-being”.
On the question of whether these functions could be dealt with by the proposed regional board the Department argued
“if responsibility for public health and social well-being is to lie with a regional board that will inevitably be driven by the significant concerns and priorities that must be addressed, the prioritisation of funds specifically targeted at public health and social well-being can necessarily take second place”.
The Chief Medical Officer stated bluntly “In a single organisation the public-health agenda would disappear”. The Department pointed out that during the consultation 59% of those who discussed the issue of an agency were supportive, 20% were undecided and 21% were not supportive.
44. In response to concerns that the separate agency must not be a talking shop but must be able to make a difference the Department stated
“We are doing detailed work on the relationship between the board and the agency to ensure that the product of their work is an integrated commissioning plan, of which both have ownership, both approve and … which gives the agency not only direct input into the smaller amounts of money that it will commit but very significant influence over the £4 billion that the board spends in total.”
45. Following detailed discussion on the issue a proposal ‘that the regional public health agency be incorporated into the proposed regional board under clause 7’ was not carried. The Committee agreed to clause 12 as drafted. (For details of the divisions see the Minutes of Proceedings of 6 November 2008 in Appendix 1)
Clause 13 – Functions of RAPHSW
46. The Committee noted that clause 13 details the functions of the Regional Agency and that the agency will have both health improvement functions and health protection functions. The health improvement functions include the reduction in health inequalities and health promotion. The health protection functions relate to protection against communicable diseases and other wide ranging dangers to the health and social well-being of the public. The Committee raised three drafting concerns about the clause which were highlighted in written submissions. Disability Action called for subsection (2)(b) to be expanded to better outline the health promotion function while the British Red Cross asked for the same subsection to be strengthened by including a reference to ‘risk reduction’. Following consideration the Department accepted the proposal relating to health promotion but did not accept the inclusion of ‘risk reduction’.
47. The Association of the British Pharmaceutical Industry called for the Regional Agency to be required to consult the Committee for Health, Social Services and Public Safety about making ‘persons, materials and facilities’ available to other bodies. Following consideration, the Department did not accept this proposal pointing out that “to insert a provision to the effect that support services could only be provided to other bodies after consultation with the Health Committee would be a significant inhibitor to the day to day performance of functions and prove to be extremely bureaucratic”. The Committee accepted this argument. The Committee agreed to clause 13 as drafted subject to the proposed amendment to subsections (2)(b).
Proposed amendment, clause 13(2)(b), “after ‘health promotion’ insert “, including in particular enabling people in Northern Ireland to increase control over and improve their health and social well-being’.
Clause 14 – The Regional Support Services Organisation
48. The Committee noted that clause 14 establishes a regional support services organisation to replace the Central Services Agency and to undertake additional functions. The Committee noted that the Central Services Agency in its evidence made a case that the name of the new body should be changed to the ‘Regional Business Services Organisation’ to better reflect the business and business-support functions it will provide. The Central Services Agency also pointed out that the acronym RSSO could have unfortunate and unintended pronunciation. The Committee called for the name of the organisation to be changed and following consideration the Department agreed to amend the title of the body to the “Regional Business Services Organisation”. The Committee agreed to clause 14 subject to the proposed amendment to the title of the body.
Clause 15 – Functions of RSSO
49. The Committee noted that clause 15 sets out in broad terms the list of functions that the Regional Support Services Organisation is required to provide on behalf of health and social care bodies. The Committee raised an issue, highlighted by the Northern Health and Social Services Board, proposing that in subsection (3)(a) in relation to the securing the provision of services the word “equitable” should be included as well as “in the most economic, efficient and effective way”. Following consideration the Department did not accept the proposed amendment and argued that
“The RSSO, like all of the newly created bodies will be bound by existing legislative requirements of Section 75 of the Northern Ireland Act in relation to fairness to all. In addition, RSSO’s business is to provide a range of transactional and support services to a number of health and social care bodies. In most cases, the services it provides are in response to demand from those bodies and, as such, it would be difficult for RSSO to demonstrate that it will provide its services in an “equitable” way.”
The Committee agreed to clause 15 as drafted.
Clause 16 – The Patient and Client Council
50. The Committee noted that clause 16 establishes a new body to be known as the Patient and Client Council which will replace the existing four health and social services councils. The Committee was strongly supportive of the new council. The Committee agreed to clause 16 as drafted.
Clause 17 – Functions of the Patient and Client Council
51. The Committee noted that clause 17 sets out the four main functions of the Patient and Client Council, which include representing the interests of the public and promoting involvement by the public, as well as other provisions relating to how those functions are exercised. The Committee raised an issue relating to subsection (2)(a), highlighted by Disability Action, which proposes that the council should be required to consult the public “in an accessible way”. Following consideration the Department did not accept the proposed amendment and argued that the Disability Discrimination (NI) Order 2006 provides sufficient provision to ensure that public bodies consult in an accessible way.
52. Disability Action also questioned whether section (4) refers to reasonable adjustment under the Disability Discrimination Act or not. The Department advised that section (4) is about the Patient and Client Council making arrangements to the extent it considers necessary to meet all reasonable requirements to provide assistance to individuals making or intending to make complaints. As a public body bound by the provisions of the Disability Discrimination Act, the Patient and Client Council would be required to make any reasonable adjustment to meet any special needs in relation to disabled persons. Following further consideration the Committee accepted this explanation. The Committee agreed to clause 17 as drafted.
Clause 18 – Duty to co-operate with the Patient and Client Council
53. The Committee noted that clause 18 places a duty on health and social care bodies to co-operate with the Patient and Client Council. The Committee had concerns that the wording of section (6) – “a body to which this section applies shall have regard to any views expressed by the Patient and Client Council” – could allow the body to listen to the views but not necessarily act upon them. The Committee proposed that it be amended to “have due regard to”. Following consideration the Department accepted this proposal. The Committee agreed to clause 18 subject to the proposed amendment to section (6).
Proposed amendment, clause 18(6), “after ‘have’ insert ‘due’”.
Clause 19 – Public involvement and consultation
54. The Committee noted that clause 19 relates to public involvement in the planning and delivery of services and it places a duty on health and social care bodies to provide information, to obtain information on the needs of the population, and to encourage and assist people. The Committee raised an issue relating to subsection (1)(a), highlighted by Disability Action, which proposes that each body should be required to promulgate information “in accessible formats”. Following consideration the Department did not accept the proposed amendment for the reasons set out in relation to a similar issue at clause 17. After further consideration the Committee accepted the explanation. The Committee agreed to clause 19 as drafted.
Clause 20 – Public involvement: consultation schemes
55. The Committee noted that clause 20 requires health and social care bodies to show, in their consultation schemes, what arrangements are in place to consult with the Patient and Client Council and the recipients of health and social care. The Committee had concerns about the use of the phrase in subsection (3)(a) “to have regard to any comments” and proposed that, as in clause 17, this be amended to “have due regard to”. Following consideration the Department accepted this proposal. The Committee agreed to clause 20 as drafted subject to the proposed amendment to subsection (3)(a).
Proposed amendment, clause 20(3)(a), “after ‘have’ insert ‘due’”.
Clause 21 – Duty on HSC trusts in relation to improvement of health and social well-being
56. The Committee noted that clause 21 places a duty on each health and social care trust to exercise its functions with the aim of improving the health and social well-being of those for whom it provides care. The Committee raised an issue, highlighted by the Community Development and Health Network, which proposes that each trust should also have a duty to exercise its functions with the aim of reducing health inequalities. Following consideration the Department accepted the proposed amendment. The Committee agreed to clause 21 subject to the proposed amendment that after the words “the health and social well-being of” in line 2 is inserted the words “and reducing health inequalities between”.
Proposed amendment, clause 21, “after ‘of’ insert ‘, and reducing health inequalities between,’”.
Clause 22 – Public-private partnerships
57. The Committee noted that clause 22 relates to the forming of public-private partnerships to provide facilities or services for the promotion or provision of health and social care. The Committee expressed concerns around the principle of public-private partnerships. The Committee also proposed that the clause should include a reference to ensuring the long term financial viability and value of any schemes. The Department pointed out that this clause enables the new bodies to form or participate in forming Public-Private Partnerships but the existing DFP and Treasury guidance, which is binding on all organisations, makes it clear that the central concern of any procurement route is the achievement of value for money. The Committee agreed to clause 22 as drafted
Clause 23 – Schemes for transfer of assets and liabilities
58. The Committee agreed to clause 23 as drafted.
Clause 24 – Transfer of functions of Health and Social Services Boards
59. The Committee agreed to clause 24 as drafted.
Clause 25 – Transfer of functions of the Mental Health Commission
60. The Committee noted that clause 25 provides for the transfer of functions exercisable by the Mental Health Commission to the Regulation and Quality Improvement Authority. In oral evidence to the Committee the Mental Health Commission had expressed concerns about the proposed transfer but the Committee noted that in later evidence from the Regulation and Quality Improvement Authority the two organisations were working closely to implement the transfer. The Committee agreed to clause 25 as drafted.
Clause 26 – Transfer of functions of Central Services Agency
61. The Committee agreed to clause 26 as drafted.
Clause 27 – Amendment of statutory and other references to dissolved bodies, etc
62. The Committee agreed to clause 27 as drafted.
Clause 28 – Dissolution of special agencies
63. The Committee agreed to clause 28 as drafted.
Clause 29 – Orders, regulations, guidance and directions
64. The Committee noted that clause 29 deals with the procedures for making subordinate legislation under the Bill. The Committee also noted that subordinate legislation made under different procedures are subject to different levels of scrutiny and approval within the Assembly. The Committee asked what consideration had been given to whether the subordinate legislation should be subject to affirmative resolution or negative resolution. The Examiner of Statutory Rules provided advice to the Committee on this issue. The Department advised that
“Subsection (1) of the Clause provides that orders altering the functions of the proposed new Regional Agency (13(5)) and Regional Business Support Organisation (15(6)) and orders which include supplementary, incidental or consequential provisions to be used for expediency to give full effect to the Bill (30(1)) must use the affirmative resolution procedures. This is because it was considered that since such orders are akin to primary legislation and, therefore, more important and more likely to merit discussion they should be formally approved by the Assembly. The regulations and other orders which may be made principally relate to the day to day organisation of the various organisations and, therefore, considered more appropriate to the negative resolution procedure.”
The Committee agreed to clause 29 as drafted.
Clause 30 – Further provision
65. The Committee agreed to clause 30 as drafted.
Clause 31 – Interpretation
66. The Committee agreed to clause 31 as drafted.
Clause 32 – Minor and consequential amendments
67. The Committee agreed to clause 32 as drafted.
Clause 33 – Repeals
68. The Committee agreed to clause 33 as drafted.
Clause 34 – Commencement
69. The Committee agreed to clause 34 as drafted.
Clause 35 – Short title
70. The Committee agreed to clause 35 as drafted.
Schedule 1 – The Regional Health and Social Care Board
71. The Committee noted that schedule 1 deals with the membership of the Regional Board and also covers other provisions including committees, sub-committees, finance and accounts. The Committee agreed to schedule 1 as drafted.
Schedule 2 – The Regional Agency for Public Health and Social Well-being
72. The Committee noted that schedule 2 deals with the membership of the Regional Agency and also covers other provisions including committees, sub-committees, finance and accounts. The Department accepted that there was an error in paragraph 7(3) in that the reference to ‘the Regional Board’ should read ‘RAPHSW’. The Department also advised that there was an error in paragraph 6 relating to the resignation or removal of members of district councils who are appointed to the regional agency. The Department advised that it intends to bring forward a revised schedule 2 because of the large number of changes required as a result of the title changes. The Committee agreed to schedule 2 subject to the proposed amendments to paragraphs 6 and 7(3).
Schedule 3 – The Regional Support Services Organisation
73. The Committee noted that schedule 3 deals with the membership of the Regional Support Services Organisation and also covers other provisions including committees, sub-committees, finance and accounts. The Committee agreed to schedule 3 as drafted.
Schedule 4 – The Patient and Client Council
74. The Committee noted that schedule 4 sets out the arrangements for the operation of the Patient and Client Council and deals with its status, constitution, remuneration, staffing, procedures, finance and annual reports. The Committee agreed to schedule 4 as drafted.
Schedule 5 – Transfer of assets, etc
75. The Committee noted that schedule 5 deals with the transfer of assets and liabilities and outlines arrangements for the completion of annual reports and accounts of health and social care bodies that have been dissolved. The Department advised that it proposed to make an amendment to paragraph 2(6) to insert a reference to the ‘transferor’ organisations. The Department explained that the provisions, as currently drafted, do not exclude the ‘transferor’ organisations from the process of consideration of grievances. The Committee agreed to schedule 5 as drafted subject to the proposed amendment to paragraph 2(6).
Proposed amendment, schedule 5, paragraph 2(6)(a), “after the second ‘of’ insert ‘a transferor or’”
Schedule 6 – Minor and consequential amendments
76. The Committee noted that schedule 6 deals with amendments to other legislation as a result of the Bill. The Department indicated that it needed to make a technical amendment to the paragraph 18(1)(a) of the schedule, namely that the words ”the Regional Board or RAPSHW” will be replaced by “Regional Business Services Organisation”. The Committee agreed to schedule 6 as drafted subject to the proposed technical amendment.
Proposed amendment, schedule 6, paragraph 18(1)(a), “leave out ‘the Regional Board or RAPHSW’ and insert ‘RBSO’”
Schedule 7 – Repeals
77. The Committee agreed to schedule 7 as drafted.
Appendix 1
Minutes of Proceedings
Relating to the Report
Thursday, 6 March 2008
Room 135, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies: Rev Dr Robert Coulter MLA
Mr Alex Easton MLA
Ms Carál Ní Chuilín MLA
The meeting commenced at 2.40 p.m. in closed session.
The meeting moved to Public Session at 3.07p.m.
3. Evidence session with the Minister for Health, Social Services and Public Safety
The Minister was accompanied by:
Dr Andrew McCormick Permanent Secretary
Dr Michael McBride Chief Medical Officer
Dr Miriam McCarthy Deputy Secretary Health Care Policy
Bernard Mitchell Modernisation Directorate
David Bingham Director Human Resources
The Minister briefed the Committee on proposals for Health and Social care reform then took questions from Members. The Minister then addressed other issues raised by Members. The Chairperson thanked the Minister and officials’ for attending.
[EXTRACT]
Thursday, 22 May 2008
Boardroom, Northern Ireland
Fire & Rescue Service, Lisburn
Present: Ms Michelle O’Neill MLA, Deputy Chairperson (In the Chair)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr John McCallister MLA
In Attendance: Mr Hugh Farren (Clerk)
Ms Hilary Bogle (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies: Mrs Iris Robinson MLA (Chairperson)
Mr Thomas Buchanan MLA
Rev Robert Coulter MLA
Mrs Carmel Hanna MLA
Ms Claire McGill
Ms Sue Ramsey MLA
The meeting commenced at 2.58 p.m. in public session.
5. Evidence session with the Health Promotion Agency
Members took evidence from Dr Brian Gaffney, Chief Executive, Health Promotion Agency about the proposals to reform the health and social care system.
A question and answer session ensued. The chairperson thanked Dr Gaffney for attending.
[EXTRACT]
Thursday, 19 June 2008
Room 135, Parliament Buildings
Present: Ms Michelle O’Neill MLA, Deputy Chairperson (in the Chair)
Mr Thomas Buchanan MLA
Rev Robert Coulter MLA
Mr Alex Easton MLA
Dr Kieran Deeny MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Ms Hilary Bogle (Assistant Clerk)
Mr Mark McQuade (Assistant Clerk)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies: Mrs Iris Robinson MLA (Chairperson)
Mr Tommy Gallagher MLA
The meeting commenced at 2.37 p.m. in public session.
5. Evidence session with the Institute for Public Health on the Department’s proposals for health care reform
Members took evidence from the following witnesses:
Dr Jane Wilde Chief Executive, Institute for Public Health
Ms Claire Higgins Public Health development Officer, Institute for Public Health
2.55pm Mr Alex Easton joined the meeting.
3.06pm Ms Sue Ramsey left the meeting.
A question and answer session ensued. The chairperson thanked the witnesses for attending.
3.40pm the Committee adjourned
3.50pm the Committee reconvened
6. Evidence session with the Northern Ireland Local Government Association (NILGA) on the Department’s proposals for health care reform
Members took evidence from the following witnesses:
Ms Heather Moorhead Chief Executive, NILGA
Arnold Hatch President, NILGA
A question and answer session ensued. The chairperson thanked the witnesses for attending.
4.27pm Dr Deeny left the meeting
[EXTRACT]
Thursday, 3 July 2008
Senate Chamber, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Ms Hilary Bogle (Assistant Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Officer)
Apologies: Rev Robert Coulter MLA
Dr Kieran Deeny MLA
Mr Tommy Gallagher MLA
Ms Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
The meeting commenced at 2.39 pm in public session.
5. Evidence session with the Mental Health Commission
Members took evidence from the following witnesses:
Mr Paul McBrearty Chief Executive, Mental Health Commission
Mr Noel McKenna Chairperson, Mental Health Commission
Ms Clare Quigley Social Work Member of the Commission
Dr Brian Fleming Consultant Psychiatrist and Medical Member of the Commission
3.18pm Ms Ramsey left the meeting
3.22pm Ms Ramsey returned to the meeting
A question and answer session ensued. The chairperson thanked the witnesses for attending.
7. Health and Social Care (Reform) Bill
Members noted that the Health and Social Care (Reform) Bill received its Second Reading in the Assembly on Tuesday 1 July 2008 and that the Bill has been passed to the Committee to undertake the ‘Committee Stage’. The Committee agreed to release a press release and public notice and that relevant organisations should be invited to submit comments on the provisions of the Bill.
[EXTRACT]
Thursday, 11 September 2008
Room 135, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Alister Strain (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Apologies: Dr Kieran Deeny MLA
Mr Tommy Gallagher MLA
The meeting commenced at 2.34 pm in public session.
5. Health & Social Care (Reform) Bill.
Briefing on the provisions of the Bill
Members took evidence from the following witnesses:
Bernard Mitchell Modernisation Unit, DHSSPS
Ivan McMaster Modernisation Unit, DHSSPS
Craig Allen Modernisation Unit, DHSSPS
A question and answer session ensued. The chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 18 September 2008
Room 135, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner, MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Ms Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Apologies: Mrs Michelle O’Neill MLA (Deputy Chairperson)
The meeting commenced at 2.05 pm in public session.
5. Health & Social Care (Reform) Bill.
Evidence session with the Central Services Agency
Members took evidence from the following witnesses:
Stephen Hodkinson Chief Executive, Central Services Agency
Jacqueline Kennedy Director of Human Resources and Corporate Services
Paula Sheils Director of Family Practitioner Services
A question and answer session ensued. The chairperson thanked the witnesses for attending.
[EXTRACT]
Thursday, 25 September 2008
Seminar Rooms,
Muckamore Abbey Hospital
Present: Mrs Iris Robinson MP MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner, MLA
Mrs Carmel Hanna MLA
Ms Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
Apologies: Mr Thomas Buchanan MLA
Mr John McCallister MLA
Ms Sue Ramsey MLA
The meeting commenced at 2.01 pm in public session.
5. Health & Social Care (Reform) Bill
Evidence session with the Health & Social Services Boards
Members took evidence from the following witnesses:
Dominic Burke Acting Chief Executive, Western Health & Social Services Board
Paula Kilbane Chief Executive, Eastern Health & Social Services Board
Stuart MacDonnell Chief Executive, Northern Health & Social Services Board
Fionnuala McAndrew Director of Social Services, Southern Health & Social Services Board
Dr Kieran Deeny made a declaration of interest that he was a member of a Local Commissioning Group
A question and answer session ensued. The chairperson thanked the witnesses for attending.
A Member made a request that witnesses avoid using abbreviations when presenting evidence to the Committee.
6. Health & Social Care (Reform) Bill.
Evidence session with the Health & Social Services Councils
Members took evidence from the following witnesses:
Richard Dixon Chief Officer, Eastern Health & Social Services Council
A question and answer session ensued. The chairperson thanked the witnesses for attending.
3.08 p.m. Committee meeting adjourned.
3.16 p.m. Committee meeting resumed.
7. Health & Social Care (Reform) Bill.
Evidence session with the Regulation & Quality Improvement Authority
Members took evidence from the following witnesses:
Alice Casey Interim Chief Executive, Regulation & Quality Improvement Authority
Phelim Quinn, Director of Operations, Regulation & Quality Improvement Authority
Jude O’Neill Head of Mental Health and Learning Disability, Regulation & Quality Improvement Authority
A question and answer session ensued. The chairperson thanked the witnesses for attending.
3.22 p.m. Mr Tommy Gallagher rejoined the meeting.
[EXTRACT]
Thursday, 2 October 2008
Senate Chamber, Parliament Buildings
Present: Mrs Michelle O’Neill MLA (Deputy Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner, MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
The meeting commenced at 2.06 pm in public session with the Deputy Chairperson in the Chair.
5. Health & Social Care (Reform) Bill.
Evidence session with the Royal College of Nursing
Members took evidence from the following witnesses:
Mary Hinds Director, Royal College of Nursing Northern Ireland
Ann Marie O’Neill Chair, Royal College of Nursing Northern Ireland Board.
A question and answer session ensued. The Deputy Chairperson thanked the witnesses for attending.
6. Health & Social Care (Reform) Bill.
Evidence session with the British Medical Association
Members took evidence from the following witnesses:
Dr Brian Patterson British Medical Association (NI), Chairman of Northern Ireland Council
Dr Brian Dunn British Medical Association (NI), Chairman of the General Practitioners Committee
Mr Danny Lambe British Medical Association (NI), Deputy Secretary
Mr Ivor Whitten British Medical Association (NI), Assembly & Research Officer
A question and answer session ensued. The Deputy Chairperson thanked the witnesses for attending.
Mr Sam Gardiner made a declaration of interest that he is a Local Councillor.
Mrs Claire McGill made a declaration of interest that she is a Local Councillor.
2.50 p.m. Mr Tommy Gallagher left the meeting.
3.02 p.m. Mr Tommy Gallagher rejoined the meeting.
3.02 p.m. Mr Thomas Buchanan joined the meeting.
3.12 p.m. Mr John McCallister joined the meeting.
3.14 p.m. Ms Sue Ramsey left the meeting.
7. Health & Social Care (Reform) Bill.
Evidence session with the Allied Health Profession Federation
Members took evidence from the following witnesses:
Mrs Liz Cavan Committee Member, Allied Health Professions Federation UK
Ms Liz McKnight Chair, Allied Health Professions Federation NI.
Mr Tom Sullivan Policy Officer, Chartered Society of Physiotherapy NI.
A question and answer session ensued. The Deputy Chairperson thanked the witnesses for attending.
Dr Kieran Deeny made a declaration of interest that he is a member of a Local Commissioning Group.
3.44 p.m. Ms Sue Ramsey rejoined the meeting.
3.44 p.m. Committee meeting adjourned.
3.56 p.m. Committee meeting resumed.
8. Clause by Clause consideration of the Health & Social Care (Reform) Bill
The following witnesses attended:
Ivan McMaster Department of Health, Social Services & Public Safety
Bernard Mitchell Department of Health, Social Services & Public Safety
Craig Allen Department of Health, Social Services & Public Safety
The Deputy Chairperson referred Members to the legislation & copy of responses received from relevant bodies.
Clause 1 (Restructuring of administration of health and social care)
Clause 1 deferred. The Department is to provide further information.
Clause 2 (Department’s general duty)
Clause 2 deferred.
Clause 3 (Department’s general power)
Clause 3 deferred.
Clause 4 (Department’s priorities and objectives)
Clause 4 deferred. The Department is to consider proposed amendment.
Clause 5 (The framework document)
Clause 5 deferred. The Department is to consider proposed amendment.
Clause 6 (Power of Department to give directions to certain bodies)
Clause 6 deferred. The Department is to consider proposed amendment.
[EXTRACT]
Thursday, 9 October 2008
Senate Chamber, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner, MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
The meeting commenced at 2.04 pm in public session.
3. Clause by Clause consideration of the Health & Social Care (Reform) Bill
The following witnesses attended:
Bernard Mitchell Department of Health, Social Services & Public Safety
Ivan McMaster Department of Health, Social Services & Public Safety
Craig Allen Department of Health, Social Services & Public Safety
Michael McBride Chief Medical Officer
The committee discussed the rationale for the proposed Regional Board and the separate Regional Agency for Public Health and Social Wellbeing.
4.19 p.m. Mrs Carmel Hanna left the meeting.
4.19 p.m. Mrs Michelle O’Neill rejoined the meeting
4.20 p.m. Mrs Carmel Hanna rejoined the meeting.
4.20 p.m. Mr Tommy Gallagher rejoined the meeting.
4.27 p.m. Mrs Claire McGill rejoined the meeting.
4.42 p.m. Mr Thomas Buchanan rejoined the meeting.
4.42 p.m. Mr Sam Gardiner left the meeting.
4.45 p.m. Mr John McCallister rejoined the meeting.
4.52 Dr Michael McBride left the meeting.
4.54 p.m. Mr Tommy Gallagher left the meeting.
The Chairperson referred Members to the legislation & copy of responses received from relevant bodies. The committee commenced clause by clause consideration of the Health & Social Care (Reform) Bill at Clause 7.
Clause 7 (The Regional Health and Social Care Board)
Clause 7 deferred.
Schedule 1 (The Regional Health and Social Care Board)
Schedule 1 deferred.
Clause 8 (Functions of the Regional Board)
Clause 8 deferred, officials advised that the Minister was considering an amendment to Clause 8(3) (b).
Clause 9 (Local Commissioning Groups)
Clause 9 deferred, The Department is to consider a proposed amendment.
Dr Kieran Deeny made a declaration of interest that he is a member of a Local Commissioning Group.
Clause 10 (Power of Regional Board to give directions and guidance to HSC trusts)
Clause 10 deferred.
Clause 11 (Provision of information, etc. to Regional Board by HSC trusts)
Clause 11 deferred.
The Committee agreed to continue consideration of Bill at its next meeting. The Chairperson thanked the witnesses for attending.
5.06 p.m. Mrs Carmel Hanna left the meeting.
[EXTRACT]
Thursday, 16 October 2008
Senate Chamber, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner, MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
Apologies: Mrs Michelle O’Neill MLA (Deputy Chairperson)
The meeting commenced at 2.03 pm in public session.
7. Clause by Clause consideration of the Health & Social Care (Reform) Bill
The following witnesses attended:
Bernard Mitchel Department of Health, Social Services & Public Safety
Ivan McMaster Department of Health, Social Services & Public Safety
Craig Allen Department of Health, Social Services & Public Safety
Michael McBride Chief Medical Officer
The Chief Medical Officer provided the Committee with an update on screening for breast cancer.
The Chairperson referred Members to the legislation & copy of responses received from relevant bodies. The committee commenced clause by clause consideration of the Health & Social Care (Reform) Bill at Clause 12.
2.28 p.m. Mr Tommy Gallagher left the meeting.
2.35 p.m. Mr Tommy Gallagher rejoined the meeting.
Clause 12 (The Regional Agency for Public Health and Social Well-being)
Clause 12 deferred. The Department is to provide further information.
Schedule 2 (The Regional Agency for Public Health and Social Well-being)
Schedule 2 deferred.
Clause 13 (Functions of RAPHSW)
Clause 13 deferred. The Department is to consider proposed amendment.
3.09 p.m. Mr Tommy Gallagher left the meeting.
3.14 p.m. Dr Michael McBride left the meeting.
3.14 p.m. Mr Tommy Gallagher rejoined the meeting.
Clause 14 (The Regional Support Services Organisation)
Clause 14 deferred. The Department is to consider proposed amendment.
3.15 p.m. Mrs Iris Robinson left the meeting.
3.15 p.m. Ms Sue Ramsey took the Chair.
Schedule 3 (The Regional Support Services Organisation)
Schedule 3 deferred.
Clause 15 (Functions of RSSO)
Clause 15 deferred. The Department is to consider proposed amendment.
3.20 p.m. Mrs Iris Robinson rejoined the meeting & resumed the chair.
Clause 16 (The Patient and Client Council)
Clause 16 deferred
3.26 p.m. Ms Sue Ramsey left the meeting.
Schedule 4 (The Patient and Client Council)
Schedule 4 deferred
Clause 17 (Functions of the Patient and Client Council)
Clause 17 deferred. The Department is to consider proposed amendment.
Clause 18 (Duty to co-operate with the Patient and Client Council)
Clause 18 deferred. The Department is to consider proposed amendment.
3.32 p.m. Mrs Carmel Hanna left the meeting.
Clause 19 (Public involvement and consultation)
Clause 19 deferred
3.39 p.m. Ms Sue Ramsey rejoined the meeting.
Clause 20 (Public involvement: consultation schemes)
Clause 20 deferred
Clause 21 (Duty on HSC trusts in relation to improvement of health and social well-being)
Clause 21 deferred
Clause 22 (Public-private partnerships)
Clause 22 deferred
Clause 23 (Schemes for transfer of assets and liabilities)
Clause 23 deferred
Clause 24 (Transfer of functions of Health and Social Services Boards)
Clause 24 deferred
Clause 25 (Transfer of functions of the Mental Health Commission)
Clause 25 deferred
Clause 26 (Transfer of functions of Central Services Agency)
Clause 26 deferred
Clause 27 (Amendment of statutory and other references to dissolved bodies, etc)
Clause 27 deferred
Clause 28 (Dissolution of special agencies)
Clause 28 deferred
Clause 29 (Orders, regulations, guidance and directions)
Clause 29 deferred. The Department is to consider proposed amendment.
Clause 30 (Further provision)
Clause 30 deferred
Clause 31 (Interpretation)
Clause 31 deferred
Clause 32 (Minor and consequential amendments)
Clause 32 deferred
Clause 33 (Repeals)
Clause 33 deferred
Clause 34 (Commencement)
Clause 34 deferred
Clause 35 (Short title)
Clause 35 deferred
Schedule 5 (Transfer of assets, etc)
Schedule 5 deferred
Schedule 6 (Minor and consequential amendments)
Schedule 6 deferred
Schedule 7 (Repeals)
Schedule 7 deferred
The Committee agreed to continue formal consideration of Bill at its next meeting. The Chairperson thanked the witnesses for attending.
Members agreed a motion to extend the Committee Stage of the Bill to 5 December 2007.
[EXTRACT]
Thursday, 23 October 2008
Senate Chamber, Parliament Buildings
Present: Ms Sue Ramsey MLA (In the chair)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner, MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
Apologies: Mrs Iris Robinson MP MLA (Chairperson)
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Dr Kieran Deeny MLA
The meeting commenced at 2.06 pm in public session.
8. Clause By Clause consideration of the Health & Social Care (Reform) Bill
The following witnesses attended:
Bernard Mitchel Department of Health, Social Services & Public Safety
Ivan McMaster Department of Health, Social Services & Public Safety
Craig Allen Department of Health, Social Services & Public Safety
Carolyn Harper Department of Health, Social Services & Public Safety
The Committee agreed to consider clauses where there was no dispute and defer consideration of other clauses to the next Committee meeting
The Chairperson referred Members to the legislation & copy of responses received from relevant bodies. The committee commenced clause by clause consideration of the Health & Social Care (Reform) Bill at Clause 1.
Clause 1 (Restructuring of administration of health and social care)
Clause 1 deferred for further consideration.
Clause 2 (Department’s general duty)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 3 (Department’s general power)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 4 (Department’s priorities and objectives)
Clause 4 deferred for further consideration.
Clause 5 (The framework document)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment by the Department, put and agreed to.
Clause 6 (Power of Department to give directions to certain bodies)
Clause 6 deferred for further consideration.
Clause 7 (The Regional Health and Social Care Board)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 8 (Functions of the Regional Board)
Clause 8 deferred for further consideration
Clause 9 (Local Commissioning Groups)
Clause 9 deferred for further consideration.
Clause 10 (Power of Regional Board to give directions and guidance to HSC trusts)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 11 (Provision of information, etc. to Regional Board by HSC trusts)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 12 (The Regional Agency for Public Health and Social Well-being)
Clause 12 deferred for further consideration.
Schedule 2 (The Regional Agency for Public Health and Social Well-being)
Schedule 2 deferred for further consideration.
Clause 13 (Functions of RAPHSW)
Clause 13 deferred for further consideration
Clause 14 (The Regional Support Services Organisation)
Question: That the Committee is content with the clause as drafted subject to the change in the title of the body, put and agreed to.
Schedule 3 (The Regional Support Services Organisation)
Question: That the Committee is content with schedule 3 as drafted, put and agreed to.
Clause 15 (Functions of RSSO)
Clause 15 deferred for further consideration.
Clause 16 (The Patient and Client Council)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Schedule 4 (The Patient and Client Council)
Question: That the Committee is content with schedule 4 as drafted, put and agreed to.
Clause 17 (Functions of the Patient and Client Council)
Clause 17 deferred for further consideration.
Clause 18 (Duty to co-operate with the Patient and Client Council)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment by the Department, put and agreed to.
Clause 19 (Public involvement and consultation)
Clause 19 deferred for further consideration.
Clause 20 (Public involvement: consultation schemes)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment by the Department, put and agreed to.
Clause 21 (Duty on HSC trusts in relation to improvement of health and social well-being)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment by the Department, put and agreed to.
Clause 22 (Public-private partnerships)
Clause 22 deferred for further consideration.
Clause 23 (Schemes for transfer of assets and liabilities)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Schedule 5 (Transfer of assets, etc)
Schedule 5 deferred for further consideration.
Clause 24 (Transfer of functions of Health and Social Services Boards)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 25 (Transfer of functions of the Mental Health Commission)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 26 (Transfer of functions of Central Services Agency)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 27 (Amendment of statutory and other references to dissolved bodies, etc)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 28 (Dissolution of special agencies)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 29 (Orders, regulations, guidance and directions)
Clause 29 deferred for further consideration.
Clause 30 (Further provision)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 31 (Interpretation)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 32 (Minor and consequential amendments)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Schedule 6 (Minor and consequential amendments)
Schedule 6 deferred for further consideration.
Clause 33 (Repeals)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Schedule 7 (Repeals)
Question: That the Committee is content with schedule 7 as drafted, put and agreed to.
Clause 34 (Commencement)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 35 (Short title)
Question: That the Committee is content with the clause as drafted, put and agreed to.
[EXTRACT]
Thursday, 6 November 2008
Senate Chamber, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Dr Kieran Deeny MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
Apologies: Mr Thomas Buchanan MLA
Mr Sam Gardiner MLA
Mrs Claire McGill MLA
The meeting commenced at 2.04 pm in public session.
7. Clause By Clause consideration of the Health & Social Care (Reform) Bill
The following witnesses attended:
Bernard Mitchell Department of Health, Social Services & Public Safety
Ivan McMaster Department of Health, Social Services & Public Safety
Craig Allen Department of Health, Social Services & Public Safety
Martin Bradley Chief Nursing Officer
Clause 1 (Restructuring of administration of health and social care)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment agreed by the Department, put and agreed to.
Clause 4 (Department’s priorities and objectives)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment agreed by the Department, put and agreed to.
Clause 6 (Power of Department to give directions to certain bodies)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment agreed by the Department, put and agreed to.
Clause 8 (Functions of the Regional Board)
Question: That the Committee is content with the clause as drafted and supports the proposal to amend section (3) requiring the Regional Board and Regional Agency to jointly sign-off the commissioning plan, put and agreed to.
Clause 9 (Local Commissioning Groups)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment agreed by the Department, put and agreed to.
Clause 12 (The Regional Agency for Public Health and Social Well-being)
Question: that the regional public health agency be incorporated into the proposed regional board under clause 7.
Proposer: Mr Alex Easton
Seconder: Mrs Iris Robinson
The Committee divided: Ayes 2; Noes 6; Abstentions 0
AYES
Mr Alex Easton
Mrs Iris Robinson
NOES
Dr Kieran Deeny
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Mrs Michelle O’Neill
Ms Sue Ramsey
ABSTENTIONS
None
The motion falls
As consensus could not be reached on clause 12 as drafted the Chairperson proposed:
That the Committee is content with Clause 12 as drafted Question put.
The Committee divided: Ayes 6; Noes 2; Abstentions 0
AYES
Dr Kieran Deeny
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Mrs Michelle O’Neill
Ms Sue Ramsey
NOES
Mr Alex Easton
Mrs Iris Robinson
ABSTENTIONS
None
Question accordingly agreed to.
Clause 13 (Functions of RAPHSW)
Question: That the Committee is content with the clause as drafted subject to the proposed amendment agreed by the Department, put and agreed to.
Clause 15 (Functions of RSSO)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 17 (Functions of the Patient and Client Council)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 19 (Public involvement and consultation)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 22 (Public-private partnerships)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Clause 29 (Orders, regulations, guidance and directions)
Question: That the Committee is content with the clause as drafted, put and agreed to.
Schedule 1 (The Regional Health and Social Care Board)
Question: That the Committee is content with schedule 1 as drafted, put and agreed to.
Schedule 2 (The Regional Agency for Public Health and Social Well-being)
Question: That the Committee is content with schedule 2 as drafted subject to the proposed amendments to paragraph 6 and 7(3), put and agreed to.
Schedule 5 (Transfer of assets, etc)
Question: That the Committee is content with schedule 5 as drafted subject to the proposed amendment to paragraph 2(6), put and agreed to.
Schedule 6 (Minor and consequential amendments)
Question: That the Committee is content with schedule 6 as drafted subject to the proposed amendment to paragraph 18(1)(a), put and agreed to.
4.17 p.m. Mr John McCallister left the meeting.
4.21 p.m. Ms Sue Ramsey left the meeting.
4.29 p.m. Ms Sue Ramsey rejoined the meeting.
4.33 p.m. Mr John McCallister left the meeting.
4.36 p.m. Mr Tommy Gallagher left the meeting.
[EXTRACT]
Thursday, 13 November 2008
Room 135, Parliament Buildings
Present: Mrs Iris Robinson MP MLA (Chairperson)
Mr Thomas Buchanan MLA
Mr Alex Easton MLA
Mr Tommy Gallagher MLA
Mr Sam Gardiner MLA
Mrs Carmel Hanna MLA
Mr John McCallister MLA
Mrs Claire McGill MLA
Ms Sue Ramsey MLA
In Attendance: Mr Hugh Farren (Clerk)
Mr Mark McQuade (Assistant Clerk)
Mrs Noelle Bourke (Clerical Supervisor)
Mr Joe Westland (Clerical Supervisor)
Mr Rodney Aiken (Clerical Officer)
Apologies: Dr Kieran Deeny MLA
Mrs Michelle O’Neill MLA (Deputy Chairperson)
The meeting commenced at 2.06 pm in public session.
6. Consideration of the draft Report on the Committee Stage of the Health and Social Care (Reform) Bill.
The Committee considered the Draft Report on the Committee Stage of the
Health and Social Care (Reform) Bill paragraph by paragraph. The Committee agreed the main body of the report:
Paragraph 1-11, read and agreed
Paragraph 12-13, read and agreed
Paragraph 14-15, read and agreed
Paragraph 16-18, read and agreed
Paragraph 19-22, read and agreed
Paragraph 23-27, read and agreed
Paragraph 28-34, read and agreed
Paragraph 35, read and agreed as amended
Paragraph 36-38, read and agreed
Paragraph 39, read and agreed as amended
Paragraph 40-41, read and agreed
paragraph 42-45, read and agreed
Paragraph 46-49, read and agreed
Paragraph 50-55, read and agreed
Paragraph 56-57, read and agreed
Paragraph 58-70, read and agreed
Paragraph 71-77, read and agreed
The Committee agreed the Executive Summary
Paragraph 1-6, read and agreed
The Committee agreed that Appendix 1 to 5 be included in the report.
The Committee agreed that an extract of today’s Minutes of Proceedings should be included in Appendix 1 of the report and were content that the Chairperson agrees the minutes relating to this to allow them to be included in the printed report.
The Committee ordered the Report on the Health and Social Care (Reform) Bill (NIA 21/07) to be printed.
[EXTRACT]
Appendix 2
Minutes of Evidence
Table of Contents
Ministerial Briefing 6th March 2008 51
Health Promotion Agency 22nd May 2008 61
Institute for Public Health 19th June 2008 67
NILGA 19th June 2008 75
Mental Health Commission 3rd July 2008 81
Departmental Briefing on the provisions
of the Health & Social Care (Reform) Bill 11th September 2008 87
Representatives of Central Services Agency 18th September 2008 95
Representatives of Eastern Health & Social Services Council 25th September 2008 103
Representatives of the Health & Social Services Board 25th September 2008 107
Representatives of the RQIA 25th September 2008 115
Representatives of Allied Health Professions 2nd October 2008 123
Representatives of the BMA 2nd October 2008 129
Clause by clause consideration of
the Health & Social Care (Reform) Bill 2nd October 2008 137
Representatives of the Royal College of Nursing 2nd October 2008 147
Clause by clause consideration of
the Health & Social Care (Reform) Bill. 9th October 2008 151
Clause by clause consideration of
the Health & Social Care (Reform) Bill 16th October 2008 161
Clause by clause consideration of
the Health & Social Care (Reform) Bill. 23rd October 2008 177
Clause by clause consideration of
the Health & Social Care (Reform) Bill. 6th November 2008 183
6 March 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Sue Ramsey
Witnesses:
|
Dr Michael McBride |
||
|
Mr Michael McGimpsey |
Minister of Health, Social Services and Public Safety |
1. The Chairperson of the Committee for Health, Social Services and Public Safety (Mrs I Robinson): I apologise for the delay in inviting the public and the Minister into the Committee; we had some housekeeping matters to attend to. I welcome the Minister and his officials and those in the Public Gallery.
2. Minister, I regret that your time has been cut short. When the Deputy Chairperson and I met you some time ago, you said that you would be happy to discuss any issues that we might raise. However, we will not have time to discuss those matters today. The main evidence session will be on the proposals for health and social care reform, which you announced on 4 February 2008 and which are now subject to consultation.
3. I welcome Dr Andrew McCormick, the Department’s permanent secretary; Dr Michael McBride, the Chief Medical Officer; Dr Miriam McCarthy, deputy secretary from healthcare policy; Bernard Mitchell from the modernisation directorate; and David Bingham, the director of human resources.
4. As our time is limited, I will hand over immediately to the Minister.
5. The Minister of Health, Social Services and Public Safety (Mr McGimpsey): Thank you for the welcome; I am delighted to be here. I will get through my opening remarks as quickly as possible, as I know that you are anxious to ask questions and I am keen to answer them.
6. First, restructuring is guided by the need to modernise the health estate — several hospitals are more than 50 years old and will need to be replaced at considerable capital cost. Secondly, we need to be efficient; I recognise that the Health Service is inefficient, and we must drive out inefficiencies. Thirdly, we must engage the local population in taking responsibility for its own health. Those are the three overarching strategic aims to which I work.
7. When I came into office I was faced with a proposal for a health and social care authority, and when I examined the proposals I felt that some opportunities had been missed. I went back to square one and began with a blank sheet of paper. I worked on proposals that presented the best opportunity for administering health for the future and began by looking at the three core functions that were proposed for the health and social care authority.
8. The first was to determine need in various areas and to commission health provision to address it.
9. Secondly, we considered performance management and improvement. Much of that is included under targets and ensuring that we deliver as efficiently as possible without affecting quality and patient safety.
10. The third aspect is finance. We deal with a very large budget and some very large organisations, and those organisations must stay within budget and exercise financial discipline.
11. Those were the three core elements that I looked for in a new regional health and social care board to replace the four existing health boards. It will have a maximum of 400 staff and will focus on commissioning performance management, improvement and financial management.
12. The next step involved engaging the population. Direct rule Ministers proposed to abolish the Health Promotion Agency, and its functions would be subsumed in that giant authority. I thought that that was a missed opportunity. Having taken advice from Dr Michael McBride, the Chief Medical Officer, and a very wide range of opinion from Northern Ireland and further afield, it was decided that the agency was the best way forward. A health promotion and improvement organisation was proposed — which would include the Health Promotion Agency — but which would have several other functions, including health promotion, health protection and public health.
13. We will engage the population, particularly on health inequalities: men living in inner south Belfast will live five years less than those who live in outer south Belfast; women will live three years less. That is as a result of health inequalities. We must look at how we drive forward health promotion, health protection and the public-health agenda.
14. Furthermore, I talked about the need for democratisation. Local government has a major role in public-health and in working closely with the new public health agency. There are some problems with local government as we do not know how many councils there will be, but we are fastened to the present five trusts, and we can be largely coterminous with whatever emerges, with some small adjustments. There is a focus on local government working on local community planning with local community and volunteer groups; initiatives such as health action zones and healthy cities will also be important. Responsibility for those functions will be removed from the trusts and given to the new agency, which will work closely with local government.
15. As part of the democratisation agenda, I have examined the commissioning function of the regional health and social care board and have decided that local public representatives should sit on the commissioning groups. I also expect to see local government representation on the board of the new agency as well.
16. I have also considered the proposal for a patient client council. As the Committee is aware, there are four health and social service councils, whereas the proposal under direct rule was to abolish them and to replace them with a single patient client council. However, we do not want to miss an opportunity to allow local representatives to play an important role in representing their communities. Those councils should not be abolished but should be reinforced and strengthened. We are considering proposals for a regional council with five sub-councils or perhaps one for each trust. That is covered in the consultation document. It is important that the local population has a voice.
17. A common services organisation will take over functions such as financial payments, recruitment, estates management, and information and communication technology that are not core to the board, the agency or the Department. That will reduce the size of the Department. The Department will focus on policy, legislation, standards and priorities, and on supporting and advising the Minister. The original proposal was for human resources to be dealt with by the new authority. However, as I do not believe that to be a sensible move, I will retain human resources in the Department.
18. That is a brief synopsis of the Department’s direction. The time frame is very tight, but it is achievable, and the 12-week consultation period is already under way. My target is to have the legislation ready for Second Stage by the summer.
19. The efficiencies that were set out under the review of public administration — a reduction of 1,700 administrative jobs to save £53 million per annum — will be achieved under that arrangement, and we will hit all the targets that we said we would. However, the major efficiencies will be achieved through the working of the new structures. As colleagues are aware, the five trusts were in place when I took up office in May, and I felt that it would be a mistake to alter those structures fundamentally or to tamper with them. At that stage, the new structures were just starting out and needed to be built up rather than put into reverse. Thus those structures will largely stay the same. As I said, it is my intention that responsibility for public health will be taken from the trusts and given to a new regional health promotion agency.
20. I am happy to leave it there and answer colleagues’ questions.
21. The Chairperson: When will the regional health and social care board come into being?
22. Mr McGimpsey: I anticipate that it will come into being in April 2009. The target date is 1 April in the next financial year, which is tight but achievable. There is sufficient time for a full consultation period and the consideration of its findings. As in the run-up to the Budget, I will visit boards and trusts throughout Northern Ireland because the establishment of the new board poses many questions.
23. Through the consultation process, I will be keen to hear what others have to say and to consider any additional feedback. I am at pains to emphasise that nothing is written in stone. I have created a broad outline, but I am keen to hear from everyone, including the unions and staff. A great deal of wisdom is gained simply by listening.
24. The Chairperson: I have a question for the Minister, although it may not be particularly relevant to today’s meeting. Given that the Department of Health, Social Services and Public Safety has been treated differently from all the other Departments, have you calculated what further savings can be made over and above the 3% efficiencies that can be returned to the Department over for use in front-line services? Have you come up with any figures?
25. Mr McGimpsey: The review of public administration states that 1,700 jobs must be cut to save £53 million, and that will be achieved.
26. Mr McCallister: Minister, I want to tease out more of your thoughts on local councils. How will local councils help in promoting health?
27. My second question is probably more for the Chief Medical Officer: will the agency do as much to promote and improve health as it will do for those who already suffer from long-term conditions?
28. Michael, you and I attended a stroke strategy event yesterday. Is that the type of condition that the agency can help to prevent? Is the agency as concerned with preventing the further deterioration of poor health as it is with health promotion?
29. Mr McGimpsey: Many Committee members have been local government representatives. My experience, as a member of Belfast City Council for the past 15 years, is that Departments are good at devising policies and plans. However, I am not so sure about their ability to deliver and implement those policies, and I envisage that local government will play a crucial role in that. Local government would be good at implementation. There is an opportunity for local representatives, who work closely with communities, to provide local representation and implementation.
30. Local government will have a strong role to play in delivering initiatives such as health action zones and healthy cities, and particularly in Investing for Health and the tackling of health inequality. As I do not yet know how many councils there will be, it is difficult to determine to what extent local government will be represented on commissioning groups, the public health agency, and patient and client councils.
31. However, I will reserve places for local government representatives, and there must be a drive for representation across the board. How that is done is a matter for discussion with the Northern Ireland Local Government Association (NILGA), local councils and others. Peter Hain proposed seven councils, the present number is 26, and the assumption is that the final number will be neither of those but somewhere in the middle.
32. I do not know where that middle will be. We may have our own views on the proposals, but whatever the council structure may be we will accommodate it coterminously.
33. Mr McCallister: You are determined, Minister, to move forward —
34. The Chairperson: The member will address his remarks through the Chair.
35. Mr McCallister: Minister, through the Chair, are you determined to move forward and let the Department of the Environment — and whatever is finally decided in relation to councils — catch up with you?
36. Mr McGimpsey: I am on the ministerial subgroup on the review of public administration. As for the Department of the Environment, the planning proposals are at an advanced stage, although discussions still need to be held on other areas. The new local-government structures offer us a brilliant opportunity, since decisions on the promotion of health will no longer be just a matter of the Assembly exercising its powers regionally. We have a tremendous opportunity, through local government, to redress the difficulties of the past 30 wasted years in which local councils had no powers. Councils will have an important role in the new regional health promotion agency. I will let Michael talk about health protection and public health and the input that we hope to get from local government.
37. Dr Michael McBride (Department of Health, Social Services and Public Safety): There has been much discussion about public health, and it is important that we remind ourselves that public health is about what society does to improve and protect its health and that everyone has a part to play. As the Minister said, improving public health must happen at a variety of levels. There is a strategic level across Government, under the framework that is outlined in Investing for Health and through the ministerial group on public health, which is chaired by the Minister. There is also the local level, because public health is about delivery in communities.
38. The proposals, particularly those for strong involvement from local government, provide a unique opportunity to ensure that we build on the projects that have been working well, such as the local Investing for Health partnerships. District councils have already been actively involved in that and in bringing about meaningful change for communities. Through the consultation exercise on the Minister’s proposals, we now have a unique opportunity to further embed local government in tackling health inequalities and in improving the health and well-being of the population.
39. Ultimately, public health is a matter of where people work, learn and live. It is about urban planning, such as local government decisions on the licensing of premises or about fast-food outlets; it is also about how we plan our environment, such as planning cycle paths and pedestrian precincts. Therefore local government has a vital, vibrant role to play. Public health must be put into the hearts of communities and local government, and we must build on the successes that we have undoubtedly had under the Investing for Health strategy.
40. The Chairperson: Thank you, Michael. I hope that that answers your questions, John.
41. Mr McCallister: Yes. Thank you, Chairperson.
42. Dr Deeny: Minister, you and your officials are more than welcome. Wearing my GP hat, I have a particular interest in local commissioning. That is a new concept, and I could not agree more with the idea of local and bottom-up involvement.
43. I have some questions on practicalities. This morning, I spoke to a couple of GPs who are on present local commissioning groups, and they are concerned about practical issues. For example, some GPs have made arrangements in their practices for taking on locums. I know of one practice that has taken on a partner on what it understood to be a four-year contract. What will happen in such circumstances?
44. Having spoken about the proposals in my area and with other GPs, I know that people would welcome council representation on local commissioning groups, as GPs are particularly concerned about commissioning. Some years ago, in what might be described as a water-testing exercise on fundholding, GPs almost got their hands on commissioning and the ability to use finance for services for their patients. Will there be devolved commissioning with the necessary finance and the power to make decisions?
45. If that was the case, my GP colleagues and I would more than welcome that proposal. You said that the Department is involved in legislation; we believe that it is involved in strategies and planning, but not commissioning. If the proposal is genuinely about the devolution of commissioning — with the necessary finance and decision making and a bottom-up approach involving GPs, health professionals, the public and council representatives — we would be very interested.
46. If the proposal ends up as an exercise that needs a rubber stamp from the Department, my worry is that the GPs involved might walk away from it. The Health Committee does not want that to happen, because there is a great deal of GP interest in it.
47. Can you give me an assurance that that will be the case? I know that the local commissioning groups will be part of the regional health and social care board. GPs must be made aware that they will have real commissioning power that will be backed up by financial measures. With the help of councillors, patient representatives and allied health professionals, GPs having the power to determine the needs of primary care will be good news for the future of local commissioning groups.
48. Mr McGimpsey: I can give you that assurance, Kieran. We began with a blank sheet on this proposal. I sat down with officials — Dr Andrew McCormick, David Sissling and others — and one of the first issues to arise was the agreement that David Sissling came to with the British Medical Association (BMA). The Department will stand over that, as it is very much a part of the proposal.
49. A public health medical professional, along with GPs, will be part of a commissioning group and will help to determine need. There were four GPs in each group, and that number should stay the same. You can take comfort from that, as the BMA has done. If you wish, Andrew can go through the technical details and what has already been discussed with the BMA.
50. The proposal for seven groups was made because Peter Hain said that there would be seven councils; there will not be seven, although I do not know how many there will be. It seems to work with five groups; as 15 multiplied by seven would result in 105 commissioners for Northern Ireland. I wanted to change that. I also wanted to give the groups extra weight by reducing the number to five.
51. In addition, it seems that there was a missed opportunity for local representation in the make-up of the groups. I propose that there should be four locally elected representatives in each of those groups as well a public health medical professional and other professionals. That will be subject to consultation, and other proposals will be made.
52. There will be a transition, and the Health Department will seek to manage those GPs who have given undertakings or made commitments. Andrew will deal with that crucial issue because one of the building blocks is GPs being involved in commissioning for their areas.
53. Dr Andrew McCormick (Department of Health, Social Services and Public Safety): The proposal always included a framework within which the questioning process would work. There will be a continuation of regional targets, standards and service frameworks as the basis for commissioning. However, decision making — which is the critical point — will be increasingly devolved. That will allow for consideration of targets and standards at regional level.
54. In that context, it is for the commissioning groups to make plans for the services that are appropriate to the needs of their populations, and that will enable the devolved process to work.
55. We get the best of both worlds: decision making is devolved while infrastructure and bureaucracy is kept to a minimum. The handling of money, for example, will not be the responsibility of the local commissioning groups; that minimises the need for administration and bureaucracy, but it delivers exactly what is decided at local level.
56. The Minister remains in control and his approval for commissioning plans will be required; but any plan that is based on a local assessment of need and in response to that need will be considered. That is the best of both worlds.
57. Dr Deeny: What happens to a GP has who has made changes to his or her practice and is not reselected to serve on a local commissioning group?
58. Dr McCormick: That issue will not arise until July at the earliest, so we have some time to work through the detail. During direct rule we decided not to set local commissioning groups up in shadow form, as we did not want to ask GPs to commit for a year when we were unsure what would happen. Therefore the decision was made that appointments would last for four years, which meant that some GPs made the kind of decision that you talked about. We now have to manage the consequences of that.
59. The seven groups remain, and their contribution continues to be beneficial. The consultation on the proposals is ongoing, and we will proceed only after a primary decision has been taken by the Assembly. However, the transition will have to be handled sensitively. We are grateful for the adjustments that some GPs made, and we will respect and honour those.
60. Mr Gallagher: I welcome the Minister and his team and thank them for the presentation. Most people will welcome the steps that are being taken to improve structures. It is important that what is mapped out runs concurrently with the setting up of the new councils, which is supposed to happen by 2011.
61. Does the Minister agree that, with each passing day, it becomes more likely that we will have 26 councils until 2013? If that is the case, does the Minister agree that there is a danger that the process will be messy, confusing and frustrating for those who use the service?
62. We all want inequalities to be removed. Practically every stroke sufferer who spoke at the event that John McCallister referred to said that treatment is often a postcode lottery. For example, the availability of occupational-therapy services in the west is much poorer than in the east of the Province. Is there anything in the structures that will tackle such problems?
63. Living within budgets was talked about. The Western Trust has to deal with debts of £3·3 million. I am not questioning how that debt was accrued, but it is difficult to understand how inequalities of service can be tackled while some trusts have to deal with significant debts as well as other problems.
64. Mr McGimpsey: It is coming to the end of the financial year, and trusts are expected to live within their budgets. At this time of year things become concentrated. I am not aware of there being a deficit in any of the trusts, and I would expect them to inform us if there were. Last year’s deficit has been recovered, and I expect all trusts to meet their targets this year.
65. As far as the 26 councils are concerned, I remain optimistic that we can get agreement. If we do not get agreement, things will be very messy. The Department of Health will accommodate whatever number of councils there are, whether that be 15 or some other number. Although we may be stuck with the existing structure for another while, I will deal with that and with the discussions with local government officials. However, I will not allow that to derail the key issues for the future structure of the Health Service.
66. We expect much of the inequality of provision to be addressed through commissioning based on local need. Another key element is the capitation formula for financial resources in each area. That should be done equitably and fairly, and it should be based not simply on population but on need.
67. Mr Gallagher: Will the Department still carry out the capitation exercise?
68. Mr McGimpsey: Yes, it will. The budget will flow from the Assembly to the Department. You mentioned the introduction of the service frameworks, which will set the level and quality of service that patients anywhere in Northern Ireland are entitled to expect. Some of those frameworks have been introduced and more will follow. The issue of stroke services will be addressed through one of those service frameworks.
69. Dr McBride: It is a well-known fact that, every year, 4,000 people in Northern Ireland suffer a stroke. Unfortunately and tragically, 1,300 of those people will die in the first month, and a further 1,300 will be left permanently disabled. Indeed, some of us heard the views of those affected by strokes and their carers at a very compelling workshop, which was sponsored by the Northern Ireland Chest, Heart and Stroke Association and by Speech Matters.
70. With regard to the point about the inequity in service provision, we are consulting on the draft stroke strategy. Thanks to the agreed budget settlement, there is significant investment to ensure that we improve the inequity in service provision. The consultation period finishes at the end of March.
71. We are, as the Minister indicated, developing a raft of service frameworks. There will be a section on stroke in the cardiovascular health-and-well-being service framework. That will set the optimal standards that we should attain for all patients, irrespective of whether they live in Strabane, Strangford, Ballymena or Ballycastle. The standard of service provision should be the same everywhere. Therefore, the service frameworks will set explicit standards and outcomes that we would like to achieve. As Dr McCormick said, those frameworks will then form the basis of our commissioning of services from providers, and they will inform how we will benchmark ourselves against achieving that quality of service.
72. Dr Miriam McCarthy (Department of Health, Social Services and Public Safety): We are in the process of consulting on the stroke strategy, and we invite comments from Committee members. We asked Speech Matters to produce a user-friendly, shortened document, which has been very useful in workshops for people who do not want to sit and read a lengthy textual document and for people who have suffered a stroke and for whom sight is a problem. There is a real opportunity with this strategy to make a difference.
73. I know that the Committee is interested to hear more about it at a future date, and I will facilitate that.
74. Ms S Ramsey: It is crucial that this be tied in with Investing for Health because, at that time, that document was a vision for the future. If the Assembly implements this strategy correctly, there are exciting times ahead. I do not want to seem too negative; however, having gone through the Committee’s work and having dealt with issues in my constituency, it is clear that staff, service-users and families must be informed as quickly as possible. It is important to avoid confusion during the transitional period.
75. The Minister indicated in his statement on 4 February that he had examined other models. It would be interesting to know if he has incorporated any areas of best practice into his own proposals. I am eager to ensure that no potential conflict of interest arises on commissioning groups between the provider and the commissioner.
76. I take on board the Minister’s point about local government and increasing the input of local councillors; however, considering that those councillors know the issues in their own constituencies, will the community and voluntary sector’s contribution to health and social care be negatively affected by the reform?
77. Mr McGimpsey: The community and voluntary sector plays a key role, which will be enhanced by the establishment of a regional public health agency. In my experience — and probably in the experience of anyone has who been a local councillor — local government plays an important part, through local knowledge, in delivering information and service on the ground. Furthermore, local councillors will play a key role, because they are in close contact with their communities. That is a strong reason for local government to work together with the community and voluntary sectors. Rather than compete, each should complement the other and strengthen the system.
78. The Department examined other models. For example, the Irish Republic has the Health Service Executive, which is essentially a super health-and-social-care authority, similar to what was proposed here under direct rule. However, there are mixed views about how successful that has been. The Scottish model provides that the trusts commission for their areas, depending on what they determine the needs to be. That is dangerous because the providers could commission simply what they can provide, rather than deliver provision based on need. Therefore, I believe that a separation is necessary. The Department has effectively stripped away the outer layers of the proposed health-and-social-care model to the three core functions of commissioning, performance management and financial management, and there are very strong reasons for those. That is the best way forward.
79. This is potentially a very exciting time for health, and the first time that this has happened in 30 years. If the Assembly establishes the new health and social care body correctly, it can tick a box, and — as long as the model is flexible enough to evolve and change without having to break up and start again — that body can serve its purpose for the next 30 years.
80. Dr McBride: At the time of the launch of Investing for Health. in 2002, Sir Donald Acheson, former Chief Medical Officer of England, referred to it as the best public-health document that he had seen in the English language.
81. That was a product of genuine cross-Government and cross-party co-operation under the leadership of the Minister in the Ministerial Group for Public Health. It has delivered in the short term by improving life expectancy. However, we have not been as successful in closing the inequality gap between rich and poor.
82. As you outlined, crucial factors are coming together: we have, again, a strong, local Government, and a policy review of Investing for Health will commence next year, for which we are doing the preparatory work. We are happy to keep the Committee updated on that. Furthermore, we are reviewing the fundamental structures of the Health Service to improve the health of the population, improve life expectancy and reduce health inequality. Therefore, I agree — this is an exciting time.
83. Ms S Ramsey: I do not want to sound negative, but can there be a conflict of interest between the provider and the commissioner?
84. Dr McCormick: No. We are trying to get the right balance. The commissioning groups are designed so that there is no provider involvement; there is, therefore, no conflict of interest. Furthermore, we do not regard commissioning as a confrontational process or something that is designed to cause dispute or difficulty. On the contrary, the power — the financial resources and the decision-making power — is on that side of the system. However, we must build on the successful collaborative approach that works well in this region, because trusts and commissioners can — and should — work together, particularly clinicians and other professionals. The structure and systems can deal with the hard edge of final decision-making, but the nature of the system is more collaborative and constructive, and we must build on that strength.
85. Mr McGimpsey: It is also important to stress that, although there are five commissioning groups tied to five trusts, that does not mean that each commissioning group is tied to one trust for provision — they can go to any trust. The commissioning groups have the freedom to go to any one of the five, which strengthens the commissioning function.
86. Mrs Hanna: I welcome the Minister and his colleagues. I am grateful for the presentation.
87. Although there is a fair bit of detail on the issue, I will concentrate on the headlines. You talked about the local focus; however, you spoke about the health inequalities in the individual patient’s journey. The other inequality is in long-term illness, which you referred to when you mentioned strokes. We have all been to presentations with patients and carers, and it is humbling to listen to what goes on in their heads and to how little their voice is heard. We focus on cancer and heart disease; however, many people, such as those with arthritis and multiple sclerosis who do not have those diseases still suffer quality-of-life problems. It is important to improve the details and quality of their care, even if that is only flexibility in appointments or not having to wait for six months to go to a pain clinic following a flare-up. I put it on record that it is important to do that. Many people, particularly the long-term sick, do not feel that they have a voice in a big organisation, because they are spoken to but not listened to.
88. You mentioned health promotion and the Health Promotion Agency, which is covered by the commissioning functions. Do you have any details about that? Will the Health Promotion Agency per se be incorporated into a new regional public health authority? How do you picture the strategies for disease prevention and health promotion?
89. Mr McGimpsey: Miriam will respond to your remarks about long-term illnesses and the patient journey.
90. I see the new agency as reinforcing, strengthening and enlarging the whole health-promotion agenda about promotion, protection and public health. Michael McBride can deal with the detail better than I can.
91. Dr McCarthy: You raise a very important issue on chronic-disease management.
92. Management of chronic disease is crucial to the future of services. There has been a move away from isolated incidents of disease. Most people, as they get older, are now more likely to have a chronic disease, and live with it rather than die from it. During the CSR period, the Department has identified a significant amount of money — over £10 million — to improve the management of chronic disease. Some of that is based on trying to keep people in their own homes, and maintaining their independence and dignity, rather than their being hospitalised. You are absolutely right: often, it is humbling to listen to people’s stories about how they must manage, and how their chronic disease affects not only them as individuals, but their entire families.
93. Therefore, it is important to maintain patients in their own homes, with independence and dignity. An example of how that is achieved is through the introduction of specialist nurses — heart-failure nurses and specialist respiratory nurses — who visit people in their homes. Patients love that and it makes a difference. It helps patients on a personal level and significantly improves the management of their disease. That has real potential, which must be further explored in the next couple of years.
94. Moreover, there is the potential to monitor patients at home. Rather than bring them to outpatient clinics or to GPs, they can monitored without having to leave their homes. For years, diabetics have monitored their own blood-sugar levels at home. There is huge scope to expand that area through telemedicine and other technological advances. The Department is committed to exploring those possibilities and now has funding to do so. It will look to working with professionals in achieving its objectives.
95. Dr McBride: The first part of the question referred to functions of the public-health agency. Clearly, there are three large elements of that. The first is public-health support and expert advice from the multidisciplinary public-health team to the board that will commission services, so that commissioning will be about transformational changes and services that achieve better, more equitable outcomes for all patients and service users, irrespective of where they live.
96. The second important element is that of health improvement and of bringing together the critical mass of staff and expertise from the existing boards, the Health Promotion Agency, and the health-action zones, to move forward that work agenda in a way that has always been envisaged in the investment strategy’s objectives and goals for health.
97. The important third element is health protection, which covers, as the Minister mentioned, childhood immunisation, cervical screening, breast screening, emergency planning and preparation for pandemic flu, as well as the important issue of surveillance for infections, including healthcare-associated infections. Recent events have emphasised the importance of ensuring that there is a strong, centralised function that can rapidly co-ordinate the Department’s response.
98. Mr Buchanan: Many areas have been covered. I welcome the pledge from the Minister and the Department to set the wheels in motion to deliver a more effective, efficient and better Health Service for patients, and to set in place the framework, strategies and targets that are long overdue. Input from local councillors will be a move in the right direction towards helping to eradicate health inequalities. Serious inequalities in the current health system must be addressed.
99. Two issues that always come to the fore are the efficiency savings of £53 million by 2011 and the 1,700 reduction in staff. I want an assurance from the Minister that those staff will come from the already overbureaucratic management-administration system, rather than from nursing and front-line staff who deal with patients; and that there will be no detrimental effect to patients. I am concerned that patients will still have a service that is delivered to the highest standard during the transitional period. Perhaps the Minister will provide clarification.
100. Mr McGimpsey: Yes, I can give that assurance. The 1,700 reduction in jobs will, primarily, be from the boards’ administrative staff and not from such staff as nurses. Dr McCormick will provide the details.
101. Dr McCormick: The first phase, the merger of the trusts, has happened. The unfolding of the job reductions will happen through to 2011; the numbers will be achieved and the savings secured by that date. The process will involve filling the posts by competitive processes as the new organisations form. There will be a process of early retirement or voluntary redundancy so that delivery of the objective of streamlined administration is achieved as smoothly as possible.
102. The majority of savings will come from the reduction of the 18 trusts — all of which have their own finance divisions, HR divisions and other support — to five organisations. Approximately 1,300 of the 1,700 job reductions will come from the merger. The new proposals on the structures for the rest of the sector, which affect the existing boards and agencies, must secure around 400 job reductions. Those will not be achieved by staff redundancies but by suppressed posts. We have had a process of vacancy control for two years, which means that the process can be managed. Although that involves a substantial cost, we are seeking to manage and minimise it to achieve long-term savings. The costs are one-off, but the savings will last for the rest of time. That works as a justifiable value-for-money process, and it delivers the objective of streamlined administration.
103. Mrs O’Neill: Some Committee members touched on commissioning. Minister, you said that effective commissioning is the link between policy development and delivery on the ground. Given that research shows that healthcare improvement starts from the ground up, have you considered other ways, in addition to the health and social services councils, to ensure that the patient voice is heard at all levels, including commissioning and regional-board levels?
104. Do you think that the new regional health agency could contribute to renewing the focus on protecting the funding of such key public-health strategies as Protect Life, which is part of the suicide strategy?
105. Mr McGimpsey: The four elected local representatives will pay an important part in representing local communities. That element was missing before, and it is an important element because those representatives are in a position to represent the views of local communities. Furthermore, the patient-client councils will have an important role. Places will be set aside for local councillors, as well as for the councils representing their particular areas. There will be five organisations; the question of whether that will be one organisation with five subsets or five separate organisations is out for consultation. I am in favour of there being one organisation because a strong regional voice is needed, as well as a local voice.
106. A council and sub-councils seems to be the best solution. However, patient client councils are another important way of enabling people to express their views and to ensure that there is accountability, not merely through the Assembly but through local councils as well.
107. Mrs O’Neill: Does the Minister envisage the new public health agency giving a renewed focus to the protect life strategy and the suicide strategy?
108. Mr McGimpsey: Those strategies aim to reduce need and demand for Health Service resources by encouraging local health engagement. The strategies will benefit greatly from that approach.
22 May 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr John McCallister
Witnesses:
|
Dr Brian Gaffney |
Health Promotion Agency |
109. The Deputy Chairperson (Mrs O’Neill): In the first of today’s two evidence sessions, representatives from the Health Promotion Agency (HPA) will give evidence on the proposals to reform the health and social care system. Members have hard copies of the HPA’s submission and a briefing paper from the Assembly’s Research and Library Services.
110. I welcome Brian Gaffney, the chief executive of the Health Promotion Agency. I invite you to make a presentation, after which Committee members will ask questions.
111. Dr Brian Gaffney (Health Promotion Agency): Thank you. I am delighted to meet the Committee. My invitation reflects the Committee’s interest in public-health issues, and it affords me the opportunity to convey my organisation’s perspective on the proposed changes to structures, which will have a wider impact on public health in Northern Ireland.
112. I will provide some background information on public health in general and on health improvement in particular, and I will then talk about changes to the current structures. I will focus on the proposal to establish a regional public health agency (RPHA), because that will have the greatest impact on the Health Promotion Agency. However, if required, I will also comment on the broader structural reorganisation.
113. Much debate on the health system rightly concerns medical care and treatment — they are the most expensive, demanding and, probably, most important aspects. Public-health issues have increasingly come to the fore over the past two decades. More evidence has been gathered, and that evidence shows that healthier communities are more socially cohesive, economically productive and, interestingly, more involved with local structures, such as local government. That is why we want to improve public health.
114. The Wanless Report and the Appleby Report, which dealt with economic issues that affect England and Wales and affect Northern Ireland respectively, indicated that we will no longer be able to afford such an extensive healthcare system without public-health improvement and an engaged population. Public health and health improvement should be taken very seriously.
115. Public health is a complex matter, but, in order to improve discussion, we divide it into three domains. The first domain is health protection, which covers protection against disease, through immunisation and other programmes, and environmental protection’s contribution to health. The second domain is service development, which deals with ways in which public-health specialists have an input into the development of other health and social care services. That input includes providing evidence, and debating how services can be improved and made more cost-effective. The third domain — in which I operate — is health improvement. When people use the term “public health”, they are usually describing health improvement or health promotion.
116. Since the mid-1980s, health improvement and health promotion have developed beyond the previous individual-based, medical model. That model was thought to be quite straightforward — if people were told what was good for them, they would change their behaviour and, thus, their health would improve. However, that is often not the case with public health, so any model must be more in-depth.
117. We now appreciate that public health — both physical and mental — is a resource that develops over a person’s lifetime. Public health concerns people’s appreciation of their capacities, knowledge, skills and behaviours, and their interaction with their social and economic environment. Health is more complex than, say, whether a person feels sick, so we must find ways in which to improve it.
118. The Health Promotion Agency offers programmes for individuals, because we want to develop individuals’ skills and knowledge, and help them to make healthy decisions. However, we must create environments that enable people to make those healthy decisions. That is why the issue is so important for the Committee for Health, Social Services and Public Safety, and, indeed, for other instruments of government. Consideration of environments and of how people interact requires work in many different sectors. Children and young people must be educated to enable them to make healthy decisions. People need to have a healthy workplace that helps them to make healthy decisions on their behaviours, including on smoking and nutrition.
119. Moreover, safe neighbourhoods are needed. The physical environment must allow people to take physical activity where they feel safe. People must be able to make healthy and affordable choices about food, and so on, and they must be provided with the skills to use those choices. That is particularly relevant to the Committee and the Government, because we realise that the legislative programme has an impact on people’s health.
120. That is most clearly seen in the example of smoking legislation. For many years, those of us who work in public health lobbied for smoking not to be allowed in public places or workplaces, but Government action is required to legislate on such issues in order to allow us to put programmes in place. The current debate on alcohol misuse depends on legislation that will enable people to make choices about alcohol. Changes may be reflected in licensing laws and sales restrictions.
121. Public health and health improvement is so complex, and involves so many people, that no one agency or organisation can be responsible. The issues require much collaboration and many partnerships. The Health Promotion Agency has partnerships at community level with various organisations, such as healthy living centres and community development programmes. We have relationships with many community and voluntary groups, such as Action Mental Health, the Ulster Cancer Foundation, the Northern Ireland Chest, Heart and Stroke Association, Age Concern, Barnardo’s and PlayBoard. All those are important partners of ours in developing public health.
122. The Health Promotion Agency describes its work as being an integrated approach across many areas. Those areas include research, because we need to know what we are talking about, we need to know the evidence for what works and we need to know what is effective. That research should feed into training for professionals, not only health professionals but educational professionals, and even Government professionals who work in the legislative field. We disseminate a great deal of information, to health professionals in particular but also to the public. Some of that is evidenced in many of the programmes with which the Health Promotion Agency is involved.
123. None of that work goes on by itself. It must be linked to what is happening locally, and it must be linked to other organisations. It must be done through many different health settings, including work with local councils, other agencies and local health structures. I hope that the current proposals will facilitate that work. In our various consultation submissions, we said that current structures do not easily facilitate those partnerships or local working. They do not facilitate a truly cohesive relationship between local work and regional work, and they do not necessarily link that work. Therefore, we are neither making best use of scarce funding nor ensuring that good programmes are sustainable.
124. Much good work is taking place, particularly at community level. The Health Promotion Agency and other organisations, such as local councils and other health structures, are doing work at a regional level. However, there is, as yet, no joint-planning approach or agreed funding mechanisms across the partnerships and programmes. There are no common objectives, nor is there joint accountability. There is no real, agreed process for evaluation or measurement of outcomes. It is to be hoped the current proposals will tackle and improve those areas.
125. We consider the current restructuring proposals to offer a major opportunity for change. To do that, much of the work that is done on health improvement regionally and locally must be linked. We hope that, by sharing evidence and by planning programmes together, we will ensure local input as well as regional commitment, and we hope that the two sides can work together. Any proposed new organisations should make public health, particularly health improvement, a priority.
126. Sometimes, in the public-health system, health improvement plays second fiddle to health protection and service development, which often eat up resources. It is important that the proposed RPHA focus mainly on health improvement and collaborate with local commissioning groups (LCGs) and the proposed regional health and social care board (RHSCB). The Health Promotion Agency is unsure of the RHSCB’s commissioning and providing function, and the proposals do not outline clearly the plans for other sections of the health system. For instance, our relationship with primary care and, especially, general practice must be outlined in the new structures.
127. We must accept that we do not want longer timescales or the difficulty in measuring health outcomes to deflect the focus from health improvement. Health improvement is essential — we want to improve individuals’ health and produce a vibrant, more productive — socially and economically — community in Northern Ireland. We need structures that will enable us to help the community. If such decisions were determined by the market, there would not be any smoking legislation or restrictions on alcohol sales, and other development programmes would not exist. Government must take the lead and establish structures that will allow public-health workers to work together with other health-system employees and local-government representatives.
128. Therefore, I look forward to the changes, because there are faults in the current structures. I hope that the debate on the new structures will consider health improvement a top priority.
129. The Deputy Chairperson: You mentioned that adopting a partnership approach is crucial to delivering health promotion. Do you think that the review of public administration (RPA) proposals should impose a statutory requirement to compel local councils to become involved? Would such a measure strengthen health promotion? Would that enrich the council’s forthcoming local community-development plans?
130. Dr Gaffney: The HPA’s work with local government is always conducted on an ad hoc basis; those sectors do not usually work together, and they do not always prioritise public health. In the history of public health, local government has, undoubtedly, played a major role. Through its traditional and regeneration roles, it can enhance public health. Local government also has a long history of community development and of working at a local-community level.
131. The public-health agendas of the Health Service and local government must come together. There are proposals to introduce community-planning rules and to impose a duty of well-being on local government. Local councils should have a statutory responsibility as well as a responsibility to work closely with any new health-system structures.
132. Dr Deeny: I have known Brian Gaffney for a long time — longer than I care to admit — and I am interested in health reform. I am worried that the Health Reform Bill will not be passed by its target date. The intention is that it will come into operation on 1 April 2009. However, its Second Stage is scheduled for the week commencing 23 June 2008, and its Committee Stage is expected to commence at the end of June.
133. I am familiar with the HPA’s work. I spent this morning in Altnagelvin Area Hospital, where I saw a poster, which probably came from the HPA, that I had never seen before. I do not know whether other Committee members have seen it, but it is anti-drink-driving poster carrying a slogan along the lines of “I’m sure you wished you’d crashed at your mate’s”. Such posters convey a message effectively, as do television adverts.
134. I wonder just how many people will be involved in the regional public health agency. Will there be too many organisations? Will it be too complicated? I have heard other people ask whether the proposed RPHA should be incorporated in the proposed RHSCB. What are your views on that? Furthermore, if my figures are correct, even with the RPHA and the RHSCB to come into being next year, the Department of Health, Social Services and Public Safety (DHSSPS) will continue to employ around 400 people in the trusts. Why are those staff required?
135. I have another question on coterminosity. Interestingly, I have changed my tune. Initially, I would have preferred there to be five to seven LCGs, but I now think that, given the proposal to have 11 councils, there should be six LCGs — one for Belfast and one between two for each of the 10 other councils — particularly as they are involved in local councils. That would help secure councillor representation. It is right to base the number of LCGs on the number of councils. For example, a single LCG, coterminous with the trust, would not be adequate for the west. I am sure that Tommy will agree, because it would be a city-dominated LCG. The commissioning body would be in the city, as would the provider. For example, Derry has entirely different needs from the rural populations of Tyrone and Fermanagh. My view is that LCGs should be based on councils.
136. I agree with Brian that the whole idea of LCGs is that they will involve GPs and other health professionals in the area, as well as local councillors — we health professionals are keen to work with health promoters in future. I am sure that Brian will agree that the health and social boards, with which I have worked for well over 20 years now, have, in many cases, not been in touch with the local communities. I mean no disrespect when I say that. Local communities do not know what they are. They adopt a top-down approach, through which decisions are made. Services are commissioned by people who are not really in touch with local communities at all. The new method of health commissioning, and the other new proposals under the RPA, are supposed to have the reverse character and operate in a bottom-up fashion.
137. Do you agree with me on that, Brian? A very good relationship could be formed were the new RPHA to work with the LCGs, which should take over most of the commissioning in future, once the process has bedded down for a few years. Indeed, that were the original plan. Those are all my questions and comments.
138. The Deputy Chairperson: There are plenty to keep you going.
139. Dr Gaffney: I will try to cover all the points raised. I cannot really comment on the size of the organisations, because, in a sense, it is still up for debate, because the consultation has only just finished. On whether public-health agencies should be incorporated in the board, I urge that, at least, there should be a separate health improvement agency. One might think that I am bound to say that because I come from a stand-alone agency; however, the proposed RHSCB, which will contain the LCGs, will be a huge commissioning organisation. Its budget will be huge, if not the number of people that it employs. As I said earlier, health improvement in particular sometimes loses out when decisions and choices have to be made about hospital care, and waiting lists tend to dominate in those circumstances. Sometimes, health improvement and public health must have a separate focus. I am not 100% sure what the relationships will be — I think that a decision has yet to be made — nor am I sure whether the RPHA will be commissioned by the board or the Department. Therefore, I do not know what the relevant sizes will be.
140. However, where important public-health issues, such as alcohol misuse, require discussion, it is important that a focused body raise them. Although it does not seem difficult for an agency such as the Health Promotion Agency to raise issues around smoking, that has not always been the case. In my first ever meeting with Government, an outgoing Conservative Minister with responsibility for health did not allow us to raise the issue of smoking legislation. However, that did not stop us. My chairman at the time, the late Jimmy Hawthorne, who was outspoken on public health, did not hesitate to raise the issue.
141. Sometimes, an independent voice is required. Issues that are coming to the fore include obesity, which will involve the food industry, and alcohol, which will involve the drinks industry. The revenue that the Government collect in tax means that it is sometimes difficult to tell them what needs to be done. An independent body that is at arm’s length from Government could raise the difficult issues. I am not sure whether that body should incorporate the three domains of public health — health protection, service development and service improvement — because those domains must have strong, close links with services that the proposed RHSCB will develop. Therefore, whatever structures are created, it is important that those links be tight, because the body needs to influence what is commissioned. In some ways, I am glad that I do not have to answer the questions about the structures that should be created and the relationships that there should be. However, a separate, independent and health-improvement-focused public-health body is necessary for a range of reasons.
142. The Health Promotion Agency is a regional provider of public health and, because of the current structures, it has no formal mandate to work at a local level. Despite that, much of our work is done at a local level. Dr Deeny is correct to say that people who work at the community level often do not know the functions of their local health and social services board. Recently, we had to work with a range of local groups on mental-health issues and, because we were not 100% sure of their agenda and what they do, and vice versa, that has been a fractious relationship at times. However, the results have been positive, so such difficulties can be overcome. In future, we must ensure that whatever is created is accessible to LCGs.
143. As an aside, we must realise that five or six LCGs will not be local to the communities that they serve; for example, the Belfast Health and Social Care Trust is a huge organisation, with many employees. I am not saying that that trust should be smaller, but, when an organisation covers such a large population, the body that commissions from it will not be able to work with local communities day to day. A way must be found to ensure that those local communities have an input into the process. A series of proposals, such as the community commissioning associations and community development processes, has not solved the problem.
144. Our new local trusts must have their agenda set clearly by the commissioning process that is implemented. They must interact with local communities, because I cannot see any other way for local communities to feed into the process under the current system. It is difficult to get a grasp on local issues, and local people may sometimes, for genuine reasons, find it difficult to get a grasp on regional issues. Nevertheless, both are important and must be accommodated. There is a clear role for input from those who are involved in primary care, especially GPs, who are the top health professionals at a local level. After all, the organisation with which local people are registered is the local practice, so GPs should reflect that.
145. Very few local practices are concerned about coterminosity — many of their patients are from locations that are within different local-government or health-trust boundaries, yet those practices manage to work around that. We must consider every body’s boundaries, but, for me, two points stand out. We must ensure local input — be that through a system that the LCGs develop or through the trusts being told that they must obtain that input — and it must be balanced against regional provision of public-health functions. It is sometimes the case that those functions can only be delivered regionally, so they must be developed in that way. The question of how we strike that balance is difficult to answer, but it is not, and should not be, insurmountable. In a sense, it should be the main driver for creating the new structures.
146. Mr Gallagher: Thank you, Brian, for your presentation. I agree with the point in the Heath Promotion Agency’s response to the consultation on proposals for health and social care reform that the proposed RPHA should have executive powers. It is obvious that the HPA is concerned about which body will have responsibility for health improvement and, if I interpret your response correctly, the HPA believes that that responsibility should remain with the local trust. Given that the trusts have badly managed health improvement, will you explain why the HPA would not want the proposed RPHA to assume responsibility for health improvement?
147. Dr Gaffney: I do not necessarily feel that the trusts are doing that work badly. In many instances —
148. Mr Gallagher: Sorry, that is simply my opinion.
149. Dr Gaffney: Much of the work may be a duplication of, or it may not be linked to, other work. For example, I am working in the system and even I was surprised to find that some of our Investing for Health partnerships, even at a local level, were not really aware of the work that their local healthy-living centre was undertaking. It did not seem to be possible to co-ordinate the two, because they were funded and managed separately, and did not seem to be part of the same system. Therefore, it is not the case that the trusts are doing bad work, but it may be that they do not co-ordinate.
150. The HPA feels that we still need health-improvement and health-promotion staff based in trusts, because we see no other way in which local links can be established. In any part of Northern Ireland, it is possible to find examples of work going on between local community groups and local health trusts. A regional organisation would not be able to replicate that work.
151. Even if all health-improvement staff were relocated from trusts and based in a regional agency, at some stage they would have to return to local level and work with the local trust. Therefore, as far as I am concerned, it is a question of whether we can ensure that the work that those people do ties into a common agenda and that it is subject to a common system of accountability and a common planning process.
152. If the proposed RPHA is to commission health improvement, it must ensure that trusts, through their health-improvement staff, are meeting the regional agenda and that their work complements it. I see no point in reorganising the existing structures to make health-improvement staff work at a regional level, only for them to return to work at trust level subsequently. However, greater co-ordination is needed.
153. Mr McCallister: We all agree that we must make huge strides to make the entire population aware of public-health issues.
154. I am interested in following up on questions about tying in the issue of health to the proposed new council structures. Would councils play a strategic role, using their structures as a delivery mechanism to get across the message?
155. Dr Gaffney: There are examples of local councils taking the lead role in public-health programmes and in the work of Investing for Health partnerships, and those are good examples of what councils should do at a local level. Regionally, we have engaged with councils on issues such as workplace health, and that has been a fruitful exercise. Therefore, the public-health role of councils could be played at strategic and local implementation levels.
156. Councils have vast experience of working with their local communities, but some public-health workers may feel that if we encourage that partnership too much, we will hand over public health from the health system to local councils, thereby losing something. However, I regard such a partnership as a strength rather than a weakness. If we can ensure that the councils, whatever their number or size, prioritise local public-health programmes and issues, that will only enhance the process. Councils must work in close partnership with the health system, but they have slightly different perspectives and structures, so they could assume responsibility for many areas. Although we have developed a good training programme with GPs to address fuel poverty, much of the real work on tackling fuel poverty should have local-council input.
157. Fuel poverty is a health issue. Many people who endure fuel poverty develop ill health, and some of those people die a result of the cold weather. That is only a small example, but it is one that local councils could implement locally, by improving the housing stock and providing grants. Therefore, there is a role for strategic input at both council and local implementation levels.
158. Mr McCallister: I agree that councils have a huge role to play, but some are better than others at dealing with such issues. How do we ensure that the programme is delivered evenly across Northern Ireland?
159. Dr Gaffney: Again, I would look to examples of good work elsewhere. I would not normally hold up England as being somewhere with examples of good public health. However, it has tried not only to have coterminous boundaries with its health and local government structures but to have joint planning. Therefore, local authorities there have a community-planning brief, but they work to that within existing health structures.
160. Some local authorities appoint a director or head of public health, who is jointly appointed with the local health trust, which, in England, is known as the local primary-care trust. The model is one that we could use, in order to ensure that community planning, for example, were done jointly by the health system and local authorities. That would guarantee accountability, with joint funding and programmes. People would try to ensure that it were evenly spread and that no inequity existed in the work done in Northern Ireland.
161. Mr Easton: You touched on my question. Will the proposal to transfer public-health functions from the boards and trusts to the new RPHA lead to more effective delivery of public-health services for Northern Ireland?
162. Dr Gaffney: We must examine more closely public-health functions in boards and trusts. Currently, the health boards are involved in commissioning and in providing some public-health and health protection programmes, and they provide some health improvement. The trusts, as the providers, are involved in all three areas. If nothing else, reorganisation should provide some clarity on who commissions and provides the different local and regional services, which may lead to better co-ordination and a more cohesive approach to public health.
163. Of the three public-health domains that I mentioned earlier, the Health Promotion Agency’s focus is on health improvement. I do not want whatever new system is created to allow the boards’ current public-health functions — service development and health protection — to dominate. That could mean that they take their eye off the ball when it comes to health improvement. However, bringing the functions of the health boards and trusts together in order to match them to local input will be an improvement.
164. The Deputy Chairperson: Fewer Committee members than normal are present today, Brian, so that concludes the questions. Thank you for coming; it has been most helpful. The Minister is attending next week’s meeting, and you have given us some questions to put to him.
165. Dr Gaffney: If Committee members have any further questions, I am happy for them to contact me at the agency, and I will supply information on public-health issues.
166. The Deputy Chairperson: When the legislation comes before the Committee next month, we will write to you to request feedback. Thank you.
167. Dr Gaffney: Thank you very much.
19 June 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Rev Dr Robert Coulter
Dr Kieran Deeny
Mr Alex Easton
Mrs Carmel Hanna
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Ms Claire Higgins |
Institute of |
168. The Deputy Chairperson (Mrs O’Neill): Our first evidence session today on the Department of Health, Social Services and Public Safety’s proposals for health and social care reform comes from the Institute of Public Health in Ireland. A copy of the institute’s response to the proposals, its report entitled ‘Towards Healthier Societies’, and a briefing paper from Assembly Research Services can be found in members’ pack.
169. I welcome Dr Jane Wilde and Ms Claire Higgins. Jane Wilde is the chief executive of the Institute of Public Health in Ireland, and Claire is the public health development officer. I invite you to give a short presentation of approximately 10 minutes. Members will then have the opportunity to ask questions.
170. Dr Jane Wilde (Institute of Public Health in Ireland): First of all, thank you very much indeed for asking us to come and give evidence. We are delighted to be able to come to the Committee, because we think that the proposals are such an important change issue in Northern Ireland. We also think that politicians have a huge role to play in health and social care — particularly in the public-health agenda, which is what we are interested in as an institute of public health.
171. I will say a few words about us so that the Committee is aware of our perspective. Claire Higgins, who works in the institute with me, leads on our health impact assessment programme. She is particularly interested in looking systematically at how different policies, programmes and projects affect the health of communities, particularly the most vulnerable people in those communities. She worked previously in a local strategy partnership in Antrim and also in the voluntary and community sector.
172. I am a public-health doctor. I worked in the health system in Northern Ireland, and then I was the founding director of the Health Promotion Agency. Later, I became an executive in establishing the Institute of Public Health, which was set up to promote co-operation between North and South.
173. We have been asked to say something about the proposals for health and social care reform. There are five main strands to the Minister’s proposals, but I will confine my comments to just three areas: the proposed regional health and social care board; the proposed regional public health agency; and proposals for increased democratisation of the system.
174. It is important for us to think about whose eyes we are looking through when we examine the proposals. Therefore, I thought that it would be useful to outline the most important issue, which is whether the proposals will make any impact on community health inequalities. That is the whole purpose of the issue. When I talk about health inequalities, I am talking mainly about socio-economic inequalities; in other words, the huge gap between the rich and the poor. Therefore, the first issue is whether the proposals will make a difference.
175. The second issue is whether the proposals will help to use the mammoth amount of expertise, commitment and experience that exists in Northern Ireland. The third issue is to think about how the Institute of Public Health can contribute, and whether the proposals will allow us to contribute to better health in Northern Ireland.
176. We welcome the proposals. They provide a way ahead for Northern Ireland. They are radical, but they are sensible and timely, and can be made to work.
177. With regard to the proposal for a regional health and social care board, the functions of commissioning, financial management and performance management are sensible and rational, and no further functions should be added. There are huge issues with regard to commissioning. We welcome the issue of local commissioning and the role of primary care and others in that. Commissioning should cover the different fields of public health. Therefore, we are talking about how we protect people from infections, and so on, how we help people to improve their health, and how the services that we deliver are directed to, and planned for, the most vulnerable people.
178. There must be strong links between the board and the proposed regional public health agency, but it is not entirely clear how those links would be taken forward. We have some ideas about how that might happen, but, in the absence of clear proposals, the Committee may have views on the issue.
179. Our view is that there must be a strong relationship. We would like the proposals for the regional health board to include a requirement that commissioning plans go through the regional public health agency when they are being signed off by the board. Therefore, they should be checked from a public-health perspective.
180. The proposals have a strong focus on increased democratisation, in particular trying to strengthen the role of local government. Claire has a wealth of experience in that area, and she will say a few words about that.
181. Ms Claire Higgins (Institute of Public Health in Ireland): The institute welcomes calls for closer links with local government and supports that action to strengthen its role in improved public health for communities. There are already good working relationships between local communities and local authorities, and they should be supported and strengthened to help to develop and shape services for improved quality of life.
182. That could be done by community planning and the power of well-being. That presents an opportunity to create healthier communities and to address health inequalities. It is essential that the regional public health agency is strongly involved in the development of the community planning framework. It is important to ensure that Investing for Health targets for tackling health inequalities are reflected in the planning process, that they complement and build on existing area-based partnerships, such as the Investing for Health teams and the health action zone teams, and that community planning targets should reflect the social determinants of health in all action areas — for example, in transport and education — and not just through health actions.
183. The institute recommends that community plans are signed off by the regional public health agency. That will ensure that health is adequately addressed in each of the area plans.
184. Finally, local government is in an excellent position to engage in health impact assessment (HIA), which is a methodology to assess the health impacts of an identified proposal. The institute, with the Department of Health, has led in HIA in Northern Ireland, and the regional public health agency has a key position to support conducting health impact assessments.
185. The institute has been closely involved in the health impact assessment in the west Tyrone area plan, which is funded by Omagh and Strabane District Councils, and the Western Investing for Health partnership. The assessment will engage with key stakeholders to look at the health impacts of the plan, which will be in place until 2019.
186. Therefore, HIA presents a way of working that engages local communities, local government and other sectors that need to take into account the impact of their work on health.
187. Dr Wilde: The proposed regional public health agency is very dear to our heart. I have been working in public health in Northern Ireland for almost all of my working life. I see this proposed agency as a major opportunity to bring together the different aspects of public health, and to give public health a much stronger voice.
188. I welcome the proposal to put public health at the centre of these proposals, and I note that the Chairperson of the Committee has welcomed the proposals. I hope that the Committee will feel able to do likewise as this develops.
189. The functions that are set out are the right functions for the regional public health agency. However, there must be a stronger function relating to research and information. Unless we have good information across a range of issues, it will be very difficult to be sure that we are doing the right thing and in the right way.
190. The agency must be multi-professional. That means bringing in not just public health doctors like myself, but other members of the health-and-social-care family, as well as economists, behavioural scientists and anthropologists to consider how to shift Northern Ireland’s rather poor health record. I cannot think of any professional group that does not have a role in public health.
191. The agency must also be multi-sectoral. Public health is not about just the Health Service, as the Committee well knows, but about other areas such as housing, education, agriculture, transport and rurality. This organisation must be outward looking and forward looking. There is here a fantastic opportunity to create in Northern Ireland something that is truly world class.
192. I have just come from an international event at which Queen’s University, the institute, and the Community Development and Health Network were chosen as one of five centres across the United Kingdom to create a centre of excellence for public health, bringing £5 million into Northern Ireland in order to build capacity. That shows what can be done when we join together: we can beat other people and be not only good but really great.
193. We are very enthusiastic about the proposals, and we look forward to contributing to making them work. I have not mentioned anything about the institute’s work, but Committee members have copies of our first 10-year report. Rather than talking about the institute’s contribution, I hope that we might come back and say what the institute is doing for public health in Northern Ireland and across the island of Ireland. Thank you very much.
194. The Deputy Chairperson: Thank you. The Committee welcomes your enthusiasm for the proposals and the way forward, because we want to make an impact on the community.
195. How do you visualise the healthy living centres, which you evaluated, fitting into the proposals?
196. Dr Wilde: Healthy living centres, and the many other partnerships in Northern Ireland, whether Investing for Health partnerships, community development partnerships, or Healthy Cities partnerships, have a key place with regard to the proposals.
197. As the term “public health” has become better known, and as action locally has flourished, there is now a range of partnerships. Healthy living centres, for example, have made a big impact locally, as the evaluation states. Partnerships that work should be strengthened, and the proposals not used to leave them behind. We are very keen to see the existing successful partnerships being strengthened, resourced and supported. For too long, partnerships have had to exist with minimal resources. I recently met the Community Development and Health Network; it does not know how much money will be available next year. That is despite that fact that that organisation is a remarkable network that brings community-based organisations together throughout Northern Ireland. We are very keen to see existing successful partnerships being better supported.
198. The Deputy Chairperson: With your background in the Health Promotion Agency, you will be aware of its five core aims. Do you think that the proposals will subsume and build on the current role?
199. Dr Wilde: That is a good idea. If people work in an organisation, they have a commitment or loyalty to that organisation. They might not want to see organisational shift. However, it is the right way to go because it can strengthen the work that has been done in the Health Promotion Agency by bringing a stronger element of the other aspects of public health — the health protection aspect, for example, which provides protection against infectious diseases. It also has a stronger role in ensuring that the services that are commissioned throughout Northern Ireland have a strong public health function. Including those considerations will be very important in strengthening the role of the work that the agency does.
200. The Institute of Public Health has had a very strong role in health intelligence — the information side of things; forecasting new conditions; and evaluation, as you mentioned. We can continue to bring that to the new public health agency, but we will do that from a slightly external perspective because of our North/South links.
201. Mr Buchanan: I thank Jane and Claire for coming to the Committee today. There is no doubt that these changes will be challenging for the Department, the Committee and to folk like you with regard to the delivery of better health provision right across Northern Ireland.
202. What input did you have into the development of the Minister’s proposals for the restructuring of the Health Service? Community planning and well-being were mentioned. You also talked about the West Tyrone area plan and the work that was done with various stakeholders between Omagh District Council and Strabane District Council. Do you think that the joined-up working between the key policy stakeholders will provide a better, improved service right across Northern Ireland?
203. You also spoke about the good partnerships that are already in existence and about how those need to be strengthened as they are currently underfunded. Do you see the new proposals strengthening or having a detrimental effect on those good partnerships?
204. Dr Wilde: Claire will comment on the community-planning side of things, and then I will cover some of the inter-sectoral issues and answer some of the questions about how we have been involved.
205. Ms Higgins: We have been working in partnership with the Community Development Health Network, the Northern Ireland Council for Voluntary Action (NICVA) and the Health Promotion Agency to draw up a briefing paper for what politicians should look to include in community planning. There are 10 action points, and those should be assessed against community plans so that health inequalities can be addressed through community plans. That is a piece of work that we have started, and we will approach political parties in the autumn. Hopefully, that will filter down to communities.
206. The new proposals should strengthen the partnerships that are in operation. Using the example of community planning, the Investing for Health teams developed a wealth of resources, including baseline health statistics. All of that information needs to be included in community planning. The process should strengthen the partnerships that are in existence.
207. Dr Wilde: I will pick up on a couple of other points that were mentioned, such as how we have been involved. Like others, we responded to the consultation. Because we are primarily funded by the two Health Departments, North and South, we also have good relationships with the Chief Medical Officer’s office, for example. We have had an input into the thinking about public health, and we have had a good chance to put our views forward and hope to continue to do so as the process rolls out.
208. New functions that have been proposed for the regional public health agency include a stronger role in resourcing and help to support local government in public health. It is important that funding goes to the new agency for that function. The proposals are scripted in such a way that all the money goes through the new regional health and social care board, which will be the main funders of the system. However, I think that some money should go directly from the Department of Health to the new regional public health agency to protect the idea of public health and health improvement, because, for understandable reasons, it generally gets a low priority compared to acute services. Therefore, it is important that a strand of money goes directly from the Department of Health to the regional public health agency. I hope that I have answered some of your questions.
209. Mr Buchanan: Yes, you have covered most of the questions.
210. Dr Wilde: I will be happy to follow up any questions that I have not answered.
211. Dr Deeny: Thank you for coming before us. The issue is of great interest to me, because I have been working in the Health Service for years. It is potentially a very exciting time if we get it right. Rather than waiting for disease to occur and then trying to prevent it, the focus will be on health promotion and disease prevention, as well as a link up with other areas, such as local government, community groups and leisure centres, walkways, cycleways and even mental health. There should be facilities for people, both young and old, living in rural communities who are isolated and lonely. Such facilities would help to prevent ill health.
212. How big will the regional public health agency be? You mentioned that the agency should have a say before services are commissioned, but that worries me. Are you saying that it should have a commissioning role, or are you saying that it should have a veto?
213. I have asked the following question before, but I have never been given a clear answer to it. I know Dr Brian Gaffney well, for example. There is a major role in public-health promotion, but how many people will be employed by the regional public health agency? Should they not be part of the regional health and social care board?
214. I will be celebrating an anniversary tomorrow — I will be 28 years qualified — and I have worked in the Health Service for more than 25 years. Over the years, I have seen many great ideas get bogged down in bureaucracy. What worries me is that there will be lots of wonderful ideas, but there will be another huge agency that will be separate from the five local commissioning groups. For instance, the Western Health and Social Care Trust has four tiers of management. New bodies always have fancy, great ideas, great strategies and protocols, but it is different on the ground. I do not want my hopes being built up for the future. We cannot afford to build up people’s hopes nor can we afford duplication, with people trampling on one another’s toes.
215. Dr Wilde: I do not want to get into competition over how long people have been qualified. In many ways, I have total empathy with the points that you make. The overall point that I would make is that you do not run systems, which is what we are really talking about here, by deciding what organisations you are going to have; you do it by deciding how those organisations link up, what kind of relationships people have and what kind of processes you build up.
216. With regard to your points about bureaucracy and waste, and so on, when the four boards are scrapped and trusts are more streamlined, the proposals will ultimately reduce the number of organisations, rather than create more. The issues are the relationships between the Department of Health, the board, the agency and the trusts. The practitioners will feed in through those organisations.
217. As I understand it, commissioning will be done by the board, but it will need public-health advice, and that advice should be provided by the public health agency. There must be a contractual relationship between the expertise of the public-health agency and the needs and requirements of the board. I am not sure how that might best be done; some of the staff of the agency will have to either be seconded, or have joint appointments, or it may all be a matter of grace and favour. That causes a few complexities in regard to how those different organisations are governed, but a lot will depend on the senior leadership in the board and of the public health agency, because if those two organisations do not work in a streamlined and sensible way, any contract that is put in place will be inappropriate.
218. I actually think there is a need for some tension between the health and care system and the public-health system. Public health is all about the organised efforts of society, but if I go to see a GP or a nurse I want the very best for me. There is a healthy tension between what we do overall in society and what each individual practitioner is going to do. I do not think that everyone is going to agree about every detail of the system, but that is OK.
219. Dr Deeny: I have an issue with the number of people that will be employed by the proposed agencies.
220. Dr Wilde: To be honest, I am not actually sure how many people are being proposed.
221. Mrs Hanna: A staff of 200 is mentioned for one of the bodies.
222. Dr Wilde: I do remember a figure of 400 staff for the regional health and social care board. I have a vague notion of that, but I would have to check — I cannot remember.
223. Dr Deeny: I cannot understand the numbers. For example, there will be 16 staff in each of the local commissioning groups, making a total of 80, and then there will be 400 staff in the regional board; it seems an awful lot, never mind those in the Health Department in Belfast. That is my worry.
224. Dr Wilde: It would be very useful if the Committee considered the issue of the actual breakdown of staff in those organisations. I do not have any inside information about that.
225. Mrs Hanna: Jane, Claire, you are very welcome. I have some of the same concerns as Kieran, even though I do feel that it is a very exciting time. In all the time that I have been on the Health Committee since 1998, this is the first time that I have heard public health being talked up, from the Chief Medical Officer down. There does seem to be more of a focus on that, which is very welcome.
226. The setting up of those two bodies does seem to be quite complex. In one way, it is good to have a separate public-health body, as long as it actually has a clear role. The arrangements certainly cannot be voluntary; there must be statutory partnerships and links established. The proposals do need to be checked out; in fact every proposal that will involve so many staff should be checked out. We do not want to be overly bureaucratic. That problem has arisen with so much of our legislation, such as equality legislation, and we must ensure that it does not become a box-ticking exercise, but genuinely does make a difference. That is particularly the case with regard to local government — the Minister has said that he plans to have local elected representatives on the proposed new bodies.
227. We want to ensure that the proposals actually do make a difference this time, particularly regarding health inequalities. They must tackle the challenging lifestyles and make a difference to the people who most need help, for they are the very same people who suffer from the health inequalities. If we do not make a difference on those issues, we are really not making a difference at all.
228. The Committee must tease out from the Department exactly how the proposals are going to work. We must look at the family tree of each of the proposed organisations to ascertain who is in it, what are they doing, and where they are making links with other organisations. At the end of the day, the whole idea of the review is to make the system better for patients. Early intervention and prevention must be at the heart of that. There is a lot of work to be done, and we in the Committee must work with the Department to tease out the details. Otherwise the proof of the pudding will be in the eating, and it may be too late then. We must ensure that statutory links are established between the relevant organisations. It cannot be the case that there will only be links between the bodies if someone feels like consulting.
229. Dr Wilde: It would be terrible to set up an organisation, such as a public health agency, but give it no power or influence. That would be a waste of money.
230. Mrs Hanna: The patients and people must be kept in mind.
231. Dr Wilde: The community must also be kept in mind. I am glad that you raised the issue of health inequalities, because it is at the core of public health. In comparison with other countries, it is socio-economic inequalities that hold back Northern Ireland. As well as the terrible suffering, the loss of life and the impact on individuals, society and the economy, socio-economic inequalities stop us from having better health and being able to be proud of that
232. Mrs Hanna: That is why it is so important to have the health action zones.
233. Dr Wilde: Yes.
234. Mrs Hanna: We know the importance of early intervention and see it in primary care all the time. For example, if older people require a physiotherapist or an occupational therapist, they need that service immediately, not in six months’ times. Early intervention in such cases can keep people out of acute beds in a hospital, but it does not happen. We must try to change that.
235. Dr Wilde: It is also important that community needs are addressed locally. That way, people can plan and manage their own healthcare organisations and health.
236. Mrs McGill: I thank you for the presentation, you are both welcome.
237. Claire, you mentioned the partnerships and referred to the Western Health Action Zone and Western Investing for Health and the relationship between those bodies and the councils. I declare an interest as a member of Strabane District Council, and it was great that you used my area as an example. I endorse what you said — I am well aware of the good work that is done in that area.
238. Strabane District Council recently received a presentation from a group of dentists who were very keen to be represented on the commissioning groups. In your submission, you state that you want a range of bodies and professions to be represented. I want to put on record that the council received that presentation and that I am passing on what was said, which concurs with the points that you made.
239. You said that the role of councillors and elected members on the commissioning groups has not been established and requires clarification. What should the role of elected members be on those commissioning groups?
240. Dr Wilde: We would very much like to see elected representatives to be on all these groups, which is what the Minister has proposed. However, we do not know how the membership of the groups will be chosen, so we do not really have a view on that. We hope that the Committee will help us decide.
241. Mrs McGill: The commissioning groups will be made up of 16 members — what would be an adequate number of elected members on a commissioning group? I ask that because the number of councillors in council areas varies, and the change in the structure of local government will also have an impact.
242. The Deputy Chairperson: No pressure.
243. Dr Wilde: What do you think?
244. Mrs McGill: I have already declared an interest, so I cannot comment.
245. Dr Wilde: I do not know. Although we support the proposal for elected representatives on commissioning groups, it is important that membership also includes people from the local communities. I recognise the local role of councillors, but we do not want the number of elected representatives to be at the expense of local people. However, that does not answer your question.
246. Mrs McGill: Geographical spread is important in choosing the number of elected members on commissioning groups.
247. Dr Wilde: That is absolutely correct. Geographical spread, how people will be chosen, whether those people will be independent, and how the system will work are all issues that have to be considered. However, that is part of what is needed in public health — more democracy, community participation and political thwack.
248. Mrs McGill: Will an elected member sitting on a commissioning group be independent? I ask that question because that individual has been elected to represent a particular geographic area.
249. Dr Wilde: This is not the only area where these issues are being debated — they apply to all sectors.
250. The Deputy Chairperson: Many of the questions that have been asked will be relevant in the upcoming evidence session with NILGA.
251. Mrs Hanna: It is important that the health systems either side of the border learn from each other. Indeed, the Committee for Health, Social Services and Public Safety has already met its Southern counterpart. Where does the Institute of Public Health in Ireland fit in, particularly regarding the regional public health agency?
252. Dr Wilde: I have not discussed what we do in any detail, and I would love to come back and do that at some stage. There are three areas in which we can help to strengthen public health in Northern Ireland. First, the same public-health issues and challenges are faced throughout the island. I did not elaborate on those because the Committee is already well aware of those. The health systems, North and South, can meet those challenges by sharing resources, where appropriate — for example, media resources, skills and expertise, and so on.
253. Secondly, things are done differently, North and South. There is, therefore, an opportunity to learn from that and to lever. The smoking ban is a good example of that; its introduction in the South helped us in Northern Ireland realise that it could work here too.
254. The third issue is about people crossing the border for treatment. The border should not undermine anyone’s health. If people in the North need to access services that are available in the South, the necessary arrangements should be made to make that possible, and vice versa. That would benefit people here and in the South.
255. The Institute of Public Health in Ireland essentially works in three areas. Research and information is one area. There is a lot that I could say about that, but this is not moment. The second area is capacity building, including training, sharing programmes, and health impact assessment, which Claire Higgins mentioned. The third area of work concerns policy and policy advice. We have a lot to learn from each other, and also from outside Ireland.
256. The proposals provide an opportunity for the Institute of Public Health to help with the new arrangements in Northern Ireland. The institute has strong academic links. We ensure that the research carried out is appropriate and addresses the relevant matters and that the results are well communicated.
257. The Deputy Chairperson: Thank you very much. I appreciate that today’s session has been very much focused on the RPA. Therefore, we will invite you back another day to discuss your specific role in further detail.
258. The relevant legislation will probably be proposed in the next few weeks, so you can come back to us over the summer with any comments that you wish to make on that.
259. Dr Wilde: We will be delighted to follow that up; thank you very much for giving us the opportunity to do so.
19 June 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Rev Dr Robert Coulter
Dr Kieran Deeny
Mr Alex Easton
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Witnesses:
|
Mr John Matthews |
Northern Ireland Local Government Association |
260. The Deputy Chairperson (Mrs O’Neill): I welcome Heather Moorhead, chief executive of the Northern Ireland Local Government Association (NILGA), John Matthews, vice-president of NILGA, and Suzanne Wylie of the chief environmental health officers’ group.
261. Mr John Matthews (Northern Ireland Local Government Association): I thank the Committee for receiving us. This is an example of how the relationship between local and central government is growing.
262. We welcome the Programme for Government and the changes that are happening. NILGA wants to contribute to those changes and play its part in the whole range of services that are being delivered to the community. I am standing in for Arnold Hatch, who, at the last minute, had to go to England on business.
263. We think, and very much hope, that our vision for local government accords with your own in that we want an innovative, modern approach that is supported by the partnerships and relationships in Northern Ireland’s new dispensation between local and central government on modern, citizen-centred public services and greater efficiency and effectiveness. We want to see the breaking down of the silo-type management of services, and very much support the hub-of-the-wheel model in community and health services and other service delivery. We see local government representatives playing a key part in that. NILGA believes that that should be at the core of the changes.
264. We have met Health Minister McGimpsey on this issue, and he assured us that his vision is for greater democratisation of local health bodies in the delivery of services. We believe that he agreed with us that local government representatives should account for at least 50% of the membership of those bodies. In that way, the local community will have ownership of the services, feel more involved, have better feedback, and enjoy an improved sense of well-being.
265. There must be a clear understanding of the roles of board members and of public and council representatives. Members who are working on health bodies must be properly supported and briefed in order that they can give responsible and rational answers to the press and public.
266. Reporting structures are central to communication between central Government, local government and service deliverers. They are at the heart of the image of politicians, both local and in the Assembly. All of us — in this respect, we are all in the same family — receive criticism and a rough press. However, if the issue of reporting structures is properly addressed, that will be to everyone’s benefit — good for services, for citizens, and for those sectors of Government that are delivering the services. In addition, we want wider emerging arrangements across central Government.
267. NILGA is producing a paper for the strategic leadership board, which has been set up by the Minister of the Environment to deal with the implementation of the review of public administration (RPA) and bringing the 26 councils into 11 councils. The paper, which deals with community health issues, is expected to be ready in about eight weeks’ time, and we will forward it to the Committee.
268. Ms Heather Moorhead (Northern Ireland Local Government Association): A lot of people are involved in local authorities, and the RPA has taken about five years, with various ups and downs. One of the prizes of the RPA was coterminosity, in order that services could be streamlined. Many of our colleagues are running three or four partnerships that have different arrangements. A lot of time is required in order to develop those relationships, which distracts from getting a key plan for service delivery.
269. Four councils are somewhat out of step with the health trusts: Limavady, Newry and Mourne, Dungannon, and Castlereagh. If it is in the gift of the Department to examine that situation, we would welcome that. If that is not possible at this stage, there should be some negotiation and discussion with NILGA on how to implement community planning and develop suitable arrangements. Part of progressing community planning is streamlining the approach to create fewer partnerships. We want to work with the Committee to consider how to do that in a way that does not involve lots of staff running around to different kinds of organisations.
270. Ms Suzanne Wylie (Northern Ireland Local Government Association): I emphasise the need to explore the opportunities for working in the new community planning process that will come into operation under the review of local government and the advantages that it will bring by streamlining and integrating services locally. It will also provide greater public engagement and local accountability.
271. Community planning of health improvement and preventive health measures has a fundamental role in addressing health inequalities and focusing on integrating health improvement, protection and promotion. It also has a role in ensuring that the health impacts are taken into consideration in every public policy and by all public services. We welcome the establishment of a regional public health agency with a central role in co-ordinating the integration that, according to the consultation document, will be both regional and local. We welcome the local support for local government that the document suggests.
272. Local government should be regarded as civic leaders and agents of delivery, as that is where the community planning framework creates the hub to ensure integration of services, including those that have an impact on health improvement. However, local government should also be seen as an organisation that, in conjunction with partners, can deliver health improvement. It has responsibilities for environmental health, health improvement through the provision of leisure and open spaces, community development, good relations, economic development, and so forth. After 2011, local government will also have regeneration and planning powers, et cetera.
273. Local arrangements must include good and balanced two-way communication and joint working in community planning. Rather than the one-way consultation process that the consultation document suggests between the community planning organisations and the regional public health agency, we want a two-way communication process; that should be included in the legislation.
274. The local community plan must also be influenced and established in the light of regional policy — none of us would argue against that. The community plan can help to strike a balance between regional policy and local need. We would welcome the exploration of innovative delivery approaches at local level and the concept of local joint public health units or teams that would have joint ownership with the regional public health agency and local government. Those could be physically co-located, with the possibility of joint appointments. I am happy to take questions from the Committee on how that would pan out in the future.
275. I am keen that best practice from other regions be considered — many joint working arrangements exist in England, Scotland and Wales. All have slight variations, and each has disadvantages and advantages. We recommend that those arrangements should be considered and that the best should be adopted.
276. During the past several years, there has also been considerable partnership working on health improvement, which should be built on. There is lots of good practice from which to learn. It should be built on in a way that links with the regional public health agency and the community planning process at a local level. Integrated health and well-being partnerships that are aligned to the community-planning framework should be developed on an appropriate geographical basis. We want to highlight the need to involve local commissioning groups and patient/client councils in that process to develop and deliver community plans.
277. Finally, local government wants to see the development of some community planning pilots from 2009, which is, obviously, when the health structures change. Local government structures will not change until 2011, but we would like some pilots to be introduced during the interim in order to test some of those models and arrangements for integrated working and also to build the capacity of local government during that period. We suggest that the health structures design team should work closely with the local government modernisation task force on order to take some of those arrangements forward.
278. Ms Moorhead: One benefit of local government is that it can think about health in its widest sense. A problem that we have found is that thinking on health ends up with the health profession — it is about sickness. In fact, health is about economic development, social cohesion, fuel poverty, crime, and so on. The language that is used and the way that business is done are important. If health remains simply a matter for the health profession, then it is somebody else’s job. Our belief is that if that were co-located with councils, and informing community plans, those plans would have a “health wedge”. The added value, or “big win”, from that is that the wedge — the thinking on health — would begin to influence all of the other areas, such as economic development, parks and leisure, and all of those kinds of strategies.
279. We welcome the regional public health agency, because it will bring about better intelligence and information. We will be able to see how our policies make people’s health and well-being better or, indeed, worse. Sometimes, work can be done on health strategies when, in fact, the economic development policy has a bigger impact on people’s health than anything else. Hopefully, community plans will have a focused approach on health, with health professionals working with environmental health officers in an influencing role and an added, innovative way of working.
280. Another advantage is that councils are innovative and close to citizens. They find ways to work together to bridge gaps, and find resources to plug those gaps, when other agencies cannot. The genesis of health action zones throughout Northern Ireland was based on where there was co-location and shared thinking between the health sector and local government. Lots of creative things happened. In fact, the health action zones created a culture for that, and innovations began to be piloted throughout the rest of Northern Ireland. We have, therefore, learnt from others and we are pushing at the right doors in order to try and find a more integrated approach.
281. Another advantage of having that within councils is that we would get all the things that we have discussed — economies of scale, back-office services, and so on. They provide the support structures, but we also get the intellectual philosophy right. Therefore, we welcome proposals for a much stronger and closer role for local government. We have begun to experience that relationship. Instead of there being a stand-off, which is usually the case, there is a realisation that everybody is responsible and that we must work together in order to make progress.
282. Mr Matthews: We do not want to usurp in any shape, form or fashion the strategic direction that will be set by the Assembly. It is good to have the opportunity to have dialogue in order to determine how services can be delivered and measured on the ground. One thing that will make a difference to our ability to make improvements and to interface with central Government is the power of well-being in that legislation. There are other features of the legislation, such as the clean neighbourhood agenda, which are more pertinent to what we do. However, it all feeds into the better lifestyle of the citizen. We are grateful for the opportunity to discuss that. Hopefully, we will have more opportunities to interface with the Assembly and to lay out the thinking of local government.
283. The Deputy Chairperson: I agree that more integration, co-operation and focus are needed in order to tackle health inequality, which can be done locally. You talked about the benefits of community planning. However, there is no legislative requirement on councils to consult. The main aim of community planning is to engage with people in communities. The absence of that legislative requirement will cause problems and disparity, depending on where one lives and how focused councils are on encouraging co-operation. Will that be a problem, or will we see improved outcomes?
284. Ms Moorhead: The style of community planning is happening all over Northern Ireland and it is beginning to show benefits, although it is frustrated by the fact that there are so many stakeholders. Some are coming to the table and some are not, and we are trying to move forward. We will see a massive difference when we get the statute and there is a better understanding and a framework. These issues are massively important. We must understand how to target things locally. We want to provide an even level of service for equality purposes, but we must also be clever about how that is done locally. The things that are happening in Strabane are not necessarily the same as those happening in Belfast; that is why we need community planning. We will have 11 new councils and there will not be the same problems throughout each borough: some towns may be quite wealthy and others not, so we will need community plans to tackle those differences. We hope that community planning will provide a level of flexibility.
285. Ms Wylie: The modernisation agenda for local government will address the issue of mechanisms for community engagement. Neighbourhood delivery structures have been put into play by many local authorities in Great Britain, and they join up neighbourhood service delivery with other agencies. That is the direction that we see local government moving in.
286. The Deputy Chairperson: I welcome your suggestion of a pilot scheme. There are some good and bad examples of neighbourhood renewal, which involves several agencies coming together. Some councils have divorced themselves from that altogether. We must learn from good and bad practices and move forward.
287. Mr Matthews: Minister Foster’s statement, when she was Minister of the Environment, was very pertinent in that the changes taking place are not an event but a process. We are all subject to that process, and the target is an improvement of the way in which we live and work together.
288. Dr Deeny: As a GP, I am greatly interested in this subject. The old days of waiting for diseases to occur and treating them are disappearing rapidly. That is good to see. It is about health promotion and disease prevention, and that is where local government comes in. I am delighted to see that happening. Ms Wylie referred to facilities for young and elderly folk to encourage them to exercise, which, in turn, encourages mental well-being.
289. In your submission you referred to local government having a function of scrutinising the delivery of health services, and I could not agree more — that would be wonderful. Coterminosity will come into effect in 2011, and we should be thinking about our local commissioning groups (LCGs) being coterminous with our councils, not our trusts — and I mentioned that to the Minister the last time he came to the Committee. I would like to see six LCGs eventually, one in Belfast and five others, each with two councils. The Minister told the Committee that the plan is for four local councillors, which would be two from each of the new councils. That, to me, would make more sense as there would be an overlap of trusts and it would introduce competition. If doctors felt that their patients were not getting the service from one trust, they could go and commission from another trust.
290. I agree with you in one sense. You said that the Minister gave a commitment that local councillors would make up over half of the LCGs, but that is certainly not what he said to the Committee.
291. Mr Matthews: The Minister did not give a commitment, but there did not seem to be any area of disagreement. That is something that we aspire to.
292. Ms Moorhead: He has given a commitment to more democratisation. This is our view.
293. Dr Deeny: I am currently on the West Local Commissioning Group — although I know that those groups are changing. There are 16 members, and four of those are local councillors and four are GPs. It is quite right that that should be geographically correct in each of the areas.
294. The regional health and social care board in Belfast is to have 400 staff, yet we have only 16 in each of the five local commissioning groups. There is no need for those 400 people in Belfast; I would have no problem with taking away half of those 400 and bringing the local commissioning groups up to 20 or 22 members. Then we could certainly have 50% councillors.
295. We are talking about commissioning going out to the local communities — bottom-up from the patient. You said that the health sector has always been in the hands of the professionals but believe me it has not. I know that you did not mean it like that. Commissioning was in the hands of the health boards, many members of which were managers or administrators and did not have qualifications in health. Many of those board members did not know the local communities, nor did the communities know them; commissioning was done in a top-down way. This whole idea of local commissioning is bottom-up.
296. There are a lot of councillors in my area who are committed to health, but I am told that on some councils there are not as many. There are reasons why many councillors in our area are involved in health, and it is a good thing. There are other people who are involved in their communities — for example, GPs such as me, pharmacists and optometrists. With the current proposal of 16 members, there is a danger of having no dentist, or no lay members, or not enough GPs. All of the people who I work with are committed to their local areas. As with elected councillors, there are people in health and the allied professions, and lay members — optometrists, dentists, people in childcare — who are very committed to their own areas and look at it in that way.
297. Is that the future? Do you think that eventually we should be coterminous with the councils — if we have 11 — rather than the trusts? There are still hundreds of people in the Department of Health, never mind the 400 people working for the regional commissioning board; that is bureaucracy dominating when we do not have enough commissioners in the community. If LCGs had 22 members, then I would accept your view that 10 of those should be councillors — there needs to be enough room for everybody who is interested.
298. Mr Matthews: We have our own house to look at; one of the big items in the review of public administration is the reduction in the number of councillors and the necessary change that will come when a lot of those councillors do not stand at the next elections. Capacity-building was one of the things writ large in that review. It is in all our interests to up the game and raise the standard of people who are aspiring to get involved in local and central government.
299. Capacity-building in local government is one of our big targets, but we have to change that culture. Currently, we have a few oul fellas going to a meeting of an evening to have a wee bit of an argument with their mates across the table — it cannot be that way in the future. I look forward to more professional people sitting on boards, bringing intelligent and rational comment to the various outside bodies. I look forward to the whole change that we are committed to, and to being able to sell that to the public.
300. Ms Moorhead: The rationale among elected members is that the health sector is run too much by professionals. The concern is that one or two elected members cannot make that much of a difference on those boards, as they would be overridden all the time by the professionals. The main point that we are making is that it is important to have public representatives — not just professionals — giving a public view of what people think is important; that is the ethos of what we are trying to say.
301. Ms Wylie: Our view is that commissioning should be as local as possible. We want coterminosity. Something similar to what you have described would be a best fit with local government, and we would support that.
302. Dr Deeny: What do you think of this situation? All of us, even local GPs, are accountable. The patients know who we are, as does the electorate. What you are proposing is a different model. Previously, no one knew who was on the health boards. The boards could commission and make decisions and people did not know who to go to if they had grievances. Now the plan is that everything will be locally controlled, and that is the good thing. However, to me, having 400 people in Belfast overseeing what the rest of Northern Ireland is doing makes a mockery of the whole situation. The Committee needs to know how many staff each of those bodies will have.
303. The Deputy Chairperson: The point about capacity-building for councillors is a key one. I sat on the RPA capacity-building subgroup, and the issue of the needs of councillors has been strongly highlighted by that subgroup.
304. There is also the issue of confidence. The general public need to have the confidence that the councillors representing them on the various bodies are capable, and that they are attending the meetings of those bodies.
305. Ms Moorhead: That is why we make the point about support. We currently have elected members on European monitoring committees, and the papers that they receive can be quite voluminous. If those councillors are carrying out five or six other jobs, that amount of paperwork is not manageable.
306. To assist with that, we received funding to appoint a European officer. That officer analyses the papers, prepares the briefings, sits with the members and agrees the key points that local government wants to make, and reports back. While we want elected members to be on the bodies, we also want appropriate arrangements. It would be inappropriate to ask public representatives to do a professional’s job. However, we do not want to undermine individual members. Often it is not the members’ fault, but the fault of the system. We have found that our members are much more confident and better briefed, and can report back and articulate their views so long as they get appropriate support.
307. Mrs Hanna: It is important that you are here today to express the views of local government. Many of us have a background in local government. Local government must be closer to the ground and the people if health inequalities are to be tackled and if people are to be supported in changing their lifestyles. There should be so much more going on in local government, particularly through the leisure centres and parks that we already have. If more is to be taken on — in a broader health sense — much will depend on how meaningful a role local government has within these bodies.
308. You talked about having sufficient numbers of elected representatives on the different bodies. That, I feel, must be balanced by the inclusion of other people and the community. A lot of it has to do with the role that councillors have. They must have something to contribute, not be sent there as a nodding dog with a large volume of paper that no one has time to get through.
309. The way that committees are set up in local councils can also make a difference. It is not just the chairperson who needs the briefings. We find in our own Committees that everyone needs to be kept informed of what is going on. That may mean cutting a great deal of less relevant matters from committee business, but that creates time for councillors to feel more confident and informed if they are attending meetings elsewhere.
310. We are in the midst of very exciting times, as the Committee has discussed with the Institute of Public Health in Ireland. Particularly in the case of the public health agency, where the more meaningful role is, how much contact have you had with the Department as to how meaningful the role of NILGA will be? Will it be a formal role rather than a consultative or box-ticking position?
311. It is important that NILGA should have a tangible role to play. It would be worth having some sort of pilot to help build capacity and see if it works. This is all about making things better for people, and it is only worth doing it if it will achieve that.
312. There has been disappointment in local councils with the responses given by some of the Departments during the review of public administration. It was not intentional, but meaning can get lost in the way that things are written. It is most important that there be a partnership between local government and everything else that goes on.
313. We have a big piece of work to do to tease out exactly what these bodies are going to do, and to make sure that they work together. The healthcare body must work with the public health agency; otherwise, it will not work at all. These bodies are so huge, as Kieran Deeny said. Decentralisation and moving services to other parts of the country have been mentioned, but we still have huge bodies in Belfast. The Committee must work with the Department to consider what the functions of those two big bodies will be. If this is to work, there must be a formal relationship between those bodies and local government and the communities. That is the bottom line for me, and I suspect that it is the bottom line for everyone. The proof of the pudding will be in the eating, but we cannot wait until it is all eaten. We must get it as right as possible before it gets off the ground.
314. Mr Matthews: It is our health and our community, not the bureaucrats’.
315. Mrs Hanna: I do not know how much contact you have had with the Department on what your role will be and how formal that role will be. It must be a meaningful role.
316. Ms Wylie: We have had quite a bit of contact with the Department, both officially and through some of the stakeholder engagement exercises that were carried out around the consultation document, which were all without prejudice. Belfast City Council has had contact with the Minister and the Chief Medical Officer. The chief environmental health officers group and NILGA have also had those contacts. We have worked closely together in local government so that we are giving one message about how the reforms could work and how the relationships should be formalised at a local level.
317. Ms Moorhead: I have been impressed. The Department has been open and engaging in wanting to have genuine talks. In such situations, a stand-off can develop as people seek to keep what they have. The Department has been open to the view that something closer is needed.
318. Mrs McGill: You made the point that Strabane and Belfast have different requirements. Carmel Hanna and Kieran Deeny mentioned inequalities, and that issue must be addressed. Inequalities can only be addressed at a local level — I support that position entirely.
319. I agree with the Deputy Chairperson and Mr Matthews about capacity-building; that is critical at this stage. However, your description of councils is not a reflection of what happens at Strabane District Council.
320. Ms Moorhead: I have one further point. The commissioning groups will be located locally. Local government is exploring options for subregional structures. For example, planning services will be with local government. NILGA’s prerequisite will always be to empower the statutory bodies, which will be the 11 councils. We want the councils to have as much of the services and to be as autonomous and locally accountable as possible. We suspect that, when we examine the services, some areas of work will need to be delivered on a shared basis. There are perhaps three or four areas in Northern Ireland that do not have technical services and planning. We would welcome a discussion on that, because we do not want separate health and planning subregional structures.
321. As you suggested, a shared service might allow the local commissioning groups to serve two councils. In the short term, a relationship with the regional public health agency might work on a two-for-one basis for community planning, and that might also work for planning and other arrangements in a group or other shared service, or in some other way that provides for the council something that could not be done across 11 councils. Our prerequisite will be to have as many services in the 11 councils as possible.
322. The Deputy Chairperson: Thank you.
3 July 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mr Thomas Buchanan
Mr Alex Easton
Mrs Carmel Hanna
Mr John McCallister
Ms Sue Ramsey
Witnesses:
|
Mr Paul McBrearty |
Mental Health Commission |
323. The Chairperson (Mrs I Robinson): I welcome Mr Paul McBrearty, chief executive, Mr Noel McKenna, chairperson, Ms Clare Quigley, social-work member, and Dr Brian Fleming, consultant psychiatrist and medical member, from the Mental Health Commission. I apologise that the Committee had to deal with other business before the evidence session could begin. I invite you to make a brief presentation, after which members will ask questions. When you have finished your presentation, I will allow up to one hour for the question-and-answer session. You are very welcome.
324. Mr Noel McKenna (Mental Health Commission): As chairperson of the Mental Health Commission, I thank the Committee for receiving us. Paul McBrearty will deliver the substantive presentation. I want simply to record our thanks to the Committee before he starts. Clare, Brian and I — and, indeed, Paul — will answer any questions that arise from the presentation.
325. Mr Paul McBrearty (Mental Health Commission): Thank you, Madam Chairperson. I understand that members have possession of our briefing paper. We will deal substantially with most of its points.
326. The Mental Health Commission is an independent, non-departmental public body — probably the smallest in Northern Ireland. Our budget is in the region of £600,000. We are comprised of a chairman and 16 sessional commissioners, who carry out a range of activities. Although those activities have been listed in our briefing paper, it is important that I highlight what they are and what they mean for the commission.
327. Commission members are drawn from a range of professions: psychiatrists, psychologists, nurses, social workers and other individuals — lay members — who bring their expertise to our work. We create teams that are required to visit any individual who is detained in hospital under the Mental Health (Northern Ireland) Order 1986. We also visit any individual who has a mental-health problem and is being treated under the legislation. That leads us to people who have difficulties that are associated with learning disability. Multi-disciplinary teams visit individuals in hospital and community facilities to check on the services that are being provided and, specifically, to meet and talk to those people and their relatives about their experiences while they are receiving treatment from health and personal social services.
328. That is a very important starting point because that means that we focus on the individual. We do not focus on the generalities of the service, but how the service has been delivered to specific individuals, how they are dealing with it and the sorts of issues that emerge. Within the statutory requirements, we can bring to the Department, the health trusts and any other body — this Committee included — any important issues that have arisen from the findings of our visits and discussions with those individuals. For example, we have expressed concern to the Minister in the past about under-18s being admitted to adult wards in mental-health facilities, and we are tracking progress on that regularly. We also have issues about the unavailability of acute psychiatric admission beds. Again, the commission has raised that issue in the past.
329. If we feel that it is necessary, we can refer a particular case to the Mental Health Review Tribunal so that it can review it with regard to, for example, issues of detention or guardianship. Very specifically, the commission has the power to gain access to any facilities, and, if required, it can medically examine an individual in private, whether it be in a hospital or a community facility. We have access to their medical notes to assure ourselves that the treatment that they are receiving is appropriate to their illness and that it is required. Last week, two of our commissioners travelled to Enniskillen to visit a learning-disabled individual in his own home to check that the guardianship was appropriate to his circumstances, as an issue had been raised with the commission about whether it was appropriate. We had to assure ourselves that that arrangement was appropriate for this individual. Again, I must emphasis that we focus on the individual, not on general services, although those general services are important to us.
330. The commission will appoint doctors who, at the end of the Mental Health (Northern Ireland) Order 1986 assessment process, can detain an individual — that is the “part II” appointment, as we call it. We also appoint doctors under part IV of the Order, which enables a doctor to get a second opinion if a patient has to undergo, for example, electroconvulsive therapy (ECT).
331. We review all legal documentation in relation to any formal detention, which is a very important function. The removal of anyone’s liberty is an extremely serious issue. The commission has to ensure that trusts that apply the legislation do so correctly. Not only do we check that the legislation is being applied appropriately, but we consider whether the clinical reasons for the detention are appropriate. That is an important function of the commission.
332. If an individual has been detained for more than three months, we are required to see the drug-treatment plan for that individual, and I know that the Committee is interested in drug-treatment regimes. Our medical panel, which is made up of the medical members of the commission, will review each and every drug-treatment plan for that individual and assure itself that the treatment plan is appropriate to the patient’s needs. We will obviously appoint individuals to give second opinions.
333. On 23 June, the Minister announced that, as part of the Health and Social Care (Reform) Bill, he intended to transfer the Mental Health Order functions from the commission to the Regulation and Quality Improvement Authority (RQIA). The commission welcomed the opportunity to make its views on that proposal known in the consultation process. In essence, the commission believes that it should be retained and its members made a submission to the Minister to indicate why it believes that that should happen. The commission felt that the fact that it is an independent body is important — that is especially important for those who access mental-health and learning-disability services. As we are a stand-alone body that is separate from the health and social services bodies, we are able to question the care and treatment that is being provided. We have indicated that we believe that that facility will be lost with the transfer of functions to RQIA because those functions will be only a small part of that overall body’s work. We are concerned about that, and I will address that issue in more detail shortly.
334. People with learning disabilities and mental-health needs are vulnerable and require an element of independence. As I said, we focus on the individual. The body that will take responsibility for that field is, in the main, focused on measurable standards, such as the regulation of various organisations and quality improvement. Although that is an important issue, the focus is different from that of the commission — we focus on the individual, rather than the wider body.
335. As I said, the commission is made up of professionals and lay members, which has been very important. The lay members challenge the professionals, and many have experience as either a service user or a carer for someone with mental-health requirements or a learning disability. That challenge is an important element of the discussion in the commission and is important to the way in which we carry out our visits. We are concerned that that level of service and client-user involvement would be lost if the commissions functions were transferred.
336. In recognition of the Minister’s indication that there will be a transfer of functions, the commission considered how to respond. We said that if our functions transfer to the RQIA, we would prefer a stand-alone unit in the RQIA to maintain the pseudo independence of the commission and to ensure that the mental-health and learning-disability element of the Mental Health Order is visible to anyone who wants to access our services. Part of our argument against the transfer is that the title “RQIA” does not reflect any aspect of the Mental Health (Northern Ireland) Order 1986. In contrast, the title “Mental Health Commission” conveys a clear message — if someone is unsure about who to contact for help, he or she will find the Mental Health Commission in the phone book or on the Internet and, if we cannot help that person, we will send him or her to the correct organisation. That is an important element that should not be lost if there is a transfer of functions. We are not sure whether a stand-alone unit can be established under the RQIA’s constitution, but we want it to be considered.
337. The functions of the commission include visiting patients and scrutinising legal documentation. Another important element of our work is the examination of serious incidents by the commission’s multi-disciplinary teams — those teams that are notified of any serious incidents that happen to people involved with mental-health services. Such incidents include suicide, other serious self-harm and violent incidents in hospitals or in the community, such as abuse from staff — which, sadly, sometimes happens — or abuse from another patient. The commission is notified of all serious incidents and intensely scrutinises the issues that arise from them. We talk to the trusts about their responses after their investigations and refer any issues that arise to our visiting panel so that, when they visit the facilities in question, they can ask what has been done to address the problems. We document the issues that are raised and how they are addressed.
338. Lay involvement is not as significant in RQIA’s format as it should be. Also, some of the professional representation for the Mental Health Order is not what it should be. Those are issues of concern, and we raise them as such with the Committee.
339. The commission made several recommendations to the Minister in the event of the functions being transferred, which is why we have come to give evidence to the Committee. Certain actions will reassure the commission about the future delivery of the Mental Health Order functions and that the interests of the vulnerable groups that I have mentioned — those who have a mental illness or a learning disability — will be protected.
340. Therefore, we made a number of suggestions. Firstly, the commission has a small budget, which it believes should be given to RQIA in its entirety. Given that that funding is a small proportion of the overall budget of RQIA, the commission feels that it should be protected for a period of years, enabling the functions to become embedded in the organisation. If efficiencies are produced as a result of economies of scale, the commission wants those additional moneys reinvested in the operations of the Order. That would allow the development of, for example, links with user-care organisations, enabling RQIA to become more familiar with the general public. The commission wants the Committee to be particularly aware of that issue.
341. The commission has suggested that the RQIA organisation should have full-time staff. That departs from the commission’s current practice of part-time sessional commissioners, but there was always an aspiration to bring in full-time professionals at some point. The commission believes that that approach is essential in delivering the function and in ensuring that it is delivered in a proper manner.
342. I have already referenced the name and logo of the RQIA. However, the commission would again ask that consideration is given to the inclusion of a reference to the Mental Health Order somewhere within that name or logo. It is not about the commission, but the Order, and it is important that it is reflected in some way so that users of the service and carers can find their way to that particular service.
343. The commission also suggests that the board of the RQIA should reflect the functions that it delivers, particularly in relation to the Mental Health (Northern Ireland) Order 1986. The commission may be being a little cheeky in that respect, but we have raised and discussed that with RQIA, and I know that it is giving it due consideration. It is fundamental that whoever is involved in the strategic direction-setting of the organisation running the Mental Health Order, has knowledge of the Order, mental-health and disability services. Furthermore, the commission feels that there should be someone with that knowledge at a very senior level in the new organisation. The commission has suggested appointing a new deputy or vice-chairperson, but that would be very aspirational in relation to what it wants to see.
344. As referenced at point 4?7, the commission is working with RQIA on a model of delivery. If a clearly identifiable and visual stand-alone unit cannot be created, the commission will work closely with RQIA between now and March 2009 to develop that model. That will satisfy the commission that delivery through RQIA will be appropriate to our beliefs and ethos, with respect to focusing on the individual. It is fundamental that a clear model of delivery is determined prior to the transfer.
345. It is also important that service users and the client groups are made fully aware of RQIA. The commission feels that that is important and that it should be actioned through the external-relations function. Preferably, there should be user or carer representation at a significant level within the RQIA organisation to represent mental-health and any disability functions.
346. The Chairperson: Thank you, Paul, for that interesting presentation. I would also like to congratulate you all for the sterling work that you have done up to now. I hope that the Minister will listen to those calls for the commission to have representation on RQIA, so that that sterling work does not get lost in the ether.
347. Mr Easton: I am a great believer that if something is working, it should remain the way that it is. In my opinion, the commission does not need fixed or changed.
348. Has the commission had direct meetings with the Minister about RQIA and is the Minister sympathetic to the commission? Furthermore, what can the Committee do to influence the Minister in the right direction?
349. Finally, how many people in Northern Ireland are held under the Mental Health Order?
350. Mr McKenna: I will answer some of those questions, and, perhaps, Paul will provide the statistical information. The commission did not have a personal, direct engagement with the Minister, but during a consultation meeting in a local hotel, I, along with Paul and some other colleagues, did have an opportunity to make a verbal representation to him, which we followed up with a substantive letter. He was well-disposed to listening to what we had to say. He told us that the purpose of transferring the functions of the commission to RQIA was to strengthen the work that will be done on mental-health and learning-disability services. If that materialises, I would be truly delighted.
351. I accept that there were deficiencies in the commission. Given its size, being a small organisation, the commission is vulnerable when it loses one or two key members of staff. There are certain benefits in economies of scale and a larger resource. If money was not a major factor, I could prescribe exactly what is needed for an independent commission. However, we live in the real world and acknowledge that money is a factor. We in the commission would be very concerned if the budget allocation for mental-health and learning-disability services was cut, and there were moves to economise, because those affected by such issues are a vulnerable section of the community.
352. I have a son with Asperger’s syndrome, and, when I meet psychiatrists and mental-health professionals, they tell me that they do not have the resources to do much for him. I will stay at the Committee meeting after this session to hear Lord Maginnis’s presentation on autism.
353. The commission would love to continue to carry out its functions, but we are not reactionary; if the democratic decision is to transfer those functions to RQIA, we are merely keen to ensure that the baby is not thrown out with the bath water. The challenge is there for RQIA, and we will do our level best to ensure that, when the functions of the commission are transferred, RQIA will deliver those functions in a competent and, indeed, an enhanced manner. We are confident that that will be the case
354. Had the commission remained in being, there were plans to appoint two or three full-time commissioners; to create a more expansive role for users and carers; to establish strong external communication links; and to provide some mental-health education. Hopefully, those things can still be done when RQIA assumes control of the functions. I was reassured when you told me on Monday, Madam Chairperson, that, as a watchdog body, the Committee will be monitoring very closely what happens when the functions transfer.
355. We accept that the decision has been made, but welcome the fact that the Committee will be monitoring the transfer of functions very closely. If the Committee can use its good offices to influence the Minister and the Department, perhaps some of the recommendations that have been suggested — which I think are valid recommendations — can be implemented under the governance of RQIA. The transfer of functions is going to happen, whether I like it or not — we are democrats, and accept the decision of the Government. All we are keen to do — and this is our bottom line — is to ensure that a good service is provided to our stakeholders; primarily, users and carers.
356. The Chairperson: Thank you. Will you provide statistics on the number of people who have been sectioned under the Mental Health Order?
357. Dr Brian Fleming (Mental Health Commission): On average, around 1,500 people per annum are compulsorily admitted to hospital by their general practitioners, and usually an approved social worker or member of the family. That period of admission is for, in the first instance, a week, then two weeks, and, thereafter, they may be detained for treatment for up to six months. Of the 1,500 people admitted per year, just over half of those remain detained for treatment. In others words, half are regraded as voluntary admissions or they are discharged from hospital before they require that detention.
358. Ms Clare Quigley (Mental Health Commission): To clarify, the role of the Mental Health Commission is also to monitor the care and treatment of the great number of voluntary patients in hospitals, in the community and with learning disabilities. Primarily, the voluntary patients with whom we deal have mental-health problems, but others may have learning disabilities.
359. Mr McKenna: Clare made an important point to which I want to add. As more and more vulnerable people with learning disabilities or mental-health problems are being decanted out of hospitals and into the community, they will need a watchdog body to represent and speak up for them. At least when those patients were in hospital they were sure of a visit from the commission, when it was in existence. My son lives in the community, so I am involved in the care movement. Community groups, with which I am in contact, are crying out for a watchdog body to represent them.
360. I want the programme for mental-health and learning-disability services to offer more user and care representation, which can deliver improvements to the service
361. The Chairperson: Thank you for your input.
362. Ms Hanna: Thank you, Chairperson. Good afternoon. Thank you for your presentation; it was very good. I do not have a specific question, but I understand where you are coming from.
363. I share your concerns about the role of an independent watchdog following the transfer. It is important that an additional mental-health role is clearly defined; at times, it is inclined to be an add-on. The presence of user groups is essential. As the Chairperson said, we will continue to monitor what happens following the transfer, because it is vital that there continues to be a specific role for the inclusion of your recommendations.
364. Mr McKenna: Thank you.
365. Ms Quigley: In future, there may be an opportunity for that when the new mental-health legislation is considered. It may be that, in the course of your monitoring, you are not satisfied with the level of specific individual attention that can be paid to mental-health issues within the transferred functions. You may want to look for a body under the proposed future legislation. That is worth keeping in mind, because we, as a commission, will not be around to make that plea.
366. Mr McCallister: We are keen that the good work undertaken by the commission is not lost or swallowed up in RQIA and forgotten about. Will you develop your point about the external-relations function; do you see some of that feeding into this Committee? How is that function being progressed? Is it effective? Where must we direct our focus to ensure that that continues to work?
367. Everyone in the room agrees that we must do more for the groups that you identified and with which you have been working. They are some of the most vulnerable people in society, so we want to be rock solid that we do everything that we can. Will the external-relations function help to build on that by not only promoting your work in the community, but by assisting all elected office bearers to communicate any problems arising from your duties back to the Committee and Assembly?
368. Mr McBrearty: It is fair to say that the commission expects a much broader discussion to take place with a wide range of groups about the operation of the Mental Health (Northern Ireland) Order 1986.
369. The commission has a limited life-span. We have only nine months left in which to work closely with RQIA on those issues. I hope that two developments take place before 1 April 2009.
370. First, the Committee will be keeping a close watching brief on the application of the Mental Health (Northern Ireland) Order 1986. However, RQIA, with its own statutory responsibilities, will be in a position to address the Committee or make reports to it, through whatever mechanisms are in place.
371. Secondly, we want RQIA to become actively involved with voluntary organisations and other user and care organisations. Without fear of contradiction, I can state that we have a good relationship with RQIA. We work very closely with it in order to develop everything that we have flagged up.
372. We cannot make RQIA do what we want, but we can try to influence its approach — in the same manner that, through talking with members, we hope that the Committee will seek to exert its influence to secure reassurance on issues that it regards as important.
373. RQIA seeks to develop external communications and to actively involve users and carers as part of a total remit, not just in regard to areas such as mental health and learning disability. RQIA must address the Committee about its plans on those issues. However, I would be remiss if failed to state that we are working closely with RQIA in order to share what we do and how we do it.
374. RQIA may have a better way of doing things — we will be happy if that is the case — but we have told it to heed our concerns. We would like to walk away on 31 March 2009, content that we had shared all our functional knowledge, and that RQIA had satisfactory plans in place for delivering services. However, we will not know whether that is the case, because we will no longer exist. RQIA’s preparedness might not be formally assessed until a year later.
375. Mr McAllister: In light of the relationship that has grown up, are you hoping for as seamless a transfer of functions as possible from RQIA?
376. Mr McKenna: Absolutely, we are anxious to ensure that a good, smooth transfer takes place. That is our responsibility and that is what we are charged to do. We have a good working relationship. We do not agree on everything, but dialogue is about negotiating.
377. We are here to make representations to the Committee, Madam Chairperson, because we will be gone in fewer than nine months, whereas the Committee will still have influence and be able to continue to monitor developments.
378. On Monday, I was reassured by your undertaking, in a personal capacity, to meet with us again formally or — time permitting — informally, if we have concerns that things are not progressing as well as we would like them to. I am confident that progress will be made.
379. Madam Chairperson, the Committee’s support, if it were possible, would be a confidence boost that we could convey to the Department, with which we share a steering group. We are also represented on a project group with RQIA. Committee support will add weight to our recommendations and ensure that both groups pay serious attention to your views.
380. Finally — and our psychiatrist, Brian, is very keen on this issue: we must have a separate annual report on mental health and learning disabilities.
381. RQIA must have some form of mechanism to convey to the population of Northern Ireland exactly what is happening in the fields of mental health and learning disability. The incidence of mental-health illness is increasing, instead of decreasing. We must take every step that is possible to reassure our population that the Government are doing everything that they can through both good health education and services. The Bamford Review has been endorsed, and the Government’s response to it, which looks positive, is available.
382. I am grateful that the Committee has listened to us today. With its support, the minds of senior civil servants and the RQIA will be more concentrated, and they may take the view that the recommendations have a lot of validity. Although they may not necessarily agree with everything that has been said, they will try to thrash out the recommendations and see whether some consensus can be reached.
383. Mr Buchanan: I commend the work that the commission has carried out already. I share its concerns about the transfer and hope that, during the transfer, none of that good work will be lost. We must keep a close eye on matters and scrutinise events. We do not want mental-health services to take a step backwards; we want to keep it moving forward.
384. I am disappointed that the Minister refused to meet with the commission during the consultation period. He should have met with it and listened to the concerns that you are now expressing to the Committee. The Minister will want to streamline services to provide a more efficient, effective service. I note that in your presentation, you said that the commission is already providing such a service.
385. What financial savings does the commission envisage the transfer will make, while maintaining the current level of service and building on it? We cannot stand still; we must build on the services that are provided already. If the services are being streamlined to make them more efficient financially, what will the savings be?
386. Mr McBrearty: The question of how the RQIA was dealing with the situation was put to it in discussion with the commission a year ago. At that time, the RQIA — perhaps not having an understanding of the full remit of the functions being transferred to it — indicated that there could be savings of about £250,000 to £300,000 from the commission’s existing budget. That is a considerable sum. However, that took into account the fact that the commission has a secretariat, a building and offices that represent expenditure that would be subsumed in a much larger organisation. At that time, and as the RQIA was considering addressing the transfer of functions, that was probably a reasonable place to be initially. However, following from our more detailed discussions about what will be required, the RQIA has shifted considerably from that position. Although I am not in a position to give an exact figure, I think that the potential cash saving that would come about from a transfer of functions would be less than £100,000.
387. The Chairperson: I reassure the commission that, following today’s meeting, the Committee will be making general comments to the Minister. I also reassure you that we will be scrutinising any legislation on the matter at Committee Stage, and we will ensure that the points on which you have major concerns are addressed in that legislation. However, if, before decisions are made, there is disparity between that and what the Committee sees as the continuation of effective good mental-health services, it will be mindful to ask the commission to come back and highlight those issues.
388. We thank you for coming before the Committee and making your presentation. I endorse what you said. It is important that we hear the voice of the user and the carer in any set-up; they represent the coalface. It is also important that that mechanism for representation is afforded to the carer or the user. It has been an interesting session; thank you very much.
389. Mr McKenna: On behalf of my accompanying colleagues from the Mental Health Commission — and, indeed, all commission staff and members — I thank the Chairperson and Committee members for receiving us today.
390. The Chairperson: Thank you.
11 September 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Mr Alex Easton
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Mr Craig Allen |
Department of Health, Social Services and Public Safety |
391. The Chairperson (Mrs I Robinson): The Health and Social Care (Reform) Bill is an important piece of legislation that will greatly affect health provision across the board. Today marks the beginning of the Bill’s Committee Stage, and departmental officials are here to brief the Committee on its provisions. Over the next few weeks, we will hear evidence from interested groups before embarking on a clause-by-clause consideration of the Bill.
392. We are subject to a very tight timescale, and we must complete our report by 23 October 2008. I refer members to the separate red folder, which contains a copy of the Bill, a briefing paper from Assembly Research and Library Services and a copy of written submissions to the Committee’s consultation on the Bill, which took place over the summer. In total, 29 responses to the consultation were received. I remind members to bring their red folder to each meeting during Committee Stage.
393. I welcome Mr Bernard Mitchell, Mr Ivan McMaster and Mr Craig Allen from the modernisation directorate in the Department of Health, Social Services and Public Safety (DHSSPS). I invite the witnesses to outline to the Committee the background to the Bill and its general provisions. Members will then be able to ask questions. I will allow up to one hour for the evidence session.
394. Mr Bernard Mitchell (Department of Health, Social Services and Public Safety): On behalf of my colleagues, I am grateful for the opportunity to begin this process of engagement with the Committee in considering the Health and Social Care (Reform) Bill. I will start by thanking the Committee for its input to date to the legislation. I acknowledge the helpful comments that were made during the Bill’s Second Stage in the Assembly on 1 July 2008.
395. The Chairperson has highlighted the tight timescale, for which I am also grateful. We are working hard to try to deliver the proposed changes by the due date of 1 April 2009. It is important to do so from the point of view of all those staff who need certainty about their futures and about the way forward. We have a busy few months ahead of us in going through the detail of the Bill’s proposals. Several proposals are still under consideration and subject to final decision. I will cover those areas if Committee members have questions about them. We will, of course, be available to answer any questions during the Committee’s consideration of the Bill, and we will call on other officials if additional expertise is required.
396. We intend to give a short explanation of the Bill’s main provisions, based on the broad thrust of its proposals. We will then take questions. I will now hand over to my colleague Mr McMaster.
397. Mr Ivan McMaster (Department of Health, Social Services and Public Safety): I will quickly run through the broad provisions of the Health and Social Care (Reform) Bill, and how those provisions are set out. First, it is important to say something about the Bill’s general content, and, perhaps more importantly, what it does not contain. The Bill’s purpose is to provide a legislative framework within which the proposed new healthcare structures can operate. The Bill’s aim is to set out, as transparently as possible, the high-level functions of DHSSPS and the various health and social care bodies that will be created under the legislation.
398. The Bill seeks, either in the body of the document itself or by securing the powers to make subordinate legislation, to establish parameters within which each of those health and social care bodies will be permitted to operate; what is expected of them; and the necessary governance and accountability arrangements that would support the effective delivery of health and social care in Northern Ireland.
399. It is probably just as important to note that certain measures are not included in the Bill. It does not rewrite Northern Ireland’s entire body of health legislation. Functions that existing health bodies carry out will still need to be performed. The Bill will legislate that functions once performed by A will instead be performed by B.
400. Pieces of legislation that bestow a vast number of functions, such as the Children (Northern Ireland) Order 1995 or the Mental Health (Northern Ireland) Order 1986, are extant, and the Bill will not seek to replace them. Rather, the Bill puts in place a framework of new structures. It will amend existing legislation only where it is absolutely necessary. For instance, pieces of legislation that were used to establish bodies that the Bill now seeks to dissolve must be repealed. In general, however, the Bill is to be read with, rather than instead of, other legislation.
401. The Bill does not address a number of issues. No mention is made of organisations such as the Northern Ireland Medical and Dental Training Agency (NIMDTA) or the Northern Ireland Practice and Education Council for Nursing and Midwifery (NIPEC). Bodies not mentioned in the Bill will continue to exist in their present form.
402. The Bill has 35 clauses, which come under 10 broad headings. I will cover those as quickly as possible. The fairly explanatory heading, “Restructuring of administration of health and social care” covers clause 1, which defines health and social care bodies. It is at the beginning of the Bill, along with explanations of abbreviations and acronyms that appear throughout, to facilitate the reader.
403. Clauses 2 to 6 deal with the “Department’s role in promoting and providing health and social care”. The clauses explain the Department’s general duties, powers and priorities. It is important to bear in mind that the Department will maintain all its existing duties. Those provisions broadly replicate the Health and Personal Social Services (Northern Ireland) Order 1972 by establishing the Department’s overall duty for health and social care in Northern Ireland.
404. However, the clauses, by providing an explanation of the Department’s duties, go one stage further than the 1972 Order did. The 1972 Order outlines the Department’s overarching duties to improve the health and social well-being of the people in Northern Ireland, whereas the Health and Social Care (Reform) Bill explains, in more depth, related issues, such as introducing policies and holding people to account. Clauses 2 to 6 set out clearly what the Department should and should not do, thereby allowing people to hold the Department to account if a duty is not performed properly.
405. Clause 5 introduces the new concept of the framework document. It sets out how the new bodies will be accountable in the discharge of their functions; how they must conduct their relationships with the Department; and, as equally important, how they will conduct their relationships with the other organisations to create an effective joined-up approach.
406. The introduction of the framework document is recognition that total clarity is needed about the roles and functions — local and regional — across all health and social care organisations, and of the Department.
407. The next broad heading, which covers five clauses from 7 to 11, deals with the establishment of the regional health and social care board, including its functions and objectives, and makes provision for the establishment of local commissioning groups (LCGs).
408. The existing four boards will be replaced by a single regional health and social care board. The regional board will focus on the main areas of commissioning health and social care; managing and improving the performance of health and social care trusts; and resource management. The legislation will give the regional board the power to offer guidance and direction to health and social care trusts, as well as to place a responsibility on them to abide by the regulations and to provide information as the board requires.
409. The reform will seek to ensure co-ordinated commissioning at all levels. The clauses will require the regional board to draw up a regional commissioning plan, and to consult with and to have due regard to advice or information that the proposed new regional agency for public health and social well-being (RAPHSW) provides.
410. Clause 9 deals with the establishment of local commissioning groups. The legislation allows the regional board to establish whatever committees it likes, but it specifically states that it must establish particular committees called local commissioning groups. Those groups will involve local health and social care professionals, local government and lay representatives. They will bring together their innovation and expertise and deal with local communities’ needs in the planning of services.
411. The number of local commissioning groups and the areas that they will cover will be specified in subordinate legislation. The current thinking is that there will be five groups, which will be coterminous with the five trusts. Those details will be covered by subordinate legislation because the issue may be re-examined when the local government boundaries are finalised. Therefore, it is slightly easier to deal with the matter through subordinate legislation than through primary legislation.
412. The membership of the LCGs will also be prescribed by subordinate legislation, which allows for more flexibility should any changes need to be made. The current thinking is that each group will comprise four GPs, a pharmacist, a dentist, four elected local representatives, two social-care professionals, one nurse, one public-health-medicine professional, one allied health professional and two health-and-social-care-related voluntary-sector representatives. If my maths is right, that is a total of 17.
413. The Bill requires the commissioning groups, in exercising their functions, to consult the proposed regional agency and to have due regard to any information that the agency provides. Again, that is an attempt to encourage joined-up thinking.
414. The next heading deals with clauses 12 and 13, which simply establish the regional agency for public health and social well-being. The creation of the agency stems from a desire to bring a higher profile to public health and social well-being and, equally importantly, to reduce health inequalities. The thinking is that a dedicated body is the best way in which to create a sustained and enhanced focus on the matter and to drive the public-health agenda forward in a manner that is not possible under current arrangements.
415. The new agency will have three key functions: health improvement; health protection; and the provision of public-health support to commissioning and policy development. It also has a particular responsibility for promoting improved partnership-working with local government and other public-sector organisations. Indeed, the clauses will place an obligation on the new agency to co-operate with other bodies that carry out health-protection or health-improvement functions. Again, we are aiming at some kind of joined-up work.
416. Clauses 14 and 15 will create a regional support services organisation (RSSO). Believe me, over the next few weeks, members will become familiar with those terms and initialisms. If members are struggling with them, do not worry. We are still struggling with them as well, so bear with me. The organisation will incorporate the majority of services that the Central Services Agency currently provides, but it will offer a broader range of support functions for the entire health and social care service.
417. Those clauses will impose a specific duty on the organisation to ensure an economic, efficient, effective service to all users. It will be required to operate within clearly defined standards, with measurable performance indicators. Clause 15 places a duty on the RSSO to put in place arrangements to that end, and the Department must approve those arrangements beforehand.
418. Clauses 16 to 20 deal with a broad range of “Patient representation and public involvement”. The five clauses deal primarily with the establishment of the patient and client council. They also deal with enhancing patient choice; meeting the needs and expectations of patients, clients and carers; and ensuring that their views are heard and listened to at all stages in the planning and delivery of services. The patient and client council will replace the four existing health and social services councils. It will build on the excellent work that those councils have carried out in the past, and it will combine the strong local focus that the councils provided with a powerful regional voice — a voice that has been missing in the current set-up.
419. Although the patient and client council will have a clear regional focus, subordinate legislation will provide that it must have five committees at local level, and those committees will be coterminous with the five integrated trusts. Those satellite offices will provide the important local presence that the health and social services councils do currently, but they will feed local issues and perspectives into the formulation of wider regional aims through the patient and client council.
420. Clause 18 places a duty on the Department, the regional board, the regional agency, the trusts and special agencies to co-operate with the patient and client council in the discharge of its functions. That is a statutory duty. There is also a duty to consult with the patient and client council, to give such information to it as it requires and to have regard to advice that it provides. That gives the patient and client council a statutory footing that it may not have had before the legislation was drafted.
421. Clause 19 also requires those bodies to prepare a consultation scheme, which the Department must approve. In the past, such a requirement has been known as a statutory duty to engage. The consultation scheme places a duty on all health and social care bodies to show that they will make arrangements with patients, clients, the patient and client council, and carers to ensure that they are involved in, and consulted on, the planning and provision of care, the development of proposals for change and decisions that affect the provision of all aspects of health and social care.
422. Clause 20 states that the bodies are required to have regard to the comments given — they cannot ignore them. The bodies will have to prepare a written statement that summarises the comments, and set out a response to those comments.
423. The next heading, “HSC trusts”, comprises clause 21, which deals with health and social care trusts. It places a duty on trusts to aim to improve health and social care, despite any competing priorities that they may have. The duty imposed in the clause already applies to the other organisations that we are creating in the Bill. However, for consistency, it was considered important that the provision be applied to trusts also, even though the legislation does not deal with trusts.
424. The next heading, “Public-private partnerships”, comprises clause 22 and deals with public-private partnerships (PPPs). Current provisions in legislation permit PPPs. The inclusion of that provision in the new structural arrangement clarifies that the Department, the regional board, the trusts, the regional agency, the regional support services organisation and special agencies are permitted to form, or participate in forming, partnerships to provide facilities or services. The inclusion of the clause is not about encouraging the use of PPPs, but it is acknowledged that private finance initiatives (PFIs) are only one of a range of procurement models and should only be used where it can be demonstrated that it represents better value for money as a conventional option over the lifetime of the contract. The clause permits, rather than encourages, their use.
425. The next heading, which deals with the “Transfer of assets, liabilities and functions”, covers clauses 23 to 28. The Bill becomes technical at this point. Clauses 24 to 26 deal with the dissolution of the health and social services boards, the Mental Health Commission and the Central Services Agency, plus the subsequent transfer of their assets, liabilities and functions. It does not seek to replace existing health legislation but merely states that functions that were previously performed in one place will now be carried out elsewhere. That is what the Bill does — it states that the responsibility for functions that were carried out previously by body A will be done by body B. Therefore, it does not interfere, detract from or add to those functions.
426. Clause 23 requires the Department to produce schemes for the transfer of assets and the liabilities of dissolved bodies, including staff who can be listed by name or by the type of work that they do. The staff have to get from body A to body B, and the technical provisions contained in clause 23 allow that to be done.
427. Clauses 29 to 35 become even more technical. They deal with the Department’s power to make supplementary, and other, provisions by amending or repealing legislation where necessary, and several are necessary. Although I said that we were leaving all legislation as it was — for the most part — some elements need to be amended or repealed, and those clauses deal with that.
428. There are seven schedules to the Bill, the final two of which set out in detail repeals and minor and consequential amendments. The first four schedules deal with the establishment of new bodies: the regional board; the regional agency; the regional support services organisation; and the patient and client council. Schedules 1 to 4 deal with details about the constitution and operation of those bodies; their committees and who shall serve on them; how their boards will be constituted; and how they will be established.
429. That is a very quick run-through of the Bill. I will leave copies of our submission with the Committee Clerk, as our submission may assist the Committee at a later stage in its scrutiny.
430. The Chairperson: May I ask a simple question? The consultation period ended on 12 May, and you received around 120 responses. Can you indicate what the general thrust of those responses is, percentage-wise?
431. Mr Mitchell: I may not be able to give a percentage breakdown, Chairperson; however, I can say, and the Minister will have said this in his announcement, that broad support was received for the thrust of the proposals. Having read through each and every page of all the received proposals, I can say that the quality of response was high and that the responses included some really good material. If you are interested, I will be happy to talk in detail at some point about changes to the proposals that have arisen as a direct result of the consultation responses.
432. A number of broad themes emerged from those responses; there was a great deal of support for the regional agency’s proposed role and for the renewed focus on public health and social well-being. There was a concern that the Bill be comprehensive and that it not be driven by a solely health-orientated agenda but that it take into account social well-being. That explains the name of the new agency in the Bill:
“The Regional Agency for Public Health and Social Well-being”.
433. It was chosen to try to get across the message that the agency will adopt a comprehensive approach to the public health and social well-being of the entire population.
434. There was much support for the new agency’s role, and for the establishment of a regional board to replace the four existing boards. The responses included a great deal of advice on how we might ensure a good relationship between the regional agency and the regional board; it was felt important that those two bodies operate seamlessly to a common agenda. It was suggested that the Department put arrangements in place to ensure that that is the case.
435. We received a limited amount of comment on the regional support services organisation. Responses that we did receive were broadly supportive, with the major theme being a concern that the RSSO be genuinely accountable to its customers to whom it will provide a service, especially those smaller agencies that will rely on it for support. It was felt important that those concerns and wishes be given due regard.
436. There was overwhelming support for our proposed patient and client council model, which is to have a regional council and five local committees. The notion of creating a strong regional voice with a good local presence that reflected local concerns and struck the correct regional/ local balance was also welcomed. That is an overview of the consultation responses, Chairperson.
437. The Chairperson: Thank you very much indeed, Bernard. I now ask Committee members to put any questions that they may have to our panel.
438. Mr Easton: In your consultation, did any groups highlight major concerns? Is there anything to be worried about?
439. Mr Mitchell: It was a good consultation so, as you would expect, two or three concerns were raised. As I have already said, the relationship between the regional board and the regional agency was raised. That is what I mean by a “good consultation”; many comments were insightful and came from people who had a good understanding of the importance of roles and relationships in an organisation. Therefore, the Department is paying a great deal of attention to that issue, and it is a key piece of work with which the Department is dealing and will continue to do so over the coming weeks.
440. Representatives from the voluntary and community sector expressed concern that that sector should play a proper role and be seen to have its place in the new system. The Department has sought to respond to that point in several ways. For example, the increased membership of the local commissioning groups — which now have two representatives from the voluntary and community sector — was a change to the original proposals that came about as a direct result of comments from the consultation. Another decision that was made as a result of the consultation was that the Department will seek to have an individual director with an allocated responsibility for the voluntary and community sector at executive level in the regional agency and the regional board so that there could be direct input into the work of both bodies.
441. A concern was raised that there should be more than one social care representative on the LCGs, so the Department has proposed that there should be two. That ties in with a related issue because notionally, at this stage, the Department has adult and children’s services in mind. Concern was also expressed that the broader agenda for revisiting arrangements for children’s services planning, and its multi-sectoral nature, should not be lost because of the new arrangements. The Department had several meetings with constituencies representing that side of the house and has agreed arrangements with them on how that part of the agenda will be developed.
442. I do not believe that any of those concerns would fall under the category of serious, below-the-waterline problems; they simply reflect a thorough response from the consultees.
443. Mr McMaster: Some concern was expressed that the regional agency for public health and social well-being might take away from the good work that is already being done on the ground. As a result of that, there was an original proposal that many health-protection and health-promotion personnel from the trusts would transfer to the new agency. Given those concerns, it has been decided that community-development and other health-improvement staff who currently work in trusts will not be affected in the shake-up. Therefore, the Department recognises that much good work is currently being done.
444. Mr Mitchell: When the proposals were initially announced, at a meeting that I attended with the Minister, members raised that point. A decision to bring a much-reduced number of staff into the regional agency was directly based on that concern and the subsequent consultation responses.
445. Mrs McGill: I joined the Committee only recently, and I have a question about the number of groups that have evolved because of the proposed changes. Is there confusion about that issue, or is there likely to be confusion? Given that you have said that the changes relate to the structure of care rather than the actual care that is being delivered, will you comment on the responses from those consultees? The Mental Health Commission responded and had some concerns about the lack of integration that might ensue as a result of the changes.
446. Mr Mitchell: I should have referred to the issue of the Mental Health Commission in answer to Mr Easton’s question. That concern was expressed, and it was considered carefully; several meetings were held with those concerned.
447. The view taken was that the functions of the Mental Health Commission could be undertaken more effectively within the broader infrastructure of, and with the greater resources held by, the Regulation and Quality Improvement Authority (RQIA). If the Committee plans to meet representatives from the RQIA, that would be an opportunity to seek some reassurance on that point. That was the rationale for the carefully considered decision to proceed with the transfer of the functions of the Mental Health Commission to the RQIA.
448. In the second reform phase, the number of bodies was significantly reduced. The first reform phase involved a significant reduction in the number of trusts, which now amounts to five trusts and the Northern Ireland Ambulance Service. The current phase will involve the amalgamation of the four health and social services boards into one regional health and social care board. The number of agencies affected was reduced from the original proposals, because it was felt that some of those agencies, such as the Northern Ireland Medical and Dental Training Agency, were doing good work. There was no reason to change the functions of that agency and other bodies because they were carrying out their functions effectively.
449. Mrs McGill: I declare an interest as a member of Strabane District Council. The Mental Health Commission submission states that councillors will be at arm’s length from commissioning decisions. Will that be the case?
450. Mr Mitchell: The view of the Department is that the functions currently undertaken by the Mental Health Commission will be fully addressed by the RQIA and that greater resources will be available to address those functions than is currently the case.
451. Mrs McGill: Is it only the elected councillors who will be at arm’s length from commissioning decisions? Will there still be local accountability?
452. Mr McMaster: The proposal is that there will be four councillors on the LCGs.
453. Mr Mitchell: There is provision for four local government representatives on each local commissioning group. There is also provision for local government representation on the patient and client council and in the regional agency for public health and social well-being. From the Minister’s perspective, the introduction of improved democratic accountability through active engagement with local government representation is an important element of the reforms. The current proposals are significantly strengthened in that regard compared with those that were previously being progressed under direct rule.
454. Mrs Hanna: Is it unusual for a Bill to contain provisions for the use of PPPs at this stage? I accept your view that that does not mean that such schemes will be used, but it seems strange to have that provision in the Bill, particularly as there is so much concern about PPPs. It seems as if the provision has been inserted so that, even if the use of PPPs is opposed, the option is still available to make use of them.
455. Mr Mitchell: The Department was conscious of that. The view was that legal clarity was needed in the event that it was decided to make use of a PPP scheme, and, if it were felt that the legal framework were not sufficiently clear, it would then be too late to address concerns from a contractor. The aim was to insert a provision into the Bill that was permissive but that made it explicit that the provision simply made the use of such a scheme possible, if it were required. As my colleague said earlier, it is not the Department’s intention to insert that provision with any motive to encourage PPP schemes. It is simply a permissive provision, and it provides the legal clarity that a PPP scheme can be used if it is required and is judged appropriate in individual cases.
456. Mrs Hanna: I am concerned that, if people are opposed to a PPP in any given case, it would be difficult to oppose it if the provision is already in the Bill.
457. Mr McMaster: The provision simply allows the use of PPP schemes, and it is not prescriptive about whether such schemes should be used; it simply permits their use. Timing is the issue; the provision for the use of PPPs does not sit altogether comfortably in the Bill. However, the Bill is probably the biggest structural change to health services since 1972, and the Department feels that the Bill is as good a place as any to insert a clarification that such a PPP scheme is available.
458. Mrs Hanna: It flags up the issue of PPPs, which people may not otherwise have thought about.
459. My other main concern is that powers are still centralised and do not flow down, despite all the discussions about personnel being in place to allow that to happen. The proof of the pudding may have to be in the eating; we will have to wait and see whether the powers are provided so that personnel will be able to make decisions and budgetary controls will be given to people nearer ground level. For many people, that has been a concern throughout the process.
460. Mr Mitchell: I want to comment on that, because several work streams are ongoing across a range of initiatives.
461. First, work is being undertaken on the proposed improved partnerships among health, social care, local government and other stakeholders. Those partnerships are at the heart of the proposals, and there are plans to run pilot schemes from April 2009. If that works and the pilot arrangements are put in place, that will be a real step forward in front-line, ground-level partnerships among the respective stakeholders who have an influence and interest in public health and social well-being.
462. Secondly, if LCGs and GPs feel that they do not have the required devolved authority, they will not participate and, therefore, will not function. Indeed, if Dr Deeny were here today, I feel that he would agree with that point. Effective commissioning is required, a sentiment that was expressed to me at a meeting this morning. I do not believe that the four local government representatives would be content to sit on a body if they felt that it did not have devolved authority.
463. Therefore, the Department is developing operating frameworks for the local commissioning groups. They begin with the premise that funds will be devolved to the LCGs through the governance arrangements of the regional board. However, that is done on the basis of empowering them to make decisions about local services. Many of the reforms rest on a number of factors, but that is one of the key foundation stones.
464. The Department is attempting to change the public’s perception of the scale of the LCGs, which is an issue that arose from the consultation process. Although LCGs are local, many people think that they will be large groups. The LCGs must think about how they will engage with local communities.
465. Mrs Hanna: Those are my thoughts. That is particularly the case with public health, where we want to reach the most vulnerable people. The LCGs must be linked in on the ground.
466. Mr Mitchell: Some of those people say that they are not represented by national bodies that represent the larger organisations. Therefore, the Department is introducing specific proposals for that type of stakeholder community engagement with the LCGs.
467. Mrs Hanna: By the same token, there is expertise beyond the Department on the current boards to make the decisions, particularly on public health issues.
468. Mr Mitchell: I recently met representatives from the Food Standards Agency, and they were enthusiastic about the potential role of that agency in focusing the agenda. That is what the Minister had in mind when he made the proposal.
469. The Chairperson: The Appleby Report identifies notable deficiencies in the Northern Ireland Health Service and also the distinct absence of an explicit performance management system. The report contends that the current performance management system is devoid of clear and effective structures, information and, most importantly, incentives — both rewards and sanctions — at individual, local and Northern Ireland organisational levels to encourage innovation and change.
470. Will you comment on that view and how it weighs up with the Bill’s proposals?
471. Mr Mitchell: That is an interesting aspect of the Department’s current work. It is akin to the blood flowing through the arteries rather than the bones of the structure.
472. Something similar to the current basic skeletal framework mechanism will remain, with the Programme for Government feeding down to a public service agreement, priorities for action, health and well-being plans, and trust development plans, with accountabilities at various levels.
473. There are real opportunities at present, because changes are being made that allow for a fresh examination of what is being done. The reduction in the number of boards, and the setting up of a regional board, provides an opportunity to consider greater consistency of information and for a more comprehensive and co-ordinated approach to the sort of management performance to which the Appleby Report aspired.
474. The very presence of the regional agency for public health and social well-being will allow a focus on the development of measures that can effectively gauge whether the progress in public health and social well-being that is expected as a result of the creation of the agency is being made. There are real opportunities. Colleagues with whom I met this morning are working on the detail of that performance regime, taking in all the relevant issues, including the regulatory framework, the role of the RQIA and the revised role of the slimmed-down Department, with an improved focus on how the regional agency and the regional board will work together and how the LCGs will play their part in that function and relate to the trusts.
475. The Department will provide a definitive framework for performance management. The reforms have given us the opportunity to do that. The Department is working hard on that matter, and proposals will be published in the next four to eight weeks.
476. Mr McMaster: The provisions of the Bill include a statutory responsibility for the regional board to performance manage the trusts. The board can now be told that that is no longer something that it should be doing but which it absolutely must be doing.
477. The Chairperson: I am glad that there will be that level of accountability and scrutiny. We are only at the start of the long process of considering the Bill in detail. Members have had to go through a lot of reading material. I thank the departmental officials for attending this afternoon; it has been very helpful. Thank you for your time.
18 September 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Mr Stephen Hodkinson |
Central Services Agency |
478. The Chairperson (Mrs I Robinson): I welcome Stephen Hodkinson, chief executive of the Central Services Agency, Jacqueline Kennedy, director of human resources and corporate services, and Paula Sheils, director of family practitioner services.
479. I invite you to make a brief presentation, after which I will invite questions from members. You are very welcome indeed.
480. Mr Stephen Hodkinson (Central Services Agency): Thank you very much for the invitation and the welcome. You have explained who we are so I will begin.
481. I intend to use our submission, which I have already sent to members, as the basis for the short presentation. I intend to give you some sense of the Central Services Agency’s work. At the end of the submission, we raise a number of issues, which are relatively minor on the scale of change taking place, but we thought it perhaps useful to draw your attention to those.
482. The Central Services Agency is a relatively long-standing Health Service organisation. It was established in October 1973 under the Health and Personal Social Services (Northern Ireland) Order 1972, and its main brief — as defined in the Order — is to provide a range of regional support services for the rest of the Health Service. The agency’s functions are wide-ranging and include legal services and procurement services, which covers sourcing, contracting, procurement and warehousing logistics.
483. The agency supplies support to family practitioner services, which I will describe in more detail, because the boards also provide such services. The Central Services Agency has a family practitioner services counter-fraud unit and an office of research ethics committees, which is less well known. The research and development office handles the budget for research and development in the Health Service, and the agency provides a range of financial services to support the Health Service and others. There is also a human resources department.
484. The agency currently provides approximately 90% to 95% of legal services to health and social services, which, in broad terms, is mainly for trusts. On 11 July 2008, as the Committee will be aware, the Minister took the decision to cease the use of private-sector providers. We are now working to bring all legal services to the Central Services Agency. That will ensure that all legal services in the Health Service are provided by the public sector. Our legal service is not profit-motivated; we aim to break even, and, furthermore, we provide services solely to the Health Service.
485. The submission shows the breakdown of the number of staff that our legal services employ, the size of the budget and the quality of service. There are usually 5,500 to 6,000 cases in operation simultaneously, which cover all areas of law including family law, child law, employment law, a wide range of medical negligence cases and cases that involve trips and falls. That workload will, probably, increase by between 500 and 1,000 cases when we adopt the work currently provided by the private sector.
486. The agency’s regional supplies service is one of two designated centres of procurement expertise in the Health Service, the second being health estates, which is part of the Department of Health, Social Services and Public Safety. That title indicates that we meet a wide range of standards in our areas of involvement.
487. The regional supplies service also provides services to the Department of Health, Social Services and Public Safety. It purchases a range of vaccines and various types of medicines for emergency situations for the Department. It has two warehouses in the Province in which those vaccines and medicines are stored.
488. There are issues about the possible future development of the procurement function. We currently play a small part in the procurement of services that are provided by nursing homes, residential homes and a range of domiciliary services. Those are currently contracted for by individual trusts, and we are working with a group made up from the Department and the trusts to find out whether some general, regionally applicable rules can be put in place so that the procurement process is consistent across the service and recognises the problems that the market faces in supplying the services.
489. The submission provides the Committee with an overview of the regional supplies service. Members will have gained a sense of its size; it has 300 staff and spends £307 million a year, which is a large amount of public money.
490. I will outline the role of the family practitioner services, although the fact that the director of that service has accompanied me to the meeting indicates that I am less well equipped to speak on that area. The service does not provide services to patients, but it provides a range of support services to the contracts that general medical practitioners, pharmaceutical practitioners, dentists and ophthalmic practitioners have with the boards.
491. We provide a range of payment services and support issues concerning the registration of patients, and our organisation issues medical cards. As a result of that process, we produce much information on the use of the services that we provide to the Department, the boards and the practitioners for planning and policy purposes and, to some extent, the monitoring of issues such as fraud.
492. Family practitioner services comprise a large part of the Central Service Agency’s business; we spend some £700 million a year on it, which is a large amount of money. We have some 180 staff, and the submission provides details of the numbers of practitioners who are contracted to the boards. My staff are in regular contact with those practitioners on various issues.
493. I have mentioned several issues that are on our agenda, and which have been for some years. The implementation of the electronic prescribing and eligibility system (EPES) is a particularly important issue. The Committee’s earlier business referred to its meeting with the Pharmaceutical Contractors Committee, and the Department and the Central Services Agency are in discussions with that committee on that issue. EPES is an important project for us.
494. There are other issues around the implementation of new contracts for certain practitioners, which automatically bring about a change in the way in which we operate, how we pay and how we staff. That is a large area of work.
495. The counter-fraud unit is, in some senses, linked to that, as it currently deals with family practitioner services issues. The unit pursues people who are suspected of having fraudulently claimed exemption from paying for their prescriptions and other charges. There is also a section that deals with contractor fraud, which, along with the boards, undertakes investigations when it is thought that fraudulent practice by practitioners may have taken place. Those are the two main areas of the counter-fraud unit’s work. We expect that the role of the counter-fraud unit will be extended to provide a service to the rest of the Health Service, including the hospital services, instead of simply concentrating on family practitioner services. That would involve a large piece of work.
496. The issue of free prescriptions has been the subject of some discussion over the years. That would be a significant issue for the Central Services Agency, because it would mean that it would not have to pursue people for non-payment of statutory prescription charges. That is an interesting area of work, to which we would respond if required.
497. The office of research ethics committees (OREC) manages health and social care’s research ethics approval process. In broad terms, applications to carry out research in the Health Service that may have ethical implications must go through the approval process. That is a statutory arrangement, and although the Central Services Agency houses OREC, appoints members of the committees and handles the process, it has very few powers as an organisation to change that arrangement, because it is part of a UK-wide process. OREC processed 230 applications for research work in 2007-08, which should give members an idea of the large volume of its work. OREC works exceptionally well, particularly in its close relationship with the trusts. The office is based at Haslem’s Lane in Lisburn.
498. I will now turn to the work of the agency’s research and development office. The Central Services Agency has managerial responsibility for a fund of some £13 million, which is allocated from the Department. That money is used to fund research across the Health Service. Although the present expectation is that all the agency’s services will be transferred to the new regional support services organisation (RSSO), to which reference is made in the Health and Social Care (Reform) Bill, a decision has still to be made about where the research and development office will go. All the other services that I have talked about will transfer to the regional support services organisation. We await that decision.
499. We have submitted two additional papers that deal with financial services and human resources services. Although it is reasonable to expect that an organisation of this size will have a finance department or a human resources department, the agency provides services to a range of other relatively small Health Service organisations and bodies, some of which are listed in our submission. The agency provides a payroll service, and it pays accounts for other customers. Our service model is an embryo of the shared services approach that is heralded by the regional support services organisation, which offers a wider service, including payroll, accounts and recruitment facilities across the Health Service. The staffing numbers are indicated in our submission.
500. Similarly, the agency provides human resources to a wide range of Health Service organisations and has been doing so for many years. Part of the human resources director’s brief is to look after equality services, to have responsibility for the implementation of section 75 of the Northern Ireland Act 1998 and to run the corporate services of the organisation such as building works and administrative processes.
501. The final page of our first submission provides the Committee with a few indicators that summarise the size of the organisation. The Central Services Agency currently has approximately 700 staff. Our operational budget is around £24 million, which is mostly spent on staff.
502. I have already referred to the large spend of the family practitioner services, while money spent on the regional supplies services is also rather significant. If taken together, those functions would account for around £1 billion of health and personal social services spend that the agency in some way handles. Furthermore, and for your information, I have indicated that we are not only based in Belfast city centre but have a range of offices — primarily for our procurement staff — across the Province. I have mentioned Haslem’s Lane in Lisburn already, but our headquarters, where the vast majority of our services is located, is in Franklin Street in the centre of Belfast.
503. That concludes my description of the agency. My general observation is that the services that health and social care provides are important and significant in the delivery of other services. Obviously, the agency’s activities mainly concentrate on services that are delivered to patients in hospitals and community-care settings. However, behind all that lies a fairly significant support arrangement that provides very important services such as procurement, payroll and legal services. We view the agency as an important part of the architecture of health and social care. We are very interested in the development of the regional support services organisation as a wider organisation that provides a wider range of services.
504. I raised four points in our second submission. They, in a sense, relate more directly to the
Health and Social Care (Reform) Bill. We, in our response to the consultation document on the Bill that the Minister issued earlier this year, indicated a support for the development of the RSSO. We believe that the establishment of the RSSO would represent a natural progression from the Central Services Agency, because it will provide a wider range of services than we currently provide. We have no fundamental concerns about the Bill or the creation of the RSSO.
505. It is very important to establish a wider organisation. Indeed, we have advocated that for some years. The creation of the RSSO will ensure that individual parts of the Health Service provide more functions regionally or centrally, and, for that reason, we support its creation.
506. I mentioned earlier that, as more services are placed together, the potential for producing a great deal of regional information begins to kick in. Therefore, we need to think of the RSSO not only as a provider of services but as a major provider of information.
507. My letter of 7 August 2008 to the Committee suggested that the new organisation not be named the RSSO. We feel that the new organisation’s name should be more reflective of the business and business-support functions that we currently provide, and “support services” does not reflect those. Although the RSSO will support the delivery of health and social care, it will also have a status of its own. For example, we currently have a number of professionals working for us who provide financial, human resources, legal and procurement support. We also employ other professionals, such as dentists and pharmacists. We wish to see the name changed to reflect that.
508. The Chairperson: Thank you, Stephen, for that detailed presentation. I will now open it up for Committee members to ask questions.
509. Mr Easton: First, what functions that will add to your workload will come from the boards and trusts to the new body? Secondly, how much savings do you think that you will be able to make? Thirdly, will there be any job losses among your 700 staff, or do you foresee that an increase in staff will become necessary as a result of more services being transferred from boards and trusts?
510. Mr Hodkinson: I expect the RSSO to provide more services than the Central Services Agency does at present. The Department’s superannuation branch, which runs the health and personal social services superannuation scheme — therefore, it is a scheme for the Health Service, not one for the Department — should transfer to the regional support services organisation. That is the current thinking. According to the timetable, that function will probably transfer on 1 April 2009, so that will happen in the relatively short term.
511. The four health boards perform some payment functions for GPs. Our expectation is that those functions will transfer to the RSSO to complete the package of payment services that we have. Our medium-term expectation is that ICT and IT services provided in the Department will transfer to the new organisation.
512. In the longer term — two to three years — subject to the investment that is necessary in ICT, we expect financial services such as payroll and “accounts payable”, which is the handling of all invoices, will transfer to the RSSO, and those services will be provided on a regional basis for all the trusts.
513. Human resources and recruitment is another area. At present, all Health Service organisations recruit for themselves, more or less. There are some arguments, and models, that indicate that some of those recruitment services could be provided regionally for other organisations.
514. Mr Easton: What about savings and job losses?
515. Mr Hodkinson: The expectation is that savings will be made once the RSSO is in its completed form. Several models of shared services exist across the public sector. Those can be found principally in the United States, Australia and the Far East, where organisations have adopted the shared-services approach. I must stress that, with proper investment in IT and its various support systems, one can make savings and produce a much more cost-effective way of working.
516. As I said, the agency currently has 700 staff, and it is planned that the RSSO will have anywhere between 2,000 and 2,500 staff. That represents a sea change. Central Services Agency services will not make savings in the first instance, but they could be made as we expand the support services that form part of the RSSO over the next two to three years.
517. We will remain part of the comprehensive spending review until 2011, and the whole of the support-services area must take its share of savings made.
518. The Chairperson: That was a very detailed response.
519. Dr Deeny: I welcome Jacqueline, Paula and Stephen. It is nice to see some of the faces behind the Central Services Agency, because, in my role as a GP, I have been in touch with the agency many times down the years. Of course, Stephen, I know your brother well, who works in Omagh as a consultant.
520. Ms S Ramsey: Do you need to declare an interest?
521. Dr Deeny: I do not. I want to be clear, because I have not looked at the legislation since before the summer recess. Three major agencies are to be established: the regional health and social care board; the regional agency for public health and social well-being; and the common services organisation. I assume that the Central Services Agency, which will be renamed the RSSO, and which you would prefer to see renamed, will lie within the common services organisation. Is that correct?
522. Mr Hodkinson: “Common services organisation” was the initial name chosen, before it was changed to “regional support services organisation”. We were even more unhappy with the former, because we did not like the use of the word “common”. We have progressed the issue to “regional support services organisation”, and the next stage, as we see it, should be to change the name again to “regional business services organisation”. However, yes, the agency’s services were originally to lie within the common services organisation.
523. Dr Deeny: What else, along with the Central Services Agency, will make up the RSSO?
524. Mr Hodkinson: The legislation indicates broad headings of areas in which the RSSO will provide services. However, the kind of work that we are trying to plan for the RSSO indicates that it will include: the Department’s superannuation branch; a large part of the services that the Department’s directorate of information systems currently provides; and some of the financial and human resources services that boards and trusts currently provide. There has also been discussion about moving information services and providing a range of estates services regionally for the entire service, but that is a longer-term objective. Some of the boards’ family practitioner services will also move to the RSSO.
525. Dr Deeny: I have some experience of what the agency does, and that includes much good work with GPs. Mr Hodkinson also mentioned that he would like to see other functions added to the agency’s current duties.
526. Finally, paragraph 4 of your letter states that the acronym RSSO:
“could have an unfortunate and clearly unanticipated sound”.
What is that sound?
527. Mr Hodkinson: I have been practising it, Chairperson, and I am not sure how to say it to the Committee.
528. The Chairperson: I have that problem all the time.
529. Mr Hodkinson: In my case, the problem is possibly down to my age. RSSO, if pronounced as one word — must I say it?
530. The Chairperson: Yes, please. I like to laugh at someone. [Laughter.]
531. Mr Hodkinson: It sounds like “arso”. [Laughter.] I thought that that might surprise the Committee.
532. Ms S Ramsey: It is as well that Jonathan Ross is not here.
533. Mr Hodkinson: People are generally mumbling the sound. I was hoping that members would rehearse it in their minds and that I would not have to say it. It is an unfortunate sound, even if it was not intentional.
534. The Chairperson: Once it gets out, the name will stick.
535. Mr Hodkinson: That is true. It must be dealt with at an early stage, and I am trying to do so with my departmental colleagues.
536. The Chairperson: It would be wise to change the name, because you would be the butt end of a joke. [Laughter.]
537. Mr Hodkinson: Thank you very much.
538. Dr Deeny: You mentioned the agency’s current functions. Are there other functions that you would like to take on?
539. Mr Hodkinson: I mentioned the research and development office, which is one of our functions. However, the Department has not as yet told us where that function will go. It may not go to the regional support services organisation but to one of the other two main bodies to which you referred.
540. Mrs Hanna: You may be aware that the before it became DEL, the Department for Employment and Learning was almost named DOLE — the Department of Learning and Employment. That had to be changed. [Laughter.] You may have to do the same.
541. What impact will the Minister’s decision to bring all legal services in-house have on the agency? You mentioned the fact that the agency plays a large role in information and communication services. How will it manage those functions?
542. Mr Hodkinson: The agency welcomes the Minister’s decision that the Central Services Agency should provide all legal services for the health and social services internally. We have argued for that for some time.
543. There will be big changes. First, costs will be saved. As I said earlier, we are not a profit-driven organisation — we charge to cover costs. That means that we build a relationship with our clients. We agree fees with them on hourly rates or block contracts. Our intention is only to recoup the funding that we need, fundamentally to pay our staff. That, in itself, takes us out of going rates in the market for legal services. That is an improvement.
544. There are other, perhaps less obvious, advantages. Under the arrangements that existed when there were several providers of legal services, it was possible that different advice was being given for the same problem in several places throughout Northern Ireland. For example, a social worker could ring for advice on a child case in Strabane, and another could ring in Newry, Larne or wherever, and they would all receive slightly different advice from different providers. There is potential for us to bring together such advice. We can, therefore, offer advice to someone in Belfast, and if that person’s query emerges as a frequently asked question, we can then inform the rest of our clients — the rest of the Health Service.
545. We provide a training regime for our professional and support staff, and also for clients, in how to handle matters themselves so that they do not always need to call their solicitors and create an administration process in order to solve a problem. Until now, we have not provided that training for some parts of the service whose legal services are provided by the private sector. Therefore, that will bring about consistency.
546. We have a system that I have always considered an expensive way in which to do things. If, for example, a medical-negligence case arises that involves three hospitals — say, a patient has gone to his or her local hospital, has been referred to another hospital, and then to a tertiary service in the Royal Victoria Hospital — and the three hospitals belong to trusts that have different legal-service providers, each of those legal-service providers may wish to engage an expert because they each represent a different client. That is expensive. That will not happen — certainly not to the same extent — if all legal services are provided from one source.
547. Therefore, there are several hidden advantages. However, there are several other matters on which we must begin to work more strategically across the entire service.
548. Mrs McGill: My question is on procurement, which Carmel touched on in a previous question. To date, what has been the agency’s relationship with the Central Procurement Directorate (CPD) here? What will it be in future?
549. Mr Hodkinson: We have a close relationship with the CPD at a professional, working level. Our colleagues in the regional supplies service work with the CPD. We consult the directorate on a one-to-one level for advice. We also work with the CPD on several groups that the Department of Finance and Personnel (DFP) has put together over the years to ensure that consistent approaches are taken to procurement across the public service. The best example, which I carry round in my head, is that we have vehicles, such as ambulances and trucks. We also have contracts for tyres and tubes. I apologise for reducing the matter to such a basic level. However, it illustrates the point that I am making.
550. Parts of the public service, such as education and library boards, use more vehicles than we do. Therefore, it makes sense that they should have the contract for tubes and tyres for the entire Province, and that we buy off that contract. Similarly, it makes sense that we should have the contract for laboratory equipment, and schools and universities can buy off our contract. We are developing relationships with the Central Procurement Directorate, the Water Service, the education and library boards, the Housing Executive, and so on, in an attempt to get the best return for the investment that has been made across the public service.
551. Mrs McGill: Did the Central Services Agency engage with CPD to provide legal services and advice on the difficulties and the Minister’s subsequent decision?
552. Mr Hodkinson: No, CPD secures its own legal advice, presumably from DFP legal services or Government legal services. The Central Services Agency has not advised CPD on legal matters. Indeed, that would have been a conflict of interest, as we would have been a potential competitor to other groups.
553. Mr Buchanan: I apologise for being late and missing part of your presentation. When I came into the meeting, you were answering a question that Alex Easton had asked. You stated that substantial investment in IT services is needed if savings are to be made. What level of investment package would IT services need in order for appropriate savings to be made?
554. Mr Hodkinson: Three projects are in need of investment. The first of those is family practitioner services, which I will ask Paula Sheils to talk about in a moment. The second is finance and supplies —procurement — and the third is payroll and human resources.
555. Our payment systems for paying bills are fairly antiquated. We have had them for some 10 to 15 years, and they are not fit for purpose for what we want them to do. Those payment systems pay the bills. However, the turnaround is not fast enough; they do not produce the necessary information; and they are not compatible with the supply services, which, because of the large number of suppliers that we have to pay within a certain timescale, are closely linked to paying bills.
556. It is generally accepted that investment is needed for new systems in finance and supplies and in payroll and human resources. Our payroll system is very old — information and communications people would call it a legacy system. The system pays people — we do not receive complaints on that front generally — but its sharing of information with human resources is antiquated. Human resources information is used in payroll calculations. An investment of around £12 million is needed in order to improve those systems.
557. Ms Paula Sheils (Central Services Agency): The payment systems that we use in family practitioner services pay general practitioners, dentists, optometrists and pharmacists. Like the systems that Stephen has just described, they were fit for purpose 20 years ago, but the nature of the contracts with the independent contractors has changed over time. The systems were originally built to cope with items of service claims — someone did one thing and was paid for doing that one thing. However, contracts are moving to the provision of a service with practice-based payments.
558. Many of our payments must be calculated offline before being entered into the payment system. We cannot calculate those payments on the system. Therefore, we must change the systems not only to ensure that they are sufficiently up to date to meet the demands of the current contracts but to ensure that they are flexible enough to be amended easily in order to adapt to future changes.
559. To make a change to the current systems is extremely expensive, because the programmes were written in an old language, the common business oriented language (COBOL), expertise in which is disappearing. People are no longer being trained to maintain that system. Therefore, we must change the system for family practitioner services payments. The system is fine for making payments, but we look forward to the day when any necessary changes can be made more cheaply.
560. Mr Gallagher: The agency seems to have approximately 700 staff employed in delivering services. The overall exercise is one of rationalisation, so how many people do you expect to employ after restructuring the organisation?
561. Mr Hodkinson: If the regional support services organisation were not being introduced, and we were implementing the computer systems that we need, we would be reducing staff numbers from 700. It is difficult to give an exact figure, but it would probably reduce to approximately 600.
562. If we transfer the 700 employees to an organisation that employs between 2,000 and 2,500 staff from other boards and trusts, there are potential savings to be made in areas such as payroll and finance, which are currently distributed around the system. Therefore, to bring them together in one or two places, or into one process, will produce savings. Overall, the Minister expects us to cut 1,700 administrative staff across the review of public administration, thereby saving £53 million. That £53 million is funding freed from support services and administrative services for release into direct patient and client-care services.
563. The Chairperson: Everyone who wanted to ask a question has done so. Thank you for that detailed and interesting presentation, Stephen, Jacqueline and Paula. We appreciate your coming today. Thank you for your time.
25 September 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Ms Claire McGill
Witnesses:
|
Mr Richard Dixon |
Eastern Health and Social Services Council |
564. The Chairperson (Mrs I Robinson): I welcome Richard Dixon, who is well known to the Committee as the chief officer of the Eastern Health and Social Services Council. I invite Richard to make a presentation, after which I will invite members to ask questions.
565. Mr Richard Dixon (Eastern Health and Social Services Council): I thank the Chairperson and members for inviting the health and social services councils to present their views on the Health and Social Care (Reform) Bill to the Committee. My presentation is based on the response to the four councils’ consultation, which is a consensus view reached by the councils after careful consideration of the proposals, particularly the proposed establishment of a patient and client council.
566. In general, the four councils are supportive of the proposals. We believe that the new structures will offer the people of Northern Ireland a much-improved system of accountability and involvement.
567. We welcome a structure that has a clear line of management responsibility from the Minister and the Department, through the commissioning board, and to the providing trusts. The accountability of trusts to the regional health and social care board is a key strength of the proposed structures. The previous arrangement, in which commissioners and providers were jointly accountable to the Department but in which providers were not clearly accountable to the commissioners, was not ideal. Customers want a simple transparent system in which they can see how, where and by whom decisions are made. The proposed new structures will deliver that.
568. Over many years, the health and social services councils have represented patients and the public within the health and social care system. Therefore, we welcome the priority that the legislation gives to engagement with patients and the public. We welcome the creation of the patient and client council. We also welcome the representative nature of the new bodies, particularly the local commissioning groups. Above all, we welcome the new duties in the legislation on engagement with patients and the public, which are applicable to all the health and social care organisations.
569. I will now comment on our response to the proposed creation of the regional health and social care board and the regional agency for public health and social well-being. Our concern for a simple, clear and accountable structure is reflected in the comments that we made in our response to the proposed creation of those two bodies. Although we strongly support the creation of local commissioning groups and the delegation to them of significant commissioning responsibilities, we wanted it to be clear that they operate under the direction of, and are fully accountable to, the regional health and social care board.
570. Underlying central authority will help to ensure equity in the allocation of resources and access to services, will guard against the risk of a postcode lottery in Northern Ireland and will ensure that regional, as well as local, interests are taken fully into account. A regional authority will benefit those in small and dispersed communities, such as those who live with a rare condition who may — and I emphasise “may” — fall below the radar of local commissioners and their priorities. For a similar reason, we said that the regional agency for public health and social well-being should be accountable to the regional board. We were concerned that a separation of the public-health functions in that manner would lead to silo thinking — a territoriality among organisations that could work against the best interests of patients and the public.
571. However, we are comforted by the Minister’s recognition of those concerns in his response to the consultation and by his commitment to the production of a framework document that makes abundantly clear the respective functions and interrelationship of the new health and social care organisations.
572. The proposals for the patient and client council are in line with the views expressed by all four health and social services councils throughout the planning process. We welcome the clarity of the proposed patient and client council’s functions, the place it will be given in the new structures, its independence and the duty placed on all health and social care organisations to engage with it, which is enshrined in the legislation.
573. The issue of most concern to members of health and social services councils in the development and delivery of the patient and client council is how local representation will be preserved and maintained. Regardless of how that is worked out in secondary legislation and in implementation, members of health and social services councils will want an organisation that is clearly rooted in local communities and which equitably hears the local voice. Notwithstanding that, the members of health and social services councils recognise the importance of having a single co-ordinated organisation to formulate and express diverse local views and, consequently, welcome the broad consensus of opinion, in response to the consultation, that the patient and client council should be a single body rather than five local and autonomous groupings.
574. In conclusion, the collective view of the health and social services councils is that they are able to support the structures that are set out because they are, in principle at least, capable of delivering fully accountable services and seeking the involvement of patients and the public in all their functions.
575. Dr Deeny: Thank you for the presentation, Richard. I have worked in the Health Service for many years and am very interested in this issue. Are you in favour of one patient and client council or one patient and client council that has five offices?
576. Mr Dixon: We are in favour of one patient and client council that has five local offices.
577. Dr Deeny: As with any consumer council, the patient and client council is a patients’ advocate. How many members will a patient and client council have? How much clout will it have to stand up for patients? I assume that the five offices will be in the confines of the five trusts; how many people will be employed in those five offices? As a GP, people visit me to discuss health issues. For example, someone rang me at lunchtime with a complaint. Should people who complain be directed to one of the five offices, which will then refer them to the patient and client council?
578. Mr Dixon: There are a number of issues there, and I will try to take them in turn. Matters relating to membership and structures are currently under debate and discussion.
579. We imagine that there will be a regional patient and client council, which will have a membership of at least 15 people. However, it will be difficult to balance the need for the council to be representative with the need for it to be a board of governors that looks after an independent organisation. The members of the four health and social services councils currently work on a voluntary basis. We have no executive functions, and we are looked after by the boards, hence I am called an officer rather than an executive. Nevertheless, we anticipate that the regional patient and client council may have a similar make-up, and there will be a genuine attempt to ensure that it is representative of local groups. We are unsure about the size and composition of the local groupings in each of the trusts and local commissioning groups areas, but we may be less constrained, provided we have the freedom to recruit people that the patient and client council regards as appropriate or representative of an area and provided a clear link is created between it and the regional body.
580. We imagine that regional body members will be paid. The local groups may remain voluntary, and that would provide more latitude, but there would have to be an absolute link between those local groups and the regional body.
581. We imagine that the patient and client council will have five offices that will deliver three core functions for their respective areas. Those functions are: advocacy for individuals with complaints; liaison; and working, and maintaining a relationship, with the local trust, the local commissioning group and other relevant bodies, including the voluntary and community sector. Furthermore, the offices will actively engage with communities. It is reflected in our response that representation will be contained within committee membership, but it is always augmented, whether by a local commissioning group or a patient and client council, by an active ongoing programme of engagement with communities. The officers will go out and meet people and bring back their views, as well as take in the views of members of local committees.
582. Access requires work, because, with the best will in the world, even with five local offices, they will not be accessible or local to everyone in that patch. We hope that serious consideration will be given to ideas such as accessible clinics for advocates, access to the Internet and to new technologies to a greater extent than was ever the case with the health and social services councils. You are correct to point out that access is of primary importance.
583. Lastly, the powers of the patient and client council are greatly augmented by the Bill. A duty is placed on all health and social care organisations to engage with the patient and client council and to listen to what it has to say and to have due regard for it. That is a significant additional power that gives the patient and client council influence to a greater extent than the health and social services councils now have.
584. The requirement that all health and social care organisations produce consultation and engagement strategies will address how they are communicating and working with the people whom we serve. Those strategies will be approved by the Department of Health, Social Services and Public Safety only after consultation with the patient and client council. Again, that is another significant additional power.
585. Mr Gallagher: Richard, you spoke about people working for the patient and client council, but most of its members will be unpaid. Is that correct? If so, it will be important for members who take time off work to receive appropriate remuneration, as they are making a valuable input into council discussions, formulation of plans, and so on.
586. In your submission, your response to clause 8(2) of the Health and Social Care (Reform) Bill is that the regional board’s functions do not include any reference to balance of regional, strategic commissioning and locally responsive commissioning.
587. It is important for that issue to receive a good deal of attention as the Bill progresses, because the public have many questions about disparity. People in the west, for example, ask why home helps there are paid at a different rate than in other areas and why, across all the trusts and boards, some areas provide vulnerable groups with more support than others. It has always been difficult to obtain accurate information about such variations, and figures must emerge to identify how much money has been allocated to different areas.
588. Is that what you were getting at? If so, have you any ideas about how to improve that situation, because the subject has been discussed in Committee and no answers have been forthcoming. How could more balanced commissioning be achieved?
589. Mr Dixon: The theme of the councils’ response was to make a clear statement on the need for central leadership and direction that will, and should, provide equity across Northern Ireland. In saying that, we do not wish to detract from the important local agenda that requires local responsiveness. We clearly stated our support for those structures that involve locally elected representatives, engage with communities and decide what people in the area need and want.
590. However, any proposals should arrive at a central point at which someone makes a decision. Among the duties of that individual should be to ensure equity of access, so that a person in Strabane will have the same experience of a service as a person in Newtownards. That is the business of decision-making; it is why a central authority is necessary, and it is the underlying theme of our response. Until now, such an authority has not existed.
591. We stated in our response that the fragmented nature of the planning and delivery of care through multiple organisations in the old system was a disadvantage and should not be replicated in the new structures.
592. Mrs McGill: Thank you, Richard, for mentioning Strabane; I am grateful to you for doing so. I want to put on record that I welcome that and the fact that equality of service, provision, and so forth, that has not existed thus far, will happen.
593. The Chairperson: That was a fairly simple and straightforward comment. Members have no further questions. Thank you, Richard, for taking the time to meet the Committee and for your presentation.
25 September 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Ms Claire McGill
Witnesses:
|
Mr Dominic Burke |
Western Health and Social Services Board |
|
|
Dr Paula Kilbane |
Eastern Health and Social Services Board |
|
|
Mrs Fionnuala McAndrew |
Southern Health and Social Services Board |
|
|
Mr Stuart MacDonnell |
Northern Health and Social Services Board |
594. The Chairperson (Mrs I Robinson): I welcome Dominic Burke, acting chief executive of the Western Health and Social Services Board; Paula Kilbane, chief executive of the Eastern Health and Social Services Board; Stuart MacDonnell, chief executive of the Northern Health and Social Services Board; and Fionnuala McAndrew, director of social services in the Southern Health and Social Services Board. You are all very welcome. I invite you to make a brief presentation, and I will then invite questions from members. I will allow around 40 minutes for the evidence session.
595. Dr Paula Kilbane (Eastern Health and Social Services Board): Thank you, Chairperson. I am the current chairperson of the chief executives’ group, so I will briefly outline some points in our submission, because the main purpose of our visit is to answer questions.
596. We welcome the underlying themes of the review of public administration (RPA), including the reduction of bureaucracy through simplifying systems and avoiding duplication. We particularly welcome public health and well-being’s significantly enhanced profile in the Health and Social Care (Reform) Bill, because, although we all recognise that it is very important to cure, and care for, those who are unwell, it would be better if we could prevent them from becoming unwell in the first instance.
597. It will be very challenging to deliver the reforms in the Bill. We are attempting to reap the benefits of reduced bureaucracy in the context of new organisational arrangements. There is a particular challenge in bringing together those different interfaces, particularly that between the regional health and social care board and the regional agency for public health and social well-being. The functions that the health and social services boards currently carry out will be transferred to one or other of those two bodies. Indeed, some will be transferred to a third body, the regional support services organisation (RSSO). The core functions of the regional health and social care board itself are: commissioning; performance management and improvement; and financial management. The regional board must have primacy in commissioning, taking account of, and paying due emphasis and regard to, input from the regional agency.
598. The range of commissioning activities and functions to be carried out should equate to what the health and social services boards are currently doing — those activities and functions should be both regional and local. The commissioning arrangements should deliver improved health and well-being, and reduce inequalities. That will depend on how efficiently the regional board interfaces with the regional agency. Importantly, the board will be a regional body with an intense local focus. The Bill contains a major and welcome emphasis on the views of service users, communities and the public, and, in particular, it provides for local representation from locally elected councillors.
599. The regional board will be multi-professional; that is absolutely essential when dealing with the complex range of services that will be commissioned. However, there will also be adequate provision in the commissioning arrangements for specialist and vulnerable services. The local commissioning groups (LCGs) will be fully involved in performance management and improvement, and, importantly, the Bill recognises that the regional board should be accountable for the management of family practitioner services. I remind Committee members that 20% of all resources are spent on family practitioner services. The strategy and policy is to move increasingly from providing services in hospitals to providing them in the primary-care arena and in communities themselves. It is very important that that be seriously represented in the structure of the regional board.
600. The local commissioning groups should play a lead role in engaging communities and in identifying local priorities for improving health and well-being. The majority of services should be commissioned locally. Only very specialist or vulnerable services, or services that cater for small numbers of people, should be commissioned regionally.
601. In order to do that, people must be located locally. One cannot be in touch with the needs of one’s local community, and with its activists and representatives, unless one is co-located and close to the ground. We firmly believe that staff from the board, the agency and the regional support services organisation, whose jobs directly relate to local issues, should be co-located in order to ensure that they work together properly — that should be done locally. Over-centralisation of those structures would not be a good idea.
602. As far as the regional agency for public health and social well-being is concerned, the three domains of public health should also be integrated and co-located in order to facilitate local working. The first of those functions is health improvement — including initiatives such as Investing for Health — and health promotion.
603. The second function is health protection — including vaccination — against outbreaks of communicable diseases. Health protection also covers environmental hazards, which is an issue of increasing importance and of public interest and concern, and emergency planning — ensuring effective responses to pandemic outbreaks of flu, major outbreaks of communicable diseases or a major emergency event such as the disastrous aftermath of a dirty bomb. Responsibility for the aforementioned should lie with the regional agency.
604. The third function is to provide input into the commissioning process, which will assist integration of the regional agency with the LCGs.
605. There is a need for the LCGs to be properly informed, so important links must be made with the regional agency, the Department of Health, Social Services and Public Safety, and bodies such as Ireland and Northern Ireland’s Population Health Observatory (INIsPHO), the Northern Ireland Cancer Registry and relevant departments at Queen’s University. Yesterday’s announcements about the increase in melanoma rates will not have been lost on Committee members. It is important for a public-health agency to have that kind of intelligence and information, enabling it to monitor progress against targets.
606. I will now move from structures to people. People are a vital resource in making the changes work. There will be fewer of them, and we must ensure that we have the right people in the right places. We welcome the fact that, at this stage of the proceedings, the chairpersons’ positions have been advertised and the appointment panels will sit in early October. As well as that, the advertisements for the posts of chief executive have been published. That is all about trying to meet an exacting timetable and moving to a position in which people can tell their staff that, all things being equal, and assuming that the Health and Social Care (Reform) Bill passes, they will be able to transfer on 1 April 2009. In bringing people along, it is important to be able to tell them where they are likely to be situated and what they will be doing.
607. That takes me to the next point, which is all about location, location, location. We support the need to implement the reforms as quickly as possible. We recognise, however, that if we have regional bodies with local outworkings, it is important to ensure the equitable distribution of local employment opportunities to match. We understand that there are some policy issues outstanding, and Sir George Bain and his team are currently reviewing those in another place.
608. We expect that, although the new bodies’ headquarters will comprise more senior staff, they will have to be supported by people in lower grades, who may be much less mobile. We must be careful that nobody feels that they are being asked to work in places that are unsuitable for them for practical, and other, reasons. Many women in the lower ranks have other responsibilities that tie them near to where they live. There are issues of equity and fairness, but those issues differ from issues that arose at the time of the trust mergers. In that instance, staff largely stayed where they were, particularly those who were working at the coalface.
609. The Minister is fully committed to avoiding compulsory redundancies, but no guarantees have been given. ICT and modern ways of working, in a remote sense, can enable those changes to happen.
610. Accountability is about having clear lines of distinction among the roles of the new organisations, and among the Department, the Minister and the trusts. The Department of Health, Social Services and Public Safety will retain financial accountability for the trusts, while the board and the agency will have responsibility for the commissioning of performance management. The operating framework, which underpins the legislation, must be clear about who does what and when, in order to prevent a situation in which the commissioners pursue the implementation of targets and priorities, while performance and financial accountability is pursued on different lines. It is vital that there be crossover.
611. Although we welcome that fact that local councillors will be represented on the regional agency and the local commissioning groups, the issue of dual mandates should be considered against the number of councillors required under the latest proposal to establish 11 new councils. The roles and responsibilities of members of the LCGs, the regional agency, and the patient and client council should not be duplicated. There may also be issues around how local councillors are identified and selected to serve on those bodies. However, that is not for us to comment on.
612. In conclusion, we recognise the huge scale of change. The process is more complicated than the trust mergers. We are creating four new organisations, whereas the trusts were merged to form bigger organisations that performed the same functions. As leaders of our boards, we are committed to managing that transition. We try to maintain the morale and knowledge base of our staff. We want them, albeit in fewer numbers, and their expertise to transfer to those new functions.
613. The Department has set up a number of work streams aimed at planning the fine detail of the operating framework. There is a number of projects groups. For the Committee’s information, I appended a communications document, issued by the Department, which lists the names of who runs what and who belongs to which work stream. A further 19 pages may be downloaded from the Internet, if members want to know exactly who does what.
614. In the background, people are working hard to produce the essential operating details, which will underpin the structure and help it to work. Clearly, communication is vital in order to keep everyone on board and to deliver the reforms to the timescales.
615. My colleagues, who have also contributed to the process, will wish to discuss a variety of issues.
616. The Chairperson: How is staff morale? Are staff being kept informed of developments?
617. Dr Kilbane: Every attempt is made to keep staff informed. However, we await movement on some issues. Staff enquire about what kinds of jobs they will have to apply for and where those will be located. Some of those questions cannot be answered. Structures are being worked on at a departmental level. The working groups are building up a head of steam, and we expect staffing issues to become clearer soon.
618. Our staff see the end point approaching, and that is helpful for them. Our vacancy rates being what they are, I do not pretend for a minute that staff do not struggle daily to get everything done — they do struggle. However, my general sense is that, as we approach the end point, people who were in a dark place a while ago are now beginning to see the light at the end of the tunnel. My colleagues may not agree with that comment.
619. Mr Dominic Burke (Western Health and Social Services Board): No, that is the situation. Staff fall into two, if not three, categories. One category is those people who are charged and ready for the new world; they want to be involved, and are clearly up for it and ready to go. Many of them will continue to do the jobs that they currently do to the same standard as before.
620. Some staff are coming to the end of their career and are getting ready to leave. The people whose morale is most significantly hit are those who are uncertain at present. People who are leaving see the end in sight and are up for delivering in this transitional period to ensure that the 2008-09 activity is carried out to a high standard. Those who will be in the new world will join the new teams and get on with planning for 2009-10 and beyond. As is to be expected, it is those who are uncertain about what is happening who have a degree of anxiety.
621. The Chairperson: Has there been a mass exodus of professional staff in any significant healthcare areas to the private sector or elsewhere?
622. Mr Stuart MacDonnell (Northern Health and Social Services Board): There has been a significant exodus, but I would not say that it has occurred at any particular grade. Like my colleagues, I try to meet staff informally once they have handed in their resignation to find out their reasons for leaving. A mixture of reasons is usually involved, with the need for certainty featuring most often. Some people are moving horizontally to a place of certainty. Small numbers are moving across the water, with others moving to the private sector.
623. A significant number are moving into the trusts — they are further down the road in the restructuring process. They may have reached a point in their restructuring whereby they have been unable to fill some posts in what they call the legacy trusts — the previous trust in that geographical area. In those cases, the trusts open the posts to the wider RPA group, and people apply for them simply because they are the first jobs to become available. We have suffered as a result of that trend. I hope, however, that it is coming to an end. In November, three years will have passed since the first changes under the RPA were announced — that is a long time. We assume that, once the senior staff take up their posts in the new agencies over the next couple of months, matters will begin to speed up.
624. The Chairperson: Let us hope so.
625. Mrs M O’Neill: You said, Paula, that the effectiveness of the local commissioning groups will hinge on local input. Should there be a statutory requirement for them to carry out proper consultation? I know that they will have a public consultation role, but should a statutory requirement be placed on them to consult publicly on their decisions?
626. I also want to know about the role that the Department will have in drawing up frameworks and in establishing aims and objectives for the different health and social care organisations. Will that give the Department a mechanism through which it can exercise control over the new bodies?
627. Mr S MacDonnell: It was a politician who said that all politics is local — I think that it was the late United States senator Tip O’Neill. The Minister is clear that a significant number of elected local representatives will sit on the boards of the local commissioning groups — perhaps four. An issue may arise with the establishment of the groups when the outcome of the new Local Government Boundaries Commissioner’s review is known. However, let us assume that that has all happened. The local commissioning groups will technically be committees of the regional health and social care board, which will be accountable to the Department. The regional board will be bound to implement the wishes and policy of the Minister of the day, and, in turn, it will ask the local commissioning groups to ensure, through service frameworks and the like, that they are working to that policy.
628. However, that said, there should be a large range of issues within the local ambit of a local commissioning group. There should be scope for difference rather than adopting a uniform approach.
629. Key to how the new system will work is how much autonomy those LCGs are afforded, after they have dealt with the pressures of the Minister of the day and the financial situation, which is not of the LCGs’ making. I believe that there is a requirement in the Bill for the regional board to consult widely on any plans. I am sure that it, in turn, could by management instruction bind the LCGs to do the same. However, whether enshrined in legislation or not, I am convinced that the LCGs will do that anyway.
630. Mrs Fionnuala McAndrew (Southern Health and Social Services Board): Having a statutory duty to consult does not necessarily mean that that consultation is more effective. Sometimes consultation can be tokenistic, even when required by statute.
631. Stuart is saying that if there is a duty on local commissioning boards to consult, and if the framework document or plans for how the LCGs should conduct their business are clear, that will encourage creative consulting methods. That consultation would then be conducted with a range of people with an interest in health and social services, and could be more productive than through statutory duty, where some people just tick the box.
632. Mrs M O’Neill: What about the creation of framework document? Clause 5 of the Bill states that the Department must work with each new health and social care body to draw up a framework document that establishes that new body’s functions. Will that be advantageous and defeat any further problems down the line?
633. Dr Kilbane: That will ensure that all the boundaries join up, which is very important. We must know who is accountable for what, what the rules of engagement are and what it is that people must do when working with one other. Furthermore, if certain functions are not delivered, we must know who takes action and what the sanctions, or, alternatively, the rewards, may be. It is essential to have a framework document, and that document must be thoroughly developed and tested. That will ensure that the people who work in the different arenas are quality-assured.
634. Dr Deeny: First, I declare an interest in LCGs. My question relates to what Stuart was talking about.
635. The regional health and social care board can overrule the LCGs. Therefore, LCGs are really local advisory groups, dealing with public-administration systems. They are not commissioning organisations in the sense that primary-care trusts in England are. Given that, do you not feel the term LCG to be misleading?
636. You have both referred to the fact that decisions are best made locally. My concern is that people on the LCGs will believe that they can be overruled by the regional board at any time. What do you think about that? Do you think that that should be the case, or do you believe that the LCGs should have the same clout as primary-care trusts in England? There, the primary-care trusts commission only in exceptional cases, and only very exceptionally are they overruled by a central body.
637. Mr S MacDonnell: Dr Deeny has hit on a pivotal issue. There need to be checks and balances in any system. Wearing his MLA hat, Dr Deeny expects the Committee to hold the Minister to account for what happens in health and social services, and, in turn, for him to have control over the various agencies that act on his behalf. As MLAs, you would not accept it were the Minister to say that a matter has been delegated to people for whom he has no responsibility. However, if everything is controlled from the centre — the point that Dr Deeny makes — what scope exists to have creative and energetic people working locally to resolve local problems?
638. It is more to do with the style used to operate the arrangements than it is to do with the statutory basis on which the different agencies are established. If the centre is very controlling — I am sure that all members are aware of organisations that operate like that — parts of the organisation, on the peripheries, may feel marginalised. Equally, I am sure that it would not be acceptable, certainly not to the Northern Ireland Audit Office or to the Assembly, if the centre were relaxed and did not know what was happening on the peripheries. There are, therefore, checks and balances.
639. The framework document, which is intended to wrestle with those checks and balances, is what we are all interested in seeing. None of us has yet seen it, Dr Deeny. Therefore, when the document emerges, I want to bench-test it to see how it deals with the issue of autonomy versus the mandatory requirement to implement the Minister of the day’s wishes.
640. Dr Deeny: I know some GPs who sit on local commissioning groups, and not only on the group on which I sit in the west, who would like to think that they are accountable to a regional body yet have the power to commission locally, and with the necessary financial backup. That is a concern at LCG meetings that I have attended, and in other LCGs. If commissioning groups do not have the clout and financial resources to back their decision-making, I do want to see GPs or other primary-care representatives walk away from local commissioning groups.
641. Mr S MacDonnell: What you have said is what, in principle, the policy direction is trying to achieve. My colleagues and I are beaten down by the pragmatism of our experiences. Sometimes the pressure of the issues of the day is such that, by the time that one has dealt with them, it is the end of the day. One then goes home, only to come in the next day to encounter more issues.
642. The framework document will, therefore, have to address the freedom to manoeuvre that you seek in the system, and I urge you to make your suggestions, whether as an MLA or through the British Medical Association (BMA), or both, in order to ensure that those freedoms are there. As I said, however, much will be in the style of operation as opposed to what the framework document says.
643. Dr Kilbane: I am more optimistic, because the intention — although we will have to wait and see what emerges — is that there will be devolved local budgets. The emphasis is that only those functions that can be commissioned regionally should be commissioned regionally — the power should lie locally. That is the intention, and I believe that people are genuine in that intention.
644. Furthermore, locally elected representatives on the LCGs will undertake a great deal of scrutiny; therefore, decisions will not be taken in darkened rooms. There will exist real power for LCGs to commission within the scope of the policy framework. They cannot send rockets to the moon if that is not the purpose of the enterprise, but they will have enough power to make decisions about local issues.
645. There is another side to that coin, which is that some of the decisions that LCGs make may not be popular locally. Therefore, be careful what you wish for, because living in the straitened circumstances of a confined budget means that it will be possible to do some things and not others, and some things will have to change — all of which is difficult to achieve.
646. The object of the exercise is that if everyone is on board and given the freedom to make decisions, that represents an important step change, and one that is genuinely expressed in anything that I have seen so far.
647. Mrs Hanna: The rationale behind the framework document is, I suppose, to reduce bureaucracy and bring services closer to people and patients. The bodies must, however, have members with the necessary expertise and knowledge, particularly on public-health matters. I am thinking particularly of health inequality, which is a big concern for everyone, because the gap it is getting wider all the time. Therefore, people must be in place who can make the necessary decisions, and we do not yet know that that will be the case. I will have a concern until more is known about what is happening.
648. The Chief Medical Officer is talking up prevention, rather than talking of picking up the pieces, so it is important that the expertise is in place, and that expertise must be joined-up. Bottom-up and top-down approaches must be taken, in order that the groups on the ground, such as those concerned with healthy living, are properly involved. Everyone is concerned about how that will all come together to make a difference.
649. Mr Burke: You are absolutely right. The important point concerns working together, and Dr Kilbane made that remark in her opening statement. The regional agency for public health and social well-being must work with the regional health and social care board. People who are currently involved with Investing for Health and health action zones will work as part of the regional agency. Local commissioning groups will include local representatives and will have the voice of the people.
650. Those people will come together to ensure that effective local health-improvement initiatives are running. The test will be whether joint planning emerges at the top level that is informed by local commissioning and by local groups. People will recognise that working together at ground level results in the implementation of the most effective plans.
651. Mrs Hanna: Therefore, it is not only about consultation. The people who are closest to the problems must inform the legislation.
652. Dr Kilbane: We understand the concept of a joined-up approach in the local areas to mean that the relevant folk from the regional agency — representatives from organisations such as Investing for Health and Wellnet — will work alongside the regional board at a local level to ensure that informed and sensible decisions are made. Otherwise, they would not be able to write a local commissioning plan, part of which requires them to outline what they are in doing, for instance, to invest in community groups and narrow inequalities.
653. At the regional level, the chief executive of the regional agency will have to ensure that that adds up to something that will deliver on inequalities across Northern Ireland. On that regional level, work must take place on an inter-agency basis. We acknowledge that that is not simply the Department of Health, Social Services and Public Safety’s baby; the work is also concerned with housing and education. Whoever gets the interesting job of chief executive of the regional agency for public health and social well-being will have to fulfil that role regionally, and that will be on the basis of joined-up local arrangements.
654. Mr Burke: Community planning, on which local councils will lead, will have a key part to play. That will bring more people to work together by statute in order to deliver that agenda.
655. Mr Gallagher: How do you see the reforms progressing? You talked about the importance of a balance that allows for grass-roots involvement in the regional board. Local influence on service delivery is important. How do you envisage that happening? The purpose of the exercise is to trim down our Health Service and to try to ensure that money is spent on front-line services rather than on bureaucracy. If the two elements are to be the regional board’s central function and local influence, can that be done, and can savings be achieved at the same time?
656. Dr Kilbane: The aim, and the challenge, is to cut 25% of the current cost of the health and social services boards and the other legacy bodies in Northern Ireland over three years. Therefore, the new designs will be based on a target of having 25% fewer staff by the end of that period, or whatever equates to a 25% reduction in costs, which is between £12 million and £13 million. That is achievable. It is happening already, because a vacancy-control programme has been in place in recent years — that is, since the changes were mooted — with the result that organisations are already operating with significantly fewer people in permanent positions. Therefore, even before the point of change, we have started managing the numbers downwards.
657. Earlier, we referred to the fact that some staff will decide not to stay with the health and social services boards. As present, our assessment of the numbers shows that we are well on target to achieving those savings, which, paradoxically, could result in a scenario in which we lose more of the necessary expertise than we should. We have lost a number of key people to organisations that seem to have a more certain future, so we must be sensible and make appropriate decisions about enabling people who need to work locally to do so. We will not be in control of the process after 1 April 2009, but, from where we are standing, we are definitely on target to achieve the reforms.
658. Mr S MacDonnell: To set that in context, the comprehensive spending review’s three-year target for the entirety of health and social services in Northern Ireland is £343 million, which is a huge sum of money. The target for the organisations that we represent, as well for the Central Services Agency and the Health Promotion Agency, is £13 million, which is approximately 4% of that target.
659. The RPA saving from reform of the first-phase organisations — the trusts — is £39 million. Therefore, the overall RPA target for Northern Ireland’s health and social care sector is £52 million. I agree with Paula that the £13 million target is achievable. We are halfway through the first of the three years and, as I said to you earlier, Chairperson, because so many people have left ahead of the change, we are almost ahead of the wave of change.
660. However, that target only equates to 4% of a very large figure, and, as the Committee is well aware, freeing up that amount of resources is a task that the trusts are wrestling with. It is a huge challenge for them. Our £13 million saving is welcome because it is a significant sum of money, but it remains a small part of a very big challenge for the entirety of health and social services in Northern Ireland.
661. Mr Easton: Are there any functions that the trusts are concerned about losing to the regional board, the regional support services organisation or any other agency?
662. Mr S MacDonnell: In time, some functions will migrate. From memory, those will include financial systems management, HR, recruitment, processing, some aspects of estate management, and so on. Those are outside my remit, but I am aware that seven or eight trust functions have been highlighted as moving to the RSSO. In turn, those may be grouped together in different sectors in Northern Ireland rather than their all moving to some kind of central administrative factory.
663. When it is appointed, the RSSO management team will have to liaise and negotiate with the trusts. A document setting that out has already been published and consulted on. I am sure that, in due course, the Committee will want to hear from the people who are driving that. That is not something that we are driving; however, one of the work streams that Dr Kilbane mentioned is dealing with that issue. A small number of board staff will migrate to the RSSO
664. The entire Central Services Agency will migrate also. However, the greater number will come from trusts, and I expect that to happen over the next three to five years.
665. Dr Kilbane: We do not believe that any functions will be lost as a result of the reforms. As custodians of the boards’ functions, we must perform due diligence to ensure that the new structure — although it will have fewer staff — carries out the essential functions. We have no reason to believe that that will not be the case.
666. The Chairperson: Everyone who indicated that they wanted to speak has done so. Thank you all for coming to the Committee and for answering members’ questions. The Health and Social Care (Reform) Bill represents the greatest shake-up of the Health Service in its history, so I hope that we get it right.
25 September 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Ms Claire McGill
Witnesses:
|
Ms Alice T Casey |
Regulation and Quality Improvement Authority |
667. The Chairperson (Mrs I Robinson): The Committee will now hear evidence from the Regulation and Quality Improvement Authority (RQIA). I welcome Alice Casey, the interim chief executive of the Regulation and Quality Improvement Authority (RQIA); Phelim Quinn, its director of operations; and Jude O’Neill, its head of mental health and learning disability. We have set aside 40 minutes for you to make your presentation and to take questions from Committee members. I will now hand over to you.
668. Ms Alice T Casey (Regulation and Quality Improvement Authority): Thank you very much for inviting us, Chairperson. Malachy Finnegan, our communications manager, is with us this afternoon as well. I will take a couple of minutes to make a few opening remarks, and then Phelim and Jude will talk more about how we will operationalise the functions of the Mental Health Commission, subject to the legislation’s passing.
669. The RQIA welcomes the opportunity to provide oral evidence to the Committee on the Health and Social Care (Reform) Bill, and to clarify, and expand on, the written evidence that we previously submitted. We were established in 2005 to register and inspect health and social care organisations across Northern Ireland. Our powers in the regulated sector include the ability to carry out announced and unannounced inspections of care organisations, nursing homes, residential homes, children’s homes, and a whole range of other services that came under our regulation on 1 April 2008.
670. Our powers include the ability to make recommendations for improvement; to enforce requirements; and to issue failure-to-comply notices. We can also administer the ultimate sanction of prosecution and compulsory closure of those homes. In the statutory sector — that is, hospitals, and community and primary-care services, including dental services — we have the ability to enter premises, to obtain information and to undertake reviews of those services. Some of the reviews that we have already undertaken include the hygiene reviews, which were publicised quite recently; clinical and social-care governance reviews of all trusts, and many more. The review that we are currently finalising is the clostridium difficile review, which is to go to the Minister shortly.
671. All our reports are made public and are available on our website; everything that we do is published. The RQIA cherishes and will defend vigorously its right to independence. We are the independent regulator for health and social care in Northern Ireland; we are independent in thought and purpose, and we believe that our work to date has demonstrated that. We have no qualms over reporting on what we see when we inspect or review organisations.
672. We review constantly our practices, we learn from sharing our experiences with other regulators across Northern Ireland and the rest of the UK, and we collaborate and share expertise. We also use clinical experts from across the UK when we review particular services, and we have experts to look at those services objectively. We used experts when dealing with the clostridium difficile outbreak, the hyponatraemia review and our review on blood safety. We will also use experts for our planned review of maternity services across Northern Ireland and for child protection arrangements, and so on. We have a wholly lay board that is made up of 12 members and a chairman.
673. The Bill does three things for the RQIA — we shorten the name of the authority to RQIA, because we find it easier to say. First, it tidies up our title and establishes the RQIA in legislation, — in place of the Northern Ireland Health and Personal Social Services Regulation and Improvement Authority — and that is welcome as it clarifies the situation for many people.
674. Secondly, the Bill impacts on the organisations that we will review. For example, we will have responsibility for reviewing and regulating the proposed new regional organisations: the regional health and social care board; the regional agency for public health and social well-being; and the regional support services organisation.
675. Thirdly, it transfers the functions of the Mental Health Commission to the RQIA, and that change is welcome. Since the transfer of the Mental Health Commission was first mooted some 12 to 18 months ago, the RQIA has worked collaboratively with the Mental Health Commission on a range of issues. Over the summer, we took a strategic approach on an operational level to discuss and plan how the services will come together, if the legislation comes into effect from 1 April 2009. We have established a project board, which includes the chairman, the chief executive and the commissioners of the Mental Health Commission with officers of the same rank in the RQIA.
676. The project board’s work to date has included developing an action plan in response to a due diligence report that the RQIA had undertaken; clarifying the legal implications of the change on the Mental Health (Northern Ireland) Order 1986 for the RQIA; clarifying the implications for our board — our 12 lay members and chairman; reaching agreement on the workforce plans and the financial implications with the Mental Health Commission; and developing an appropriate communications plan so that the public know exactly what is happening. The project board’s work has also included developing and reaching agreement on how the RQIA will take over the Mental Health Commission’s operational work. That was an important piece of work, and I am pleased that we achieved full agreement with the Mental Health Commission at our project-board meeting last week. We have now agreed how we will take the work forward, which is a major step.
677. The pathway is now clear for the transfer to take place. The RQIA is ready, willing and able to progress that important work, and it has wider powers than the Mental Health Commission. It means that the Regulation and Quality Improvement Authority will regulate all services in the health and social care family in Northern Ireland. It will also be subject to the necessary vigour that is required under the regulation.
678. I shall now had over to Mr Quinn and Mr O’Neill, who will tell the Committee how that will be done.
679. Mr Phelim Quinn (Regulation and Quality Improvement Authority): I shall deal with the discharge of the functions of the Mental Health Commission under the RQIA and the comprehensive model that we have developed in conjunction with the Mental Health Commission’s senior management staff.
680. In developing the comprehensive model, we have worked in partnership with the mental-health commissioners. We have also used the resources of senior psychiatric professionals across Northern Ireland. Establishing the dedicated mental-health and learning-disability team under that model has been an important factor in developing and delivering the functions of the Mental Health Commission, as set out in the Mental Health (Northern Ireland) Order 1986. I will speak in more detail about the model as I go along.
681. That model enshrines several factors. First, the specific care, treatment and human rights of individuals are embraced in the Mental Health (Northern Ireland) Order 1986. It has been stated that the RQIA concentrates on systems and organisations, but the authority also fully acknowledges its requirement to focus on individuals.
682. Secondly, it is stipulated that there must be engagement and consultation with wider service users, their groups and advocates. The RQIA is concerned about the context in which care is provided. In a previous submission to the Committee, the authority was told of concerns about psychiatric-unit environments in which care is provided in Northern Ireland. I will address that issue later.
683. Thirdly, there must be an assessment of the level and availability of care using quality standards, at the same time as considering clinical- and social-care guidelines, legislative regulations and legislative standards.
684. All those elements will be incorporated in the RQIA’s work under the 1986 Order and the Health and Personal Social Services (Quality, Improvement and Regulation) (Northern Ireland) Order 2003.
685. Account must also be taken of enforcement action in response to non-compliance. With both organisations working in tandem under the two relevant pieces of legislation, the responsibility for enforcement lies with the RQIA. Therefore, to some extent, the circle will be squared when it comes to discovering what is going wrong. We can then make recommendations and take any required enforcement action.
686. The RQIA is committed to promoting and protecting the core functions of the Mental Health Commission. In order to do that, key issues in several areas must be addressed. Those issues include independence, multidisciplinary working, investigative action, inspectorial action, advisory and advocacy work, and protection of patients and the public.
687. Finding a new way forward involves using the powers that are combined after the transfer in a manner that reflects the Bamford Review’s aspirations. Any work that the RQIA does will be future-proofed in line with that review’s aims, objectives and legislative recommendations. The RQIA will retain and develop its commitment to focus on the individual and the rights of service users and of their carers, incorporating enforcement powers.
688. The authority will promote multi-professional and lay working. The RQIA wants to include the lay concept in its work under the Mental Health Commission, and in the broader remit to the RQIA itself for inspection, review, governance and service reviews.
689. Extra emphasis must be put on the promotion and sharing of good practice across mental-health and learning-disability services. Once found anywhere else in the rest of the UK, in the Republic of Ireland or, indeed, in the rest of the world, examples of good practice will be shared with services.
690. There will be a drive to encourage wider promotion of service-user engagement on mental-health advocacy. That means more than simply looking at mental disorder and learning disability per se; it involves the promotion of good mental health in the Northern Ireland population.
691. The RQIA seeks to enshrine respect for everyone’s human rights and the right to timely, high-quality care. It aims to promote choice and to listen to the needs of individual service users and the views of their carers in order to develop a culture of learning and innovation. The authority will find and challenge deficient practice, and it will show integrity, and be open and transparent, in its work with service users.
692. The RQIA wants to work in a more accessible, responsible and targeted manner. It will engage more with the public. The RQIA is about to close consultation on its public-participation strategy. Among the key factors to be inserted into that strategy is the authority’s work in the areas of mental health and learning disability. It is also hoped that two external reference groups with service users will be established — a specific one each for mental-health service users and learning-disability service users. That will enable the RQIA to obtain both constituencies’ views, which will further inform all aspects of its service provision.
693. On the issue of operational alignment, the RQIA regards the transfer as an opportunity to build on existing resources by adding an expert specialist team of full-time and paid sessional multi-professional officers. Mental health commissioners are currently part-time members drawn from a range of professions. The commission has always aspired to have full-time officers. There is now the opportunity to employ those full-time officers and to supplement skills and expertise with sessional workers, such as psychiatrists, approved social workers and other care workers, who may not be represented in the full-time workforce.
694. In line with the Bamford Review recommendations, the RQIA visiting programme will include annual announced and unannounced reviews and inspections of mental-health and learning-disability hospital facilities in Northern Ireland.
695. An additional aspect of that programme that we wish to emphasise is that it will not just comprise visits to hospitals and buildings but will review the effectiveness, quality and safety of the new service-delivery models for mental health and learning disability that are developing throughout Northern Ireland. For instance, we wish to evaluate the effectiveness of home treatment and crisis- and rapid-response services, and consider how they address the needs of individuals who use them.
696. We are conscious of the high suicide rate in Northern Ireland, and, therefore, we wish to specifically focus on that. We have just completed a risk-assessment and risk-management review of adult mental-health services, and we wish to maintain that focus in order to ensure that health and social care organisations in Northern Ireland are working in line with the Northern Ireland suicide prevention strategy.
697. There should be a specific focus on services for people with learning disabilities — whether those services are in hospitals or in the community — and we are committed to maintaining a specific review programme for visits to, and inspections of, learning-disability services in Northern Ireland.
698. The Committee may also be aware that, following the transfer of responsibilities for the commissioning and provision of prison health, part of RQIA’s remit means that it now has oversight of those services. Given the incidence of mental-health problems in the prison population, we are required to continue to review the quality, safety and availability of mental-health services in Northern Ireland’s prisons.
699. Another area, which I touched on earlier, is our recent programme of unannounced hygiene inspections. Although called “hygiene inspections”, they consider the general environment in which care is provided. Resonating from our previous discussions with the Committee, we wish to extend those inspections to mental-health and learning-disability facilities in order to help us make robust recommendations about how such facilities should be improved for service users.
700. Those measures consider service provision. We wish to protect the rights of individuals in the service and to maintain a focus on people who are subject to guardianship orders, whether such people be in hospitals, in the community or in regulated sector services in the community. Furthermore, we want to maintain and deliver a service that enables us to monitor the key function of detention under the 1986 Order.
701. We will employ a sessional medical panel to continuously review treatment plans. That panel, under the Order, will appoint part II and part IV doctors. We will also employ a sessional panel of approved social workers to ensure that guardianship is closely monitored in Northern Ireland.
702. We wish to develop a revised code of practice for governance. Work on that has already started as part of the project plan for the transfer of functions, and it will reflect our responsibilities under the 1986 Order. The code of practice will also take account of the relevant elements of the Health and Personal Social Services (Quality, Improvement and Regulation) (Northern Ireland) Order 2003.
703. The functions arising from the 1986 Order will be subject to rigorous, internal performance management in RQIA. We will produce quarterly reports for our board that will reflect activity and outcome measures arising from RQIA’s work on mental-health and learning-disability services. Furthermore, in order to help our board understand the issues for mental-health and learning-disability service users, we propose to develop a mental-health advisory group that will take advice from senior professionals and will reflect the mental-health and learning-disability population in Northern Ireland. Further to our meeting with the project board last week, development of that has already started.
704. Communication is a significant issue, which was also discussed at our project board meeting last week. Up until now, the Mental Health Commission has always used distinctive blue writing paper. When the mental-health and learning-disability services received blue letters, they were always very mindful that those were letters of significance that could have highlighted any issues or problems that arose in those particular services. As a proven brand, the RQIA proposes to use the same blue paper and envelopes that were previously used by the Mental Health Commission, so that that message continues in the services across Northern Ireland.
705. We are very happy to take questions.
706. The Chairperson: Do you want to say anything at this juncture, Jude?
707. Mr Jude O’Neill (Regulation and Quality Improvement Authority): To build on what Alice and Phelim said, the RQIA will endeavour to protect and promote the core functions of the Mental Health Commission, as enshrined in the Mental Health (Northern Ireland) Order 1986, as they transfer across to the RQIA. That includes a commitment to maintaining the spirit of the view of the 1986 Order — an approach that reflects a body that is independent, multidisciplinary, investigative, inspectorial, advisory and protective.
708. The Chairperson: We had a tour of Muckamore Abbey earlier today and discovered that there is 100% occupancy, which means that people are being turned away. Some of the families of inpatients, who may have been here for 40-odd years, think that those inpatients could be put into the community. There is a feeling that that is the way to go, because Paul Goggins said that nobody should be institutionalised by 2014.
709. However, the Committee holds the view that one size does not fit all. We have heard from families and friends of Muckamore Abbey patients who would be loath to see family members who have been here for perhaps 40 years being put into the community — particularly older parents, who could not manage to care for their son or daughter. They would need a 24/7 service, and the cost of providing that is over £100,000 a person.
710. What is the RQIA’s role in a situation in which people feel that their family members should stay in a secure environment rather than being put out into the community? Do you have powers to become involved and make recommendations to reflect the fact that not everyone wants to go into the community?
711. Mr Quinn: The quality standards for health and social care, as published by the Department, are mindful to reflect the views of service users and their carers. They form the basic framework against which the RQIA assesses services. I am in absolute agreement with the Committee: one size does not fit all. In the regulated sector, we find people who regard their placement in that sector as their own home. To some extent, the long-term residents or patients of Muckamore Abbey and their carers regard it, or some of its wards, as their own home.
712. Currently, we have the right to assess those services to find out whether adequate views are taken from service users about how their care packages are being planned, and whether it is appropriate for people to be placed in the community. Through any review process, we will ensure that there is robustness and an evidence base, as well as an engagement with residents and their carers in placing people in alternative services. We will assess those services, and we will make recommendations on the back of those assessments.
713. The Chairperson: There are over 200 people in Muckamore Abbey at the moment, and it is planned that the number of beds will be reduced to 87. However, people are not being placed in the community. Bed blocking and 100% occupancy already exists.
714. How can you argue for resettling patients into the community when, currently, you cannot cope with getting them out of the care facilities? There are people in Muckamore Abbey who should have been out in the community a couple of years ago; they still cannot get out because the facility and back-up to do that is not available. I am interested to hear your views on that, and I welcome the fact that you will examine the issue.
715. Unannounced visits are also an issue. The Committee has asked for its members to be able to examine standards in their own communities and in one another’s communities, collectively or individually, because it is us, the politicians, who get it in the neck. As elected representatives, we are on the front line; our constituents fill mail bags with letters about the state of our hospitals, the lack of hygiene and the non-implementation of the policy of staff not wearing their uniforms outside work. I still see physiotherapists and other healthcare professionals shopping in my local stores while still wearing their uniforms. My understanding is that there is a Health Service-wide policy about not wearing uniforms outside the workplace.
716. Do you think that elected representatives should be allowed to make unannounced visits? Members of the community come to us first, telling us, for example, that their relatives are in a hospital ward that has blood splattered on the walls and floor, that the ward is never cleaned, and so forth. I know that this issue is a hot potato.
717. Mr Quinn: It is, and it is not, a hot potato, in that we believe that patients’ experience is probably the first indicator of their perception of their quality of care. To some extent, the public-observed experience of what is happening in hospitals is the only valid view. Having said that, I think that that must complemented by the professional view on infection-control practices and other forms of estates management relating to infection control.
718. I am sure that elected representatives do go into hospitals, and I am sure that they make comments. We are happy to take those comments on board. The RQIA can take direction about unannounced visits to specific facilities. I am conscious of the Chairperson’s comments at our last meeting, which have been at the forefront of our minds concerning unannounced hygiene inspections.
719. I will give you some background. We were asked by the Minister to conduct a series of unannounced hygiene inspections. We did that without any additional resources, and those inspections were, to a certain extent, a test bed. We have started to recruit a specialist team of inspectors, and we intend to run a full programme of annual unannounced inspections from November. Those inspections will go beyond acute hospital facilities; they will extend into mental-health and learning-disability facilities, community facilities and will also provide advice to the regulated sector. There will be no hiding place from our unannounced hygiene programme. We will be there, and we will report. The inspections may take different forms at different times. We hope that we can do them in clusters, so we will do a round of visits in, for example, a maternity service or in a group of acute mental-health hospitals. We will report on that very openly, as we have done previously.
720. The Chairperson: As elected representatives, we also have a duty of care to our constituents. When we take a phone call telling us that we should see the state of the bed, the ward or the toilets that someone’s relative or loved one is having to put up with, I think that we should be able to do something about that, thereby complementing one another. There is the possibility of overstepping demarcation lines that have been set by professionals, but elected representatives are not going to cost the Government anything by doing this. We are elected and paid representatives, and, therefore, it will not drain financial resources. Thank you for your points; I will take them on board.
721. Dr Deeny: I commend the RQIA. When we met previously, I asked Phelim whether the authority could hold the Department and the trust to account. Since that occasion, you have conducted three unannounced hospital visits.
722. Mr Quinn: We have conducted five visits.
723. Dr Deeny: I can recall the visits to Downe Hospital, Craigavon Area Hospital and Altnagelvin Area Hospital. Where were the others?
724. Mr Quinn: They were at Belfast City Hospital and the Causeway Hospital.
725. Dr Deeny: I commend you for arriving unannounced, inspecting the premises and publicising your findings. It demonstrates that the RQIA can hold trusts to account and, furthermore, justifies the motion that the Committee tabled in the Assembly. Although the Minister wanted to focus on one trust, you visited different trusts. Indeed, four of those visits took place outside the Northern Health and Social Trust, and deficiencies were found on every occasion.
726. Alice mentioned the organisation’s independence. What is your role within the structures? It is difficult for the public, the Committee — and even a healthcare professional such as me — to understand all the acronyms, and so on. Who guides and instructs you? Will you remain independent? That will enable you to hold the Department to account.
727. I reiterate the Chairperson’s comments. Although I have travelled the road to the airport many times, today is my first visit to Muckamore Abbey. I am impressed with the standard of care received by people with learning disabilities. You mentioned that you will assume the remit and duties of the Mental Health Commission. Will you be involved in commissioning mental health?
728. Ms Casey: No, we will not.
729. Dr Deeny: Will you have an influence?
730. Mr Quinn: We will influence the shape of the quality safety agenda for mental-health and learning-disability services. Our focus will be on individuals because, under the Mental Health (Northern Ireland) Order 1986, loss of liberty will be a major issue. We must defend people’s liberty and ensure that, when people lose their liberty under the Order — through a detention or guardianship — it is done within the law, and every technical detail is checked and monitored. Until now, that has been the Mental Health Commission’s role. However, we value the fact that it will be our responsibility from 1 April 2009.
731. Dr Deeny: I have worked in the community for years, and the services at Muckamore Abbey could not be matched or afforded in the community. The services are wonderful, and I am delighted that I came today. Some of the people here are severely disabled and have left the community because they could not cope with the stigma or had been picked on. Moreover, safety is an important consideration. Those people live in a safe environment and in a happy comfort zone. We have all learnt from today’s visit. Will you explain your independence?
732. Ms Casey: The RQIA believes that it is independent. We are a non-departmental public body that is funded by the Department. Therefore, we use public funds. However, beyond that, we determine our own journey. We have a lay board that comprises 13 significant people from Northern Ireland, who, rigorously, hold us to account on our independence. Although some of our work is commissioned by the Department and the Minister, we determine the majority of it ourselves. We establish our own agenda and work, and we are currently planning a three-year programme of reviews of health and social care services and the regulated sector. That review will be unveiled at a board meeting in November 2008.
733. Nobody influences our reviews, which we send to the Department and to the Minister. For the sake of factual accuracy, reports go back to the trust or organisation that we reviewed, but the findings are our findings. That has always been clear to us, and, judging from my discussions with the Department and with the trust chief executives, that approach is recognised and respected as being necessary for governance purposes.
734. As the Bill states, the RQIA currently reviews the health and social services boards and other agencies. We believe that we will review the new regional health and social care board, the regional agency for public health and social well-being, the regional support services organisation and any other new organisations. Although we believe that we are, to a large degree, our own masters, we recognise that we cannot all be our own masters in this world. We will, however, have some element of independence.
735. Mrs Hanna: The RQIA’s subsuming the Mental Health Commission will mean quite a change from its present role; it is an additional responsibility. The commission is concerned with people whereas the RQIA is, perhaps, more concerned with institutions. Phelim listed the endless issues involved; are extra resources available? Much more expertise will be required for the RQIA to go in a different direction. It is interesting that the Mental Health Commission is to become part of the RQIA, and I can understand why that decision was taken. However, will it be within the RQIA’s remit to consider any proposed legislation for competence for patients? Users and healthcare professionals have concerns.
736. Ms Casey: The current budget for the Mental Health Commission will transfer to the RQIA. There will be a slight reduction in that budget because Lombard House, where the commission is currently based, will not have to be maintained. There will be greater economies of scale because there will be no duplication. As Phelim explained, the plan is that a distinct team of people will be employed who are resourced to undertake this important work. The budget is adequate, and we will decide how to use that money.
737. Mr Quinn: As Alice says, we are considering a radically different model of delivery for the functions of the Mental Health Commission under the Bill. We are moving to an employee-based model, which may look slightly more expensive but is, in fact, built within the confines of the existing Mental Health Commission budget. There have been early indications that the Department is committed to that budget, with an in-year uplift for any cost-of-living increases. The money is there; however, if we find that our ability to discharge those functions is challenged by budget restrictions, we will make representations to the Department. The transfer of functions must be done properly; we do not want to cut corners and risk individuals’ human rights.
738. It is a different departure for us, but we are working closely with our colleagues in England and Wales, who are currently undergoing the same type of transfer. From 1 April 2009, in England, the Care Quality Commission is assuming the responsibilities of the Healthcare Commission, the Commission for Social Care Inspection, and the Mental Health Act Commission. Similarly, in Wales, Healthcare Inspectorate Wales is assuming the responsibilities of the Mental Health Act Commission, and something similar will happen in Scotland under the Crerar Review. It is useful to have that peer group working to the same timescale in developing models of delivery for a piece of work that is focused on the individual in organisations that have formerly been focused on institutions.
739. Mrs Hanna spoke about the capacity legislation to which reference is made in the Bamford legislative framework. I will be honest; we will have to consider the details, but it is our view that the RQIA, in subsuming the functions of the Mental Health Commission, will have a role to play in the protection of individuals. I cannot say how that will play out. That legislation has not yet been made, so we do not know the details.
740. Mrs Hanna: When you make those recommendations, you will find — as we and everyone else does — that the resources are not available for their implementation. Will you then act as champions for mental health? I suspect that you will make recommendations, but, as we saw here in Muckamore, the resources are not available, even for good recommendations that everyone supports. That is the situation.
741. Mr Quinn: There is the potential for that to happen.
742. People continually warn that the budget is not available to do x, y or z. However, I will give you a small example. The RQIA happened to be in Craigavon Area Hospital for a clostridium difficile review a fortnight after the unannounced hygiene inspection. We were pleasantly surprised that the chief executive and the chairperson had walked the floor of the hospital after the inspection to ensure that all the estates issues that had been identified as a result of the inspection were being addressed. When we were there a fortnight later, they had been addressed. At times, it had been said that the money was not there to address those estates issues, yet — by virtue of the fact that we were going to publish the findings of that report, which includes photographs of the state of the facilities — action was taken. We were very pleasantly surprised by that.
743. Ms Casey: It is important to remember that not all recommendations cost money and that sometimes we can cut through all of the financial issues and simply get people to do their jobs properly.
744. The Chairperson: Sometimes that is the answer: doing the job properly.
745. Mr Gardiner: Ms Casey, you represent the Regulation and Quality Improvement Authority. For the benefit of the public, I give the full title, as you were directed to do by the Chairperson but failed to do so.
746. I am disappointed by what you said in relation to your organisation. It has responsibility for the hygiene and cleanliness of hospitals. Blame me as being the culprit of Craigavon. I visited the hospital and made public the state it was in, because I had been made aware of the dangers of clostridium difficile, and I know of a lady who died as a result of that infection. That fact was not even recorded on her death certificate, which represented a risk to the undertakers who handled the body. That is under investigation.
747. I met the chief executive of Craigavon Area Hospital, and also the chairperson of the trust, who arrogantly maintained that she knew what she was talking about and asked how I dared to criticise her hospital. It is not her hospital: it is there to help and to cure people. Since the hospital is in my constituency, I represent the people who use the hospital and who work in it. I drew attention to what I had observed: children were going in and out — with their parents, admittedly — at all times, and visiting hours were not regulated. Fortunately, that issue has now been brought into perspective, and visiting times are now enforced. Children were climbing over and under the beds, when clostridium difficile was rife in the hospital. That should not have been permitted, and it has now been brought under control. I spoke with the Minister — blame me again — and voiced my concern about what was happening. He acted, and he told me that he had ordered an independent visit to the accident and emergency department, which was still not up to standard.
748. Had your organisation been on top of things, it would not have been necessary for me, or any member of the Committee, to bring that to the Minister’s attention or to make the public aware of the situation.
749. The Chairperson: Ms Casey, do you have any comment?
750. Mr Gardiner: Guilty.
751. Ms Casey: We are not guilty. The clostridium difficile review required us to examine the state of Northern Ireland’s preparedness for an outbreak. Across Northern Ireland, we found good and bad. Some trusts were better than others. That is what we found, and that is what we reported to the trusts and to the Minister.
752. We are not complacent. There is no doubt that all the trusts can improve, and some show more room for improvement than others. We did a good job on that first part of the review. We saw what we saw on the day that we visited the hospital. We did not, and could not, visit all areas of the trust. We did not visit for a longer period of time because that would have required far too many resources. On the day that we visited Craigavon Area Hospital, what we saw was quite reasonable. Undoubtedly, however, there was room for improvement.
753. Mr Gardiner: Was that on your second visit?
754. Ms Casey: Do you mean was it on our second visit or on the visit that we made in order to carry out the hygiene report?
755. Mr Gardiner: On which visit was the matter first drawn to your attention?
756. Ms Casey: The hygiene report was carried out around two weeks before we visited the hospital to conduct the clostridium difficile review.
757. Mr Gallagher: It is important that you clarify a little comment that is made in Alice’s letter to the Committee Clerk, which states:
“The RQIA recognises that it must make provision in its governance structure for an increased emphasis on mental health and learning disabilities.”
That recognition is important and welcome. First, can you clarify whether it will be your responsibility, or that of the Department, to make an appointment? Secondly, how do you envisage that that will work? Will it involve one individual or several? What do you seek to achieve? It would be best if someone were involved on the board who is a powerful advocate for people who suffer from poor mental health or who have learning disabilities.
758. I am trying to make the point while having every respect for you. We often come across that type of phraseology. Often, the outcome is simply a token gesture. How do you imagine that that will work?
759. Ms Casey: I can say clearly that the board will not have a member who represents mental health and learning disabilities. That is not in the plan. The board consists completely of lay people. It does not have representation from any group at all. It examines how the Regulation and Quality Improvement Authority carries out its work and whether it does so appropriately in all circumstances. However, strong governance arrangements will ensure that we do what we should do in respect of that new area of care.
760. Part of our responsibility is to establish the team that will undertake that work. Although it will be led by Jude, it will be managed by, and accountable to, me. Therefore, a team of people will be dedicated to undertake that work, which will fit into our governance and quality-assurance arrangements, and will be scrutinised by one of our other executive directors. Regular reports will be made. The board currently receives regular monthly reports on work progress with the Mental Health Commission to effect the transfer properly. Those reports will continue after 1 April 2009 so that the board can discuss how progress is being made to absorb the Mental Health Commission’s work.
761. The main focus of Phelim’s earlier point is that an expert advisory panel will be appointed to guide the board and the senior officers of the Regulation and Quality Improvement Authority on how we conduct our work on mental-health and learning-disability services. Therefore, governance checks will be carried out at all levels of the organisation.
762. The Chairperson: Everyone who indicated has been given the opportunity to ask questions. I thank Alice, Phelim and Jude for coming along and giving their presentation.
2 October 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Mrs Liz Cavan |
Allied Health Professions Federation UK |
763. The Deputy Chairperson (Mrs O’Neill): Our next session is representatives of the Allied Health Professions Federation. I welcome Liz Cavan, Liz McKnight and Tom Sullivan to the meeting. I invite you to make a short presentation and answer Committee members’ questions.
764. Mr Tom Sullivan (Allied Health Professions Federation NI): I thank the Deputy Chairperson and members of the Committee for allowing us to present the case of allied health professionals at short notice. We appreciate that the Committee has a busy schedule, so we will try to keep our presentation as brief as possible.
765. Like our medical and nursing colleagues, we have a number of concerns about the proposals for health and social-care reform. We also have a different perspective from our medical and nursing colleagues on how some of those proposals will be played out. The purpose of our presentation is to demonstrate the unified and collective view of allied health professionals.
766. The Allied Health Professions Federation represents more than 6,000 health and social-care workers throughout Northern Ireland. We work on all programmes of care and with all age groups. Initially, we welcomed the proposals for health and social-care reform as an opportunity to redress deficiencies at departmental, board, local-commissioning-group (LCG) and trust level and to reposition allied health professions in those various structures. Some of our concerns have been addressed, but the proposals overlook many of the concerns that we have raised.
767. I appreciate that the evidence session’s focus is not on the departmental structures. However, the departmental structures should also be reviewed to ensure that they are compatible with the other proposed arrangements. The legislation outlines the remit of the Department as a policy-development role for improving the health and social care of the population of Northern Ireland. However, the top-structures review, which was completed in August 2006, highlights the deficiencies of the department’s policy process.
768. Like our medical and nursing colleagues, we welcome the creation of a single regional health and social care board and the abolition of the four trusts. However, we have reservations about the representation of allied health professionals on that regional board. We welcome the emphasis that the regional agency for public health and social well-being will place on health promotion and protection. Allied health professions have a significant role to play in the public-health agenda. Our skills have been underutilised in the past, but that deficiency can be addressed now.
769. My colleague Liz Cavan, who is the chairperson of the council of the Chartered Society of Physiotherapy and a member of the Allied Health Professions Federation UK, will present our concerns about the proposed commissioning arrangements.
770. Mrs Liz Cavan (Allied Health Professions Federation UK): The Allied Health Professions Federation broadly supports the concept of commissioning to secure the best possible outcomes for health and well-being. We promote an inclusive approach, in which the staff who deliver the services have genuine ownership of the local commissioning groups’ plans.
771. It is planned that each group will have one allied health professional on it. Like the Royal College of Nursing Northern Ireland (RCNNI), we believe that each allied health professional will have a very broad church to deal with, and will need their colleagues’ support in order to deal with that effectively.
772. We very much believe that a bottom-up approach should be adopted, with professionals, users and local government having input into the plan. Working together, the front-line services could really take ownership of that commissioning plan and feel that it is theirs and is seen to be inclusive.
773. I hope that this does not ruin me, but I was involved with the commissioning arrangements for the local health and social care groups (LHSCGs). Although there were definite deficiencies — particularly their not having GPs on board — those groups achieved some good things. They would have been strengthened, unlike our British Medical Association colleagues suggested, by the inclusion of local-government officials. Some members may be aware of some of the initiatives that the LHSCGs started.
774. Allied health professionals work with local government: speech and language therapists work with SureStart in areas and wards of deprivation; and occupational therapists work with their housing colleagues. New work is taking place in leisure centres, where physiotherapists are training leisure-centre staff so that people with long-term conditions can receive rehabilitation to keep themselves as fit as possible. Working with our colleagues has made that work possible.
775. That partnership will do nothing but help the health of the population. Physiotherapists and dietitians are working with leisure-centre staff to tackle obesity. Our dietitians are also working with environmental health officers to give consideration to the issue of food-labelling. There are many areas in which we feel that health and well-being will be supported by taking a bottom-up approach.
776. From that point of view, we differ a little from our medical colleagues. Clarification is required in the commissioning process on the extent of the financial controls. We agree with the RCNNI that there must be clarity on the groups’ authority. Care is also needed to ensure that there is no duplication between the regional board’s role and that of the LCGs. It must be clear who commissions what, in order that duplication is avoided. Regional commissioning must have a local flavour — localities must have an input into what is commissioned regionally. The problem is that we have yet to see some detail.
777. Ms Liz McKnight (Allied Health Professions Federation NI): I shall talk about the proposed patient and client council. We fully support the establishment of one patient and client council, but one in which the five local offices cover the same geographical area as the trusts.
778. We need to ensure that there is adequate capacity in those local offices to provide a strong voice for our local population to be able to understand the structures in the individual trusts. There is a great deal of variance among trust structures and processes right across Northern Ireland. It is important that local people can get to grips with their local trusts’ processes. When working in a trust, it is sometimes difficult to know what the processes in that trust are, let alone try to figure out what is going on in another trust.
779. We would also support and acknowledge the role that the voluntary and client-representative groups would have in those local offices. That is important, because it would provide patients with a real voice. Patients who currently feel unable to voice their concerns could do so, and there would exist a representation that could channel and challenge patients’ experience.
780. We know that patients sometimes find it difficult to access the healthcare services that they require because of barriers, and they want someone to represent their view. Voluntary groups can often be a useful advocate for patients.
781. We also want to comment on the Regulation and Quality Improvement Authority (RQIA), which is responsible for overseeing the quality of patient services across Northern Ireland. Our medical, nursing and social-services colleagues are all represented at director level in the structures of the RQIA. However, allied health professionals do not have similar representation, despite a recommendation from the Department. Therefore, there is a gap in the monitoring of the delivery of the quality, effectiveness and safety of the services that our patients use.
782. Allied health professionals want to work in partnership with all the groups that are involved in healthcare delivery, including our colleagues from the different professions, local government, and, particularly, our patients and clients. Having all parties engaged in the process is the right direction for the new structures to take. We thank the Committee for its time.
783. The Deputy Chairperson: When we met informally, one of your concerns was the inadequate support structure in the Department for your professions. Has that situation improved any since we last met? I know that all trusts were supposed to appoint someone to liaise with the allied health professions, but has that happened?
784. Mr Sullivan: Last Friday, we were informed that there is nobody at a departmental level with responsibility for issues that pertain to the allied health professions. There is an allied health professions adviser in the Department, who has been on long-term sick leave for a while. Some civil servants were seconded to do specific project work and undertook the adviser’s role to provide advice to the Department. Those secondees have since retired. Therefore, as of last Friday, there is no one in the Department with the appropriate expertise and experience to advise it on issues that affect the allied health professions.
785. When the review of public administration (RPA) proposals were being considered last year, the allied health professions adviser was, again, on long-term sick leave, which meant that there was nobody at departmental level to advise appropriately the various working groups that were examining the proposed changes to the structures. Therefore, there was no effective input from the allied health professions. We raised that issue with the Minister last October, and secondments were made. However, as I said, those people have since left, so we are in a worse position, because there is no one in the Department to offer advice on issues that affect the allied health professions. It would be unimaginable to have no nursing or medical advice at the Department, yet that is the position in which we find ourselves.
786. The Deputy Chairperson: That is incredible, especially after the representation that the Committee made on the matter after we first met the allied health professionals. We will have to take that issue up with the Department. You must be concerned that, despite all the restructuring, the views of allied health professionals have been left out of the equation.
787. Mr Sullivan: Even if the adviser were to return from sick leave, there remains an issue of capacity — there would be only one person to cover all the work streams in the Department, including workforce development, training, and strategy and policy advice. Therefore, there would still be no capacity or structure for allied health professions at departmental level. The adviser’s status in the Department is not reflected as it is in other areas of the UK. In England, Scotland and Wales, there is a chief health-professions officer at departmental level, who has a direct link to the relevant Minister. Our adviser does not have that status in the Department. Even if the adviser returns, neither the structure nor the support for the role is in place.
788. The Deputy Chairperson: The Committee will raise that point with the Department.
789. Mr Gallagher: Thank you all for attending the Committee this afternoon. You expressed your concerns about the proposal for only one representative from the allied health professions on each new local commissioning group. I share that concern, because there is a wide range of allied health professionals, from speech therapists to occupational therapists. Indeed, I know from experience that occupational therapists are further split between those who work solely in a hospital unit and those who work in the community. The two, therefore, have different perspectives. I understand that such a split means that increased representation would be better.
790. What is a fair level of representation? Is it a minimum of two representatives on LCGs, or have you a different preferred figure in mind? Moreover, I am not clear about how you feel about representation of allied health professionals on the regional board. Your submission states that the Committee should, under the reorganisation, note:
“the roles and career prospects of a high number of very experienced and valuable AHP colleagues have been cut in order to make further savings.”
791. I am sure that other Committee members are aware of the demand for therapeutic support. That remains on the increase. Therefore, such a cut seems strange.
792. Mrs Cavan: We have a grave concern that, through the reorganisation, we seem to have lost an entire level of allied health professionals. That presents many difficulties, because those who managed the allied health professions were often, particularly in the smaller professions, allied health professionals who worked in a clinical capacity for part of the time.
793. In the other, larger professions, some managers had the important duties of ensuring that more junior staff were looked after and properly trained, and of maintaining the governance of the systems for which they were responsible. The removal of that layer of management means that that looking-after, the arranging of leave, and so forth, are now the responsibility of people who are specialists in their area and should be at the coalface with patients.
794. We are concerned that to remove a complete layer of management will affect patient care and leave less time for those professionals to carry out clinical work, because all those activities must still be carried out somehow. It is a matter of striking a balance: the management structures should not be overbearing, but they must be able to look after staff needs, including their training needs, and ensure the safety and care of patients.
795. You asked how many representatives we want to have on LCGs. We do not have a specific number in mind, but each new local commissioning group needs an allied health professional. However, underlying structures, from which those professionals can obtain support and advice, are also required.
796. The allied health professions — from radiography to drama and art therapists — are also part of a broad church. Consequently, so that a person striving for good commissioning is not left alone, he or she must have good support from staff with the time to provide it. We do not say that we require one of everything, or that two people should be present; however, we do require a support system.
797. Mr Sullivan: We do not want a situation similar to that which arose in the past, when there were seven commissioning groups, and one AHP representative had to look after two, and in some instances three, groups. Clearly, it was a conflict of interest for that individual to represent more than one commissioning group. Therefore, unlike the previous situation, we want a dedicated AHP representative for each group.
798. Dr Deeny: Next year’s changes to local commissioning are important. Last year, someone from one of the GP magazines rang me about an article and said that, although that commissioning system exists in primary care trusts in England, it does not exist anywhere else. Consequently, if next year’s proposals achieve the expected results — if they do what it says on the tin — and entire communities, including GPs, health professionals, nurses, elected representatives and community representatives, get involved, that will be a unique achievement, and I hope that it works.
799. I could not agree with Liz C more — I shall call Mrs Cavan, Liz C, and Ms McKnight, Liz Mac. [Laughter.] An individual allied health professional or nurse, who might be commissioning for 300,000 people, really does require support.
800. I am delighted that the Allied Health Professions Federation is here, because there was a time when that appeared unlikely, and, given that its members play a vital role throughout the healthcare system, the federation’s attendance is important.
801. You said that adequate resources and financial controls should be devolved to local commissioning groups. I am on the current western LCG, so I must declare an interest. However, if LCGs are to work, will AHP state on the record that, without those financial arrangements, people will become disinterested? I have no doubt about that, and that is my worry. Does AHP agree?
802. Given that the membership of my local commissioning group will have to be renewed next year, I may not be on it. Nevertheless, LCGs might become simple advisory bodies, which could be overruled at a whim by regional boards. They will be required to include representatives from the entire community — professionals of all forms and community representatives — who will all attempt to commission for local requirements. Everything, however, will require a rubber stamp from civil servants in Belfast, and might not be agreed.
803. I believe that such a system would collapse. Do allied health professionals agree with medical, nursing and, indeed, community people that, to be effective for people at a local level, commissioning clout must be backed by adequate finance? Otherwise, we are not interested.
804. Mrs Cavan: The straight answer is yes. We are keen that the local commissioning groups will not just be talking shops; that their role will be clear; that they will know how much they can commission; and that their financial structures will be specified. All of that must be clear in the detail, and, given that, we will support the proposals.
805. Ms McKnight: Allied health professionals have bitter experience of those in advisory posts being listened to, but not acted on.
806. In some of the working-out of healthcare delivery and the development of the structures, we have seen how an advisory capacity limits getting things done. We have seen how advisory posts do not necessarily meet the needs. There should be a financial ability to make decisions and act on them, as opposed to having to go to another level to take that action forward.
807. Dr Deeny: The person who phoned me last year will be watching with interest to see how the local commissioning groups work when they are up and running in Northern Ireland. It may be a model that other countries might follow — if it works.
808. Mr Buchanan: I notice that you support the setting up of a regional agency for health and social wellbeing, alongside the regional health and social care board. You say that that can act as a conduit for best practice and signposting the regional health and social care board and the LCGs. I am concerned that that would be nothing more than another talking shop. I am not convinced that setting up a regional agency alongside the regional health and social care board is a good move. It is currently integrated, and I cannot see why a section cannot be set aside in the regional health and social care board to continue with that practice, rather than set up another regional body alongside the board. What would that regional body do and what would its role be? The Committee has had various meetings about the issue, and I feel that it would be acting only in an advisory role to the board — and that is what you have stated in your submission.
809. Why do you support the setting up of another regional body alongside the social care board? What will its role be, and why is it necessary to split the integrated health system already in place?
810. Mr Sullivan: I take your point about the board and the regional agency. It echoes the comments that our nursing and medical colleagues have made, in that there is a lack of clarity on the roles defined for the different groups in the legislation. We would also like to see more clarity and meat on the bones as to how the different agencies would operate. However, from my perspective, the regional board has a role in the performance management of the Health Service as well as overseeing the commissioning arrangements, and a financial management responsibility for the other HPSS agencies. The regional public health and social wellbeing agency, however, is focused on health promotion and health protection and, therefore, has a different and broader focus. It can act as a catalyst for bringing the other organisations, departments and agencies together to work in a more multidisciplinary way across different departmental boundaries, such as education and social development. The regional agency, because of its social wellbeing aspect, would be much more focused on those aspects of health promotion and health protection
811. I can see a role for a regional body, but I agree that the details of how the different organisations interconnect must be clarified.
812. Mrs Hanna: I take on board your comments about your skills being underused. Is that connected with your lack of representation at the top? You said that performance management was not happening.
813. What about the local commission groups? Have you had discussions with the nurses and GPs about how the partnership would work and whom it would comprise? It would be useful if those discussions were to happen locally. The GPs were not involved previously, but discussions should be happening now. Is that the case?
814. Ms McKnight: Unless we are at the table, AHP are often an afterthought in discussions regarding planning services. At those discussions, a service is considered and developed, up to a point; subsequently, however, someone will realise that to get a patient well, mobile, rehabbed or out of acute care, he or she will require the services of a physiotherapist, occupational therapist and, perhaps, a dietitian. At that stage, someone will tell the AHP that it is required; however, not having been factored in at the start of the process makes it more complicated and difficult.
815. That goes through the whole of the structures. The AHP should be part of the discussion at every level: from planning and delivering services to acute and primary care, and through the different structures for the commissioning and developing of services for patients.
816. Mrs Cavan: Although the GPs were not at the previous commissioning arrangements, the professionals and the members of the community — our users — who were present, worked well together and came up with lots of imaginative ideas. It was wonderful to hear people say that they needed more of a particular service, sharing the small amount of money that there was and benefiting each other.
817. If you are not at the table, people do not remember. In their submissions, the Royal College of Nursing and the British Medical Association said that they wanted to be at the table with their colleagues from social services and nursing or social services and medicine. No malice was intended, but they tend to forget our special role. AHPs can get people out of beds more quickly and prevent people from going into hospital. That is our role, but it is sometimes overlooked. It can be an important factor in the Health Service’s finances, because bed days are expensive, and it is a role that AHP plays well.
818. Nurses or doctors at the table sometimes forget the role of the other professionals who may have those skills ready and willing to help the needs of patients. If we are present, we can remind them and make care better.
819. Mrs Hanna: Have discussions on partnerships with the local commission been facilitated by the Department?
820. Mr Sullivan: It is difficult for that to happen, because the Department does not have the capacity to bring that together. Currently, there is no AHP adviser.
821. Mrs Hanna: It would make sense if that were to happen.
822. Mr Sullivan: We would welcome discussions. Discussions are ongoing between various chief officers in the Department, but we are not at that level; we are not included in those discussions.
823. Ms Cavan: We tend to be forgotten.
824. Mr Sullivan: That is part of the difficulty.
825. The Deputy Chairperson: Thank you for your presentation, and we will talk to the Department and ensure that you are not forgotten. We will see what we can do.
2 October 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Dr Brian Dunn |
British Medical Association (NI) |
826. The Deputy Chairperson (Mrs O’Neill): We will now take evidence from the British Medical Association (NI) (BMA (NI)). I welcome Dr Brian Patterson, chairman of the Northern Ireland council of the British Medical Association; Dr Brian Dunn, chairman of the general practitioners committee; Mr Danny Lambe, deputy secretary of the British Medical Association (NI); and Mr Ivor Whitten, the association’s Assembly and research officer. I invite you to make your presentation. The evidence session will last for approximately 30 minutes.
827. Dr Brian Patterson (British Medical Association (NI)): The British Medical Association (NI) thanks you for the opportunity to attend the Committee. I listened with interest to the evidence from the representatives from the Royal College of Nursing Northern Ireland, and, for the most part, I echo their sentiments. It is interesting that two medical professions fundamentally agree.
828. I shall begin by making a few points on the overall view of the BMA (NI) to the reform of our Health Service. We will then take questions from Committee members and try to answer them as best we can.
829. The BMA (NI) welcomes the Health and Social Care (Reform) Bill as progression of phase two of the review of public administration (RPA), which deals with the reform of health and social care. It has the potential to improve the lives of many people in Northern Ireland. At the outset, I wish to clarify that our reservations are not related to the proposals for structural reform; rather, they are concerns about the function of those structures. However, we in no way wish to impede the Bill’s progress.
830. We also welcome the proposed establishment of a regional health and social care board. The BMA (NI) has long had the policy objective of reducing that which is totally unnecessary, and that includes the four health and social services boards in Northern Ireland. We strongly welcome that proposal. We also support the slimming down of the Department of Health, Social Services and Public Safety. We look forward to the savings that will be made from a reduction in bureaucracy, and to those savings being released into front-line patient care. It is vital that the reduction in bureaucracy produces those savings. Moreover, it is essential that any such savings are visible and audited, and that the Department communicates with health and social-care organisations and other stakeholders on how the savings will be redistributed to front-line patient care. It must a visible and transparent process.
831. The BMA (NI) welcomes, with reservations, the creation of a new regional support services organisation. In response to the proposals in ‘Transformation of Business Services in Health and Social Care — Shared Services’, which was published in 2007, our recommended option was for a single, centralised support service to provide a range of shared services. However, the size and bureaucracy of that support function is a concern. The BMA (NI) hopes that the huge bureaucracy is structured in such a way that it is flat and divisionalised, which is to say that there should be a streamlined hierarchy with only a few managers, as opposed to directorate upon directorate. The provision of any outsourcing of work must be subject to the application of stringent business cases and must be progressed openly and transparently. We have some concerns that such an organisation will be structured in such a way that it will be taken over by the private sector.
832. The establishment of a regional agency for public health and social well-being, as well as the priority given to public health in the new structures, is welcomed in principle. It is vital that the role and functions of public-health doctors are enhanced and backed up by the necessary staffing levels and support. The regional agency will need to interface with the Department, the regional health and social care board, the regional support services organisation and the trusts. It is essential that bureaucracy be minimised in the regional agency and among the other bodies. We are slightly concerned about the lack of clarity on how the organisations will communicate with one other.
833. There should be no clash of functions between the proposed director of public health and the Chief Medical Officer. There must be clarity in their relationship, and in the relationship of the advisory roles of the director of public health and the Chief Medical Officer to the Minister. We would also be concerned were the director of public health not medically qualified. It is quite common for that to be the case in England.
834. The BMA (NI) has concerns about the lack of engagement with public-health doctors by the public-health work-streams project team. The mechanism currently used for transparency and to involve staff does not compare to the mechanism used in the previous consultation process.
835. The mechanism by which people are selected for different work streams is unclear. As a single issue that is perhaps not terribly important; however, constraints have been placed on the ability of the people selected to consult fully with their colleagues. In particular, they have not been allowed to share relevant documentation. That appears to be illogical, as the documentation could probably be obtained through a freedom of information request. It causes much unnecessary suspicion and resentment, and it does not allow for open and transparent working.
836. The BMA welcomes the patient and client council. Its role, personnel, and finance should be effectively resourced, and its local offices should be based in the new trusts, the new LCG areas, or the new local council areas.
837. In turn, those bodies must be more strategic and visionary than reactive, as has previously been the policy. That will require the proper resourcing that we mentioned earlier. The BMA has major concerns about the top-down approach to managing commissioning. From listening to the discussion with the first set of witnesses, I understand that that is a widespread concern. An opportunity will be lost if we create local commissioning groups, but ignore the potential for further development at a community level, at groups of local practices or at individual practices.
838. The BMA strongly believes that any commissioning body that wishes to have a general practitioner involved must have the freedom — as long as they operate within the regional strategic framework — to commission services, and to place or to move contracts. Commissioning is about assessing, prioritising and commissioning according to clinical need. That must be evidence-based, and decisions must be taken by people with the appropriate level of expertise.
839. Our next point will not be popular. The BMA opinion is that elected local representatives should not be included on local commissioning groups. That is no reflection on local councillors; we do not want to minimise the importance of elected local representatives. The BMA fully supports the principle of local commissioning groups and local government working closely together on local health improvement plans.
840. Furthermore, we are realists, and recognise that our wishes will not be fulfilled. However, we will be keen to ensure that that works effectively.
841. If elected council representatives are on LCGs, the scrutiny and accountability of local councils may be eroded. The practicality of having four local representatives on each LCG is a concern. For instance, in the Northern Health and Social Care Trust area, the proposed community group will cover eight current local government areas.
842. The BMA has consistently called for more powers for local councils, especially with regard to well-being and community planning. That is essential if local councils are to engage with multiple stakeholders in planning healthier spaces for ratepayers. It would be difficult if local councillors were to commission services which they would then be required to scrutinise. The scrutiny role is more important. Historically, lack of scrutiny is an area where the Health Service has fallen down.
843. Thank you very much. We are happy to answer member’s questions.
844. The Deputy Chairperson: Thank you very much for your presentation. Tommy, do you want to start?
845. Mr Gallagher: Thank you for your presentation. I return to the issue about the lack of shared information in work streams. Elected representatives have found that, under RPA, in the case of local government, it has been felt that the Department has not shared information with the elected representatives who will be involved in the new set-up.
846. I presume, therefore, that the Department is also the body that is not sharing with the professionals information about all that is happening in those work streams. Is that the case?
847. Dr Patterson: The situation is even more complicated than not sharing — the difficulty is that it prohibits those who have the information from sharing it with their colleagues.
848. Mr Gallagher: Did the Department impose that restriction?
849. Dr Patterson: Fundamentally, yes, because they are the only people at present who have the information. There is little enough information available on which we can comment, but we would like to see whatever information there is to make an informed comment rather than have to fight and use legislation to get information. If the process is open and transparent — and it is hardly the Official Secrets Act — why are we not seeing that information?
850. Ms S Ramsey: When I was growing up, there was an advertisement on the television saying that one does not need a pill for every ill. I agree entirely with that.
851. Your submission states that local commissioning groups should be led from the local community upwards, that iii should not be a top-down approach, but a bottom-up approach. I agree with you totally in that respect. Therefore, I am slightly concerned at your point about elected local representatives.
852. I am not now a local councillor, but I was one for a long time. The Bill aims to achieve a holistic approach to health and social services to ensure that Departments other than Health, Social Security and Public Services play their part, whether in education, sport and leisure or on local councils. How does that fit with your view on elected local representatives? They are probably the only ones — especially at local council level — who have a holistic approach to the community’s needs, especially when councillors have grown up, live and work in that area. You need to be careful on that, which brings me back to my original point that it is not always a pill for every ill.
853. Medical practitioners, for whom I have a great deal of time and respect, do not always have the right answers. The challenge to treating heart disease or obesity could, for example, be to provide more leisure facilities. Therefore, if this Bill is to be a root-and-branch change in the approach to community health inequalities, the BMA, which is probably one of the larger medical unions, must be careful.
854. Dr Patterson: Do not get us wrong: we do not suggest that the local commissioning groups should be composed entirely of professionals, and that there is no place for community representation. That is not what we are saying. Four seats are allocated for local councils, and that could cause a problem with regard to scrutiny. That is our objection. However, that is not to say that those four seats could not be filled by other lay people from the community, empowered through various bodies. There is another way of approaching the issue which preserves the right of councils to provide firm scrutiny.
855. Dr Brian Dunn (British Medical Association (NI)): Commissioning is not a democratic process — it is not about voting whether somebody should have this or somebody should have that. The BMA(NI) believes that the political decisions are taken by the Minister, the Assembly, and the local commissioning groups. Hopefully, smaller groups below that would work within that overall strategy.
856. I am a GP. I live in, and am involved with, my community, and I am chairman of various organisations. I recognise that the local council has a big role to play. Living as they do in the community, GPs live with their mistakes as well as their successes, and that makes them human.
857. I do not think that I am infallible; I know my fallibilities. I am happy to work with other people to improve the health of the community. The Minister’s document does not recognise what true commissioning is. Northern Ireland has not had true commissioning. Boards have given huge sums of money to trusts, assuming that the volume of service will be the same as the previous year. Whether the trust either delivers or does not, in the next year, it receives the same volume of money plus an uplift.
858. Proper commissioning, as we envisage it, involves groups of practices coming together to assess the needs of their community and considering how the service is provided. It involves assessing whether there is a more efficient way of providing the service, holding the trust to account for what it does provide and cutting out inefficiencies, such as unnecessary outpatient appointments and considering drug budgets. For instance, it should look at practices having the same drug formulary as the hospital. Sometimes, patients go into hospitals on one tablet and come out on a different one just because the hospital does not use that tablet. Huge efficiencies can be made, but those efficiencies can only be made by professionals if they are fully engaged in the process.
859. Ms S Ramsey: We are not disagreeing, but a more proactive approach is needed when commissioning and local knowledge and information is considered. For example, my constituency of West Belfast had a high level of asthma for several years. People were being given the medication to deal with asthma, but no one was dealing with the Housing Executive to get rid of the cause. Local elected representatives are crucial for finding out information, and a proactive approach is required that recognises that a pill for every ill is not necessary.
860. Dr Dunn: We agree entirely with that. As doctors, we realise that the improvement in health in these islands has not come about because of better medicine. We recognise that it has come about because of better diet and better social conditions. We do not see the LCGs not working with the local councils. Local elected representatives must work closely together with the LCGs, not only to treat illness but to prevent illness and improve the health of the community. We both want the same outcome, but my perspective is slightly different from yours and that of the Minister.
861. The Deputy Chairperson: Agree to disagree.
862. Mr Easton: Thank you for your presentation. You mentioned that local councillors might not be on the local commissioning groups. Slightly before that, you suggested that another layer below that might be created that would include local representation. Can you explain more about that?
863. Dr Dunn: The Woodward proposals, the Goggins proposals and the Sissling proposals envisaged a local commissioning group. Under that, they envisaged groups of practices who use the same provider, which cover perhaps up to 50,000 patients, coming together to consider the needs of their community and how the provider was providing those needs. They envisaged that those groups would have the ability to have a devolved budget, and, if necessary, the ability to move the budget to another provider to improve the health of their community.
864. GPs did that, and fundholding was not universally popular, but the reason that fundholding patients got a better service than non-fundholding patients was not because extra money was spent on them. They got a better service because of better commissioning by the GPs.
865. For example, a fundholding practice with a practice on the Antrim coast was an isolated, single-handed practice that had a laboratory service collection twice a week. When fundholding ended, the GP had a laboratory collection twice a day, in-house physiotherapy, in-house podiatry and other services. His patients benefited, without any extra money being spent on them, and that is the way that we see services should be provided.
866. Ninety per cent of our budget is spent on hospitals, and, by increasing the efficiency and improving the service to local communities, money could be saved without sacking people or making people work harder. A year or two ago, GPs were up for that type of system, but they have become more and more cynical as delays have gone on, and they think that it will never be implemented. Our big problem will be in motivating GPs to join LCGs.
867. Dr Patterson: We do not advocate a one-size-fits-all approach. However, where local need exists, it seems strange to call it local commissioning when populations of 300,000 are involved. Most of us are familiar with practices with approximately 7,000, 11,000 or 15,000 patients. Issues in our Health Service could be sorted out at that lower level, and, although the Bill does not deny that possibility, why has the proposal changed significantly since the previous proposal? It is silent. When I explore the proposal, I am told that there is an option for local commissioning groups to suggest a lower figure. Our health boards have had many options over the years, which they have chosen not to exercise. It is difficult for large organisations to recommend smaller bodies to carry out particular tasks. There are areas in our country where local need could be addressed through smaller areas of commissioning, rather than populations of 300,000.
868. Mr Gardiner: Thank you for your presentation. I am disappointed and do not accept item 12, which refers to locally elected representatives. I declare an interest; I have been an alderman in Craigavon Borough Council for many years. I do not agree with your sentiments about locally elected representatives on this new body. Local representatives have their feet on the ground. Doctors work their hours and, afterwards, are free to play golf or go sailing. Councillors and MLAs are on call around the clock. We communicate with the public, and the public know who represents them. Therefore, I do not accept that point and your presentation is, perhaps, damned by its inclusion. I do not support you on that matter.
869. Dr Patterson: As I said during the presentation, we know that we are out on a limb on that matter. I tried to argue that the reason is not about —
870. Mr Gardiner: Why not be sensible about it?
871. Dr Patterson: I think that we will be compelled to be.
872. Mr Gardiner: You had better change your tune.
873. Dr Deeny: I disagree with Mr Gardiner. Like Brian Patterson and Brian Dunn, I am well known in the community, and I do out-of-hours GP duties.
874. Mr Gardiner: But you are a public representative.
875. Dr Deeny: That is true. My questions have, mainly, been covered. I agree with Brian Patterson that 1·7 million people spread across five local commissioning groups — amounting to over 300,000 in each area — does not constitute local commissioning. That is a concern. The Committee should consider that point.
876. The previous proposal was for the community care associations, and they covered areas of, roughly, 50,000 people each. That is local commissioning. As a GP, an elected representative and a member of community, I know that people consider 300,000 too large. We must consider reducing that figure to approximately 50,000. Our practice has over 8,000 patients, and we could amalgamate with other local practices that are aware of their specific local needs. How can the Committee address that matter — as I believe we should — to secure local commissioning and meet local health needs?
877. I accept Sue’s point, and accept the point made by the BMA; there must be a close link with councillors. Indeed, I have no problem with councillors’ being represented, because leisure centres and other facilities are involved in healthcare. Councillors are in touch with local needs in that area. How can the Committee’s response to the Department consider local need, rather than allow a regional board with five local commissioning groups to deal with more than 300,000 patients?
878. My second question is about the problems the BMA may have in communicating with the various bodies that you mentioned at the beginning. Again, I ask for your suggestions or solutions: how should communications take place between the new bodies proposed for next year?
879. Dr Patterson: To answer your second question, it is obvious that communication must be effective without involving a huge bureaucratic machine. Our major concern is that this proposal is silent on how the bodies will communicate. There is silence in other areas, for example, the number of seats available on these bodies and the persons likely to fill them. Silence always raises suspicion. I can live with it when someone states his position, and then one can argue for or against it; but silence implies a plan that we have not yet been told about. My worry is that communication must be effective, therefore people must be accountable for it. There is no need for a huge, complex machine, in which it is obvious that no one will be accountable when communications go wrong.
880. We have had a long history of being given the runaround. We speak to a trust, which tells us that the board that commissioned it is responsible; we go to that board, which says that, though it is commissioning, the trusts are not acting and the Department will not let the board do anything about it. We have spent light years running round in that circle, and we never succeed in getting the three in one room. My fear is that these bodies will act in the same way. To make communication effective, someone must be accountable for it, and we should not have to chase up 17 different culs-de-sac. To keep it simple, structuring communications is all about accountability.
881. There is something else you can do to ensure that there will be commissioning at a lower level. I am assured that what is on the table does not preclude that; however, I want firmer assurance. I want to know that it will be encouraged. With populations of 300,000, the question must be asked: are the LCGs are so very different from health boards? We may simply be moving from four health boards to five. The needs of local people are vital. We differ, in some respects, as to how those needs will be communicated, but that can be resolved. The important thing is that the ability to address those needs is definitely — not just potentially — present.
882. Dr Dunn: Regarding accountability, there was an instance recently where a board wanted to do something, but the trust said no. The board replied that it was the commissioner; the trust responded by claiming that it was not accountable to the board, but to the Department.
883. The new arrangements must ensure that the provider will be accountable to the commissioning body, rather than to the Department or anything else.
884. I must prolong the argument on elected representatives: I pushed that fairly hard in the BMA. In my community, I am a GP and an elected councillor. I know the rules of councillors, and what councillors will bring to LCGs is only peripheral and could be worked out in a meeting between the LCG and the local council. Commissioning will be about who will receive breast cancer drugs, dialysis, to where heart disease should be referred, how asthma should be treated. There are items around the periphery that will be of interest to elected local councils, but a co-ordinating committee could sort those out. There is no need to have councillors there, making decisions that, at times, will be very unpopular. However, as the Deputy Chairperson has said, I am sure that we will agree to differ.
885. Ms S Ramsey: Councillors will be the only independent element; they alone will have no agenda to push.
886. Dr Dunn: We see GPs as independent.
887. Ms S Ramsey: We’ll beg to differ on that as well. This issue is also about protection. Councillors are the only ones who are independent. The BMA — [Inaudible.]
888. Dr Deeny: Just on the back of that —
889. The Deputy Chairperson: If there is time at the end, I will return to Dr Deeny. Carmel is next.
890. Mrs Hanna: Good afternoon, gentlemen, and welcome. I take on board the point that has been made and I am concerned to ensure that savings from a reduced bureaucracy are directed towards front-line services. However, those savings must be subjected to proper accounting and auditing procedures; otherwise it will not be possible to assess their benefits. My biggest concern is how the bodies relate to each other with regard to their partnership, decision making, top-down and bottom-up relationships, where they meet in the middle, and how well they communicate.
891. The witnesses say they are concerned about the large scale of the regional support services organisation. It is so big that I wonder what it will do. It will not want to commission other services that can be obtained in-house. In a previous submission to the Committee, the Child Support Agency (CSA) stated that it was concerned about the impact on it of being subsumed into another body.
892. I am also concerned that not enough consultation has taken place with public health doctors through the Institute of Public Health. A serious effort to create a new public health body requires a lot more public consultation.
893. How do you envisage the make-up of a commissioning body? What decision-making role will its members have? Will there be a partnership role for GPs and other health professionals? I am not hung up on the number of councillors that may be involved, but in principle I support a councillor being appointed. If their role is regarded as peripheral, there is no reason why there cannot be capacity-building with councillors. There is no reason that councillors should not have a far more meaningful role.
894. I want to hear more about the proposed breakdown of that commissioning body and how to ensure that it will be a real partnership that will incorporate health professionals and others in the decision-making process. Mention has been made of Dr Brian Dean’s comments on the efficiency savings that doctors might bring to the body. If that is not happening already, surely it should be, partly as a result of a reduction in prescribing and generic drugs. Problems like clostridium difficile have informed the public about ongoing problems associated with the overuse of antibiotics.
895. I want to see commissioning groups made even more local, but there must be a real partnership in both the membership and the decision-making process.
896. Dr Dunn: I emphasise that GPs are not seeking power. As a GP myself, the only thing I want from the secondary sector is that my patients are seen and treated or operated on as soon as possible. I have no other agenda.
897. Adopting a central direction approach will not lead to savings. Generic drugs, for example, are always trumpeted as the saviour of prescribing budgets.
898. Mrs Hanna: That was just an example.
899. Dr Dunn: At any time, 30% of generic drugs are more expensive than the branded equivalent. Sometimes generic drugs are cheaper, at other times they are a lot more expensive. Reorganisation alone will not create savings. Like most reorganisations, this one will result in bureaucrats generating more bureaucracy. Therefore, savings accrued through reorganisation will be small.
900. Savings can be made by involving the practices. I want to emphasise that savings can be made by getting practices to sit down together — which involves extra unpaid work for GPs — to establish how to get more people through the health care system for the same amount of money. That involves considering referral patterns and talking to trusts about how to provide better services through increasing the number of new appointments, and reducing the number of review appointments by having those looked after by GPs rather than by hospitals.
901. I am passionate about this because it can work, and I want to see it work. It must be more radical than rearranging the deckchairs on the Titanic and declaring that everything will be OK. Trusts must provide what they are paid to provide, rather than being given huge sums of money in the hope that they do.
902. Mrs Hanna: I agree. However, all other health professionals must do exactly the same in their roles.
903. Dr Dunn: Absolutely.
904. Mrs Hanna: Therefore, my question is more about the breakdown of that partnership.
905. Dr Dunn: We envisage that locality commissioning will involve GPs, nurses and other health professionals working with people in the local community, assessing local needs, and deciding how best to meet those needs. There is no question of GPs dictating what happens. It is just that GPs hold patients’ medical records and are responsible for approximately 90% of referrals to the secondary sector. That is the only reason that GPs feel best placed to perform that function. GPs want to work with people, not boss them or tell them how things should be done.
906. Mrs Hanna: I take your point on that. We have been so concerned about making the decision-making role right in the two main bodies, but it is equally important that we are aware of how it works — right down to that level — and that we know the detail.
907. Dr Patterson: That partnership happens day and daily on the ground. When we look at the proposals, we see that there is huge potential for that partnership to flourish. In the past, people always said that that is what should happen. However, they placed so many obstacles in the way that they prevented it from happening, and we are concerned that such a situation will reoccur. They do not want that to happen at a local level, because a local level is much more effective but less controlled. This is about top-down control rather than about genuinely assessing and meeting need from the bottom up.
908. On the issue of savings, and the visibility of those savings, we have gone through phase one of the RPA for two years. Are you impressed by the level of savings resulting from the reorganisation of the trusts? I do not think that there have been any savings.
909. Mrs Hanna: The concern was always that no savings would really be made. We want to ensure that the reform of health and social care works and provide a better service for patients. We are hopeful that there will be savings in future and, if there are, that they will be visible.
910. Mrs McGill: I declare an interest as a district councillor. I do not wish to labour the point, but it would be remiss of me, as a district councillor, not to comment. Your submission demonstrates your strong opposition to local councillors sitting on local commissioning groups (LCGs). As you have declared that you are a councillor yourself, Dr Dunn, I wonder whether that opposition is a result of your personal experience of councillors. It may not be the same across the entire North —
911. Ms S Ramsey: Which means that you are not a good councillor. [Laughter.]
912. Mrs McGill: My colleague Sue Ramsey said that councillors bridge the gap between some bodies. Furthermore, you made referred repeatedly to the threat of increasing bureaucracy. I feel that councillors often do a good job in highlighting such bureaucracy.
913. My question concerns the transfer of the Mental Health Commission to the Regulation and Quality Improvement Authority (RQIA). Do you have any comment to make on that issue?
914. Dr Patterson: We have commented on that in our documentation.
915. Mrs McGill: I only require a brief answer. If you have not got the information with you, you can respond to me at a later date.
916. Dr Patterson: We are all aware of the situation surrounding mental-health services in the Province. We see the RQIA as having a huge role to play in the development of mental-health services. However, to place that body in such a position is a little like the previously mentioned scrutiny issue. How can that body scrutinise something for which it is responsible? That is our argument.
917. Mr Ivor Whitten (British Medical Association (NI)): The transfer of the Mental Health Commission to the RQIA is somewhat problematic, mainly as a result of staffing and training issues. The RQIA is already stretched, and the absorption of that extra responsibility will mean that it will be further stretched. We are not necessarily against the idea, but our real concern is whether the RQIA will be able to take on the extra responsibility. It is a very sensitive area, which must be properly resourced.
918. Dr Deeny: I am not going to ask what you think I am going to ask. [Laughter.] I wish make a point as a GP. Many people say that 300,000 people being cared for by a single LCG is too high a number. I feel strongly about that, and I wish to stress that fact to my fellow Committee members.
919. The Western Health and Social Care Trust provides healthcare for a population of almost 300,000 — I believe that 297,000 is the exact figure. That trust encompasses quite a large area, and the people’s health needs in that region are differ greatly. For example, the needs of those living in Derry city are different to those living in rural Fermanagh or Tyrone.
920. Given that the LCGs will be commissioning, it is important that Committee members take that point on board. It may be argued that it is fine for a LCG to cover a population of 300,000 in Belfast because everyone there has the same needs, but we all know that that is not the case. People living in different areas of Belfast have different needs.
921. We must consider seriously the proposal to bring the population covered by a LCG down to approximately 50,000. For example, my patients’ needs differ from those of patients in the Creggan estate in Derry. It is important that we take that on board, and I ask Committee members to consider it.
922. I was not asking a question; I just wanted to make the point that 300,000 patients are too many for a single LCG. The needs of the people in the west are different from those of the people in Belfast, and, similarly, the needs of the people in south Belfast are different from those of the people in north Belfast.
923. Ms S Ramsey: We could make a note to consider that during clause-by-clause scrutiny of the Bill.
924. Dr Deeny: As Brian Dunn mentioned, GPs, primary-care professionals and community representatives are prepared to make an input to the LCGs at no cost.
925. Ms S Ramsey: May I ask a question that may not be popular with the BMA? It does not annoy me to be unpopular. Please explain to me, as if I were a two-year-old, how the commissioning system will work. For example, if GPs are in control of the commissioning service and 90% of Brian Patterson’s patients have asthma and 90% of Brian Dunn’s suffer from allergies, who commissions for which patients? The commissioning process will be subject to a budget, so if Brian Patterson makes a stronger argument to the commissioning group, will his patients receive the treatment that they need ahead of Brian Dunn’s patients?
926. Dr Dunn: Budget setting is much more sensitive when performed at a local level. It will not be the case that a decision will be made to buy X number of drugs, which is what happens at present. Currently, the Eastern Heath and Social Services Board allocates approximately £1 billion to Belfast Heath and Social Care Trust each year. That body then requests a volume of drugs, but frequently that is not delivered. With a local commissioning system, doctors will know how many patients suffer from asthma, allergies or heart disease, for example. The doctors in the LCG will then get together and calculate the total number of patients with different conditions in that group, and they will place their contract accordingly. In that way, the contract will be much more sensitive to the local need.
927. Ms S Ramsey: I do not want to criticise, because I have a very good GP, whom I hope is listening to this. [Laughter.] However, rightly or wrongly, GPs will want to fight for the rights of their patients and will not consider people who are not their patients — the only people who will do that are those who are independent. The only people who are totally independent are elected representatives.
928. Dr Patterson: Certainly, a huge issue exists and it relates to Carmel’s point about partnership. It should not be only GPs who are determining how the system operates. GPs have a valuable input to make, as was shown when they did not participate in the local health and social care groups (LHSCGs), but that was because that scheme was doomed to failure. We do not want the LCGs to be doomed to failure. We suspect that the scheme is being manoeuvred into an LHSCG mode, and we are relying on the Committee to prevent that happening, during its clause-by-clause scrutiny. The LCG scheme is about getting everyone with an interest involved. I am not particularly hung up on people’s disciplines or professions because I recognise that a variety of people will have a legitimate interest.
929. The new scheme will be much more sensitive to the needs of individual patients if it is operated at a level of 50,000 patients or fewer, rather than at a level of 300,000 patients. The scheme should not focus solely on doctors. Doctors have a role to play and, as the Committee heard earlier, nurses have a role, as do pharmacists, dentists, and opticians, and those roles are vital. It is all about communication. Communication at a genuinely local level will produce better outcomes for patients than communication in some lofty chamber.
930. Dr Dunn: We are not particularly concerned about what form the bodies will take; we are concerned about their function. We want to see them as effective commissioners; otherwise, there will be a secondary-care-led service. That kind of service has created the waiting lists that now exist. We must have a service that considers what the patients in the community need and delivers on those needs, rather than delivering what the secondary-care service wants to provide, which is sometimes the case.
931. The Deputy Chairperson: That brings our evidence session to a close. Thank you very much for coming along and presenting your views, even those that were unpopular. [Laughter.]
2 October 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Mr Craig Allen |
Department of Health, Social Services and Public Safety |
932. The Deputy Chairperson (Mrs O’Neill): The Committee will now begin its clause-by-clause scrutiny of the Health and Social Care (Reform) Bill. I welcome Ivan McMaster, Bernard Mitchell and Craig Allen, who are here to give meaning to each clause, provide clarification, and to answer any questions. At the Committee meeting on 11 September, information was distributed, including a copy of the Bill, explanatory notes, submissions for the Committee’s consultation, together with a table that brings together comments received by the Committee in relation to each clause.
933. The Committee has a number of options in relation to each clause. Before choosing an option, I will invite officials to outline briefly the purpose and meaning of the clause. Members may wish to seek clarification about the clause as we proceed. Members will take account of the views expressed in the written submissions and the oral evidence. Following discussions with the officials on each clause, the Committee must decide if it is content with the clause as drafted, or, agree the potential for amendment, in which case the Department must be requested to consider its position and report to the Committee. Where amendment is considered appropriate, the Committee must then invite the Department to indicate whether it is willing to undertake the drafting of such an amendment. By choosing that option, we effectively defer the consideration of the clause.
934. I invite the officials to outline the meaning of the clause and then we will take members’ questions.
935. Mr Ivan McMaster (Department of Health, Social Services and Public Safety): I will set this out for you as briefly as I can. Clause 1 deals with the generality of the restructuring of the organisations. That is dealt with at the beginning of the Bill in an attempt to aid the reader, set out the bodies that are to be dissolved, the names and acronyms used, and, hopefully, get those things out of the way. Subsection (1) deals with the four bodies that are to be dissolved. Those bodies were created by primary legislation and therefore, have to be dissolved by a similar means. Two special agencies — the Health Promotion Agency and the Regional Medical Physics Agency — are also being dissolved; however; those were set up under subordinate legislation and will be similarly dissolved. The subordinate legislation dealing with those two bodies will come before the Committee at some stage later in the process. Fur the purposes of this Bill, the four bodies that will be dissolved are those listed in clause 1.
936. Subsection (2) provides for a change in name for a number of bodies. The Regulation and Improvement Authority was established in 2003, and the Order that established the authority said that it should be known as such. In practice, however, the organisation has always been referred to as the Regulation and Quality Improvement Authority. “Quality” is clearly part of its remit, and the opportunity has now been taken to regularise that situation and legally amend the title to its commonly referred name.
937. Moreover, health and social services trusts are now to be known as health and social care trusts. That reflects recent thinking that the term “and personal social services” should be replaced with the term “social care”. Indeed, some Committee members may be aware that, since they were established in April 2007, the new trusts have been branded as health and social care trusts. However, strictly speaking and legally, they are still health and social services trusts, so the opportunity has now been taken to regularise that matter as well. Similarly, to provide some uniformity, the special health and social services agencies are to be called special health and social care agencies.
938. Finally, clause 1(5) gives a definition of health and social care bodies. Its purpose is simply to list those bodies that are being referred to when the term “health and social care bodies” is used in the Bill — that includes the bodies that are being created, as well as the special agencies, the RQIA and the trusts. It provides a generic phrase, and when the Bill refers to a health and social-care body that is not one of those listed in this subsection it will say so. Essentially, when the term “health and social care bodies” is used, it refers to all those bodies listed under subsection (5).
939. The Deputy Chairperson: In the previous evidence session, we heard from representatives of the allied health professions. I am not sure whether this issue is directly relevant to clause 1, but they mentioned their concerns about representation and support services for allied health professionals in the Department. Is that issue in any way relevant to clause 1, or is the Department considering it at a different level?
940. Mr Bernard Mitchell (Department of Health, Social Services and Public Safety): I do not believe that it is; I think that that is a separate issue.
941. Ms S Ramsey: I know that we are starting clause-by-clause scrutiny, but I have a general question to ask. The proposals in the Bill were put out to consultation, and many general responses were received. In the light of those consultation responses, does the Department or the Minister have any proposed amendments to the Bill? Sometimes, a Committee can do a great deal of work on a Bill only to arrive at the same conclusion as the Minister. Therefore, it may be useful to know whether the Minister has any proposed amendments as a result of the consultation.
942. Mr Mitchell: There is none at this point.
943. Mr McMaster: As we go through the Bill, I will draw members’ attention to a couple of proposed amendments, but they are to amend printing errors and the like. However, no substantive amendments have been proposed at this stage. When we come to the relevant clauses, we will point out the changes that will have to be made. For example, in one instance, there is a reference to the “regional agency” rather than to the “regional board”. That is simply a printing mistake, or a mistake on our part. We will bring those proposed amendments to the Committee’s attention when we reach the relevant clause, if that is OK. However, there are no proposed amendments to this particular clause.
944. Mr Gardiner: Clause 1(2)(a) and (b) will rename the Northern Ireland Health and Personal Social Services Regulation and Improvement Authority the Health and Social Care Regulation and Quality Improvement Authority, and states that it will thereafter be referred to as the RQIA. Anyone who reads the Bill will be misled by references to the RQIA — they will not know what it means if the term “Health and Social Care” is removed from its title. The organisation’s role hinges on health and social care, yet the Bill refers to it only as the “RQIA”.
945. Mr Mitchell: Do you propose that the term should be prefaced by the words “Health and Social Care”?
946. Mr Gardiner: Yes, it should be spelt out properly.
947. Mr Buchanan: Clause 1(5)(b) states:
“the Regional Agency for Public Health and Social Well-being, established under section 12 and referred to in this Act as ‘RAPHSW’;”.
I am not convinced that that body should be set up. I do not really see the need for it, and I will be proposing an amendment to say that we are not convinced that such a body should be set up.
948. Mr Mitchell: It would be fair to say that, in the consultation responses, several respondents raised the issue of the respective roles and responsibilities of the proposed regional agency and regional board. They stressed the importance of being clear about the nature of those relationships. They felt that the lines of accountability and responsibility for the two bodies should be clear, and that they should work to a common agenda.
949. It is also fair to say that there was significant support for the concept of a regional agency, on the grounds that it was seen to offer a tangible sign of an intention to bring a renewed focus to the issue of public health and social well-being. Many people responded positively to the proposal from that perspective, and they felt that it was an issue that had to be addressed. They wanted a focus on health inequalities.
950. Mr Buchanan: That may be so, but to me, it is another body that has been set up to consult or to give guidance to the regional board. I do not see the need for it. It is another layer that will have to be paid for out of the health budget. The issues that it would be set up to address could be dealt with by the regional board.
951. The Deputy Chairperson: Clause 1(5) merely describes the organisations that comprise the health and social care bodies, Thomas. Clause 12(1) establishes the regional agency. Your argument may be more valid when we get to clause 12.
952. Mr Buchanan: I am simply putting a marker down today. I do not feel that there is a need for a regional agency.
953. Mr McMaster: Clause 12 establishes the regional agency. Clause 12(1) states:
“There shall be a body corporate”.
Clause 1 sets out the definition of the regional agency and provides an acronym for it. If it is subsequently decided that the regional agency should not be created under clause 12, the reference to it in clause will be also be removed.
954. Mr Gallagher: It is worth noting that we have already approved a clause, as Tom is aware, that dissolves the health and social services boards. This is a proposal, as part of a process of rationalisation, for a single board to replace the four boards that are to be dissolved. Is that correct?
955. Mr McMaster: That is correct.
956. The Deputy Chairperson: Are you happy enough to leave the matter until we get to clause 12, Thomas?
957. Mr Buchanan: That is fair enough, but I have put a marker down. I am not happy with such a body’s being set up.
958. Mr Mitchell: Chairperson, are you content that we do not respond further to that issue today?
959. The Deputy Chairperson: I think so, yes. The Committee must decide whether it wants more time to consider that position or wants to agree the clause as it stands.
960. Mrs McGill: There are concerns about the setting-up of the regional agency. We have had a presentation from one set of witnesses in particular. Those witnesses articulated their concerns about the increase in bureaucracy that the legislation will create. Your suggestion, Chairperson, that we seek clarification on the nature of the regional agency and obtain some more information may be valuable at this stage. We should all be clear —
961. The Deputy Chairperson: Are you suggesting that the officials should try to explain the situation or that we should refer the clause for further consideration?
962. Mrs McGill: I am listening to Tom’s concerns and to what the officials have said about returning with some more information. I am not clear about the process. If we agree clause 1, does it just go ahead? One member has said that he has put down a marker. It may be valuable to know exactly what added value the regional agency will give to the structures.
963. I remember that, shortly after I became a member of the Committee, I raised some concerns about the number of proposed new bodies. We have already heard today some concerns about the linkages between them and about each body’s particular authority. I agree with the concerns that have been expressed.
964. The Deputy Chairperson: I fully understand your point, but clause 12 deals with the establishment of a regional agency for public health and social well-being. When addressing that clause we will have the opportunity to fully debate the ins and outs of how that agency will operate in practice.
965. Mr Gallagher: All the groups that gave evidence in Committee this afternoon supported the establishment of one regional health and social care board to replace the four current health and social services boards. It seems to me that the Bill will enact the measures that those witnesses supported. None of those groups questioned the establishment of single regional board. That has not been raised as an issue in any of the submissions that have been made to the Committee.
966. Ms S Ramsey: Claire McGill and Thomas Buchanan make a valid point. I partly agree with Tommy Gallagher, in that no one involved in the consultation has opposed the establishment of a regional board, but, in reading the Bill, it seems as if it abolishes the four health and social services boards but establishes three more organisations. Claire’s point is that more information is needed, because, although the Bill appears to abolish the four boards and establish one regional board, it also establishes a regional agency for public health and social well-being and a regional support services organisation (RSSO).
967. Mrs Hanna: Tom Buchanan’s proposal is a radical shift from the course that we have been taking so far, and it almost represents a return to the drawing board. We all have concerns about how the new bodies will work together, but we have been expressing those concerns all along. We have never said that any of those bodies should not be established; we merely queried the methods of communication among them and where the decisions would be taken, and we sought to ensure that the new bodies would not be top-heavy. We received no clarification, so this is probably the first time that anyone has questioned the number of bodies. If we are to discuss a reduction in the number of bodies to be established under the legislation, that is a bit like going back to the drawing board.
968. It is not that we should not discuss the number of bodies, but it has not been mentioned before. Several issues concerning the bodies have been discussed, but no one has questioned the need for any of the bodies, except, perhaps, for the RSSO, which will subsume the Central Services Agency. We heard about concerns around that at a late stage. However, it represents a shift if we are now to question whether one or more of the elements should be removed. As I said, it is a bit like going back to the drawing board.
969. Mr Buchanan: With respect, it is not a shift. If you remember, I raised the issue in the House during the Bill’s Second Stage. I stated then that I did not see the need for the establishment of a regional agency alongside a regional board, and the Minister responded to my concerns. It is not a new issue. It may be the first time that it has received open discussion in Committee, but it is something that I have raised in the House prior to today’s meeting.
970. Mr Mitchell: Some very strong arguments exist in support of the creation and development of the regional agency. We welcome the chance to explore those with the Committee, and to go through the arguments in detail. We are quite happy to address the points that have been made about duplication and value for money — we can answer them. We are content to return and discuss those issues, and we shall bring some public-health expertise with us to try to inform that discussion.
971. The Deputy Chairperson: Are you suggesting that we refer clause 1 for further consideration and return to it at a later date?
972. Mr Mitchell: We can address those points when we come to discuss clause 12, which if amended, as my colleague has said, would alter clause 1.
973. Mr McMaster: When we come to clause 12, which proposes the establishment of the regional agency for public health and social well-being, the Committee will either vote on whether the clause should be agreed to or propose an amendment to it. If the Committee proposes an amendment to clause 12, it must also propose to an amendment to clause 1. In other words, if we decide not to set up the regional agency, the reference to it in clause 1(5)(b) must be removed. That is based on the assumption that every other clause will be accepted. However, if the Committee agrees that a clause should be agreed to, it will be withdrawn.
974. Clause 1 provides some clarification about the organisations that will be dissolved and details the names of the new health and social-care bodies.
975. Mrs McGill: I understand Carmel’s point that what Tom Buchanan suggests represents a complete change and that we are going back to the drawing board. However, that is not my position. Some concern was expressed about the establishment of a regional agency. When Mr Mitchell said that he will return with further information, I said that that will be valuable. That remains my position.
976. Mrs Hanna: When I said “back to the drawing board”, I meant that we as a Committee must have further discussions on the issue. The issue may have been raised at Second Stage, but it was not raised in Committee until now.
977. Mr McMaster: Clause 2 sets out the Department’s overarching duty for the provision of health and social care in Northern Ireland, as well some specific requirements.
978. The clause largely replicates article 4 of the Health and Personal Social Services (Northern Ireland) Order 1972, which states that the Ministry of the time had an overall and overarching duty for the provision of health and social services. However, given that the Bill is designed to provide a clear narrative of the major review of structures, it was considered that the Department’s overarching duties should be restated in the Health and Social care (Reform) Bill. There were concerns that it was not enough to spell out the Department’s overarching duty in high-level terms.
979. Clause 2(3)(a), therefore, provides some further detail about the Department’s overarching duties. It is the first time that the Department’s unavoidable requirements have been placed on statue.
980. It states that Department must:
“develop policies to secure the improvement of the health and social well-being of, and to reduce health inequalities between, people in Northern Ireland;”.
If the Department does not adhere to those requirements, someone could question its actions and say that it was in breach of its statutory requirements. That is the first time that that requirement has been spelt out in legislation. However, the duties listed should not be regarded as exclusive.
981. Clause 2(3) begins: “In particular, the Department must—”. The requirements that follow are areas of high-level focus. However, that does not mean that the Department cannot perform other duties.
982. Clause 2(3)(h) specifies that the Department must:
“monitor and hold to account the Regional Board, RAPHSW, RSSO and HSC trusts in the discharge of their functions;”.
983. Clause 2(3)(i) provides that the Department must:
“make and maintain effective arrangements to secure the monitoring and holding to account of the other health and social care bodies in the discharge of their functions;”,
984. because some of them are also held to account by other bodies.
985. Clause 2(3)(c) outlines the Department’s duty to:
“allocate financial resources available for health and social care, having regard to the need to use such resources in the most economic, efficient, and effective way;”.
986. The clauses place firm, clear duties on the Department.
987. Clause 2(4) states:
“The Department shall discharge its duty under this section so as to secure the effective co-ordination of health and social care.”
The clause ensures that health and social care go together. We cannot distinguish between those two issues; they are inextricably linked. The clause makes provision for effective co-ordination because it is an important issue.
988. The Deputy Chairperson: If members have no questions, I propose that the Committee move through a number of clauses and come back to agree them, rather than agree them one by one.
989. Mr McMaster: Clause 3 concerns the Department’s general power. I want to distinguish between this clause and clause 2: a duty is inescapable, whereas a power is something that the Department can exercise if it considers it necessary. Clause 3 provides a general power for the Department to do almost anything that it wants in order to discharge and secure its general duty. The duty is very broad in the first place. This clause, therefore, provides very broad power for the Department to do anything in its power in order to improve the health and well-being of people in Northern Ireland — anything legal, I should say.
990. Clearly, there are other actions that are not specified in the clause. However, clause 3(1)(b) states that the Department may:
“do anything else which is calculated to facilitate, or is conducive or incidental to, the discharge of that duty.”
Paragraph (b) will simply give the Department the power to step outside its remit. The Department will normally secure the provision of those duties, from the regional board or elsewhere, but the wording does not stop the Department from providing them itself. If the Department finds that something is not being provided, it can employ someone directly to do it. It is a very broad power, but it also, more or less, a restatement of the general power given in the 1972 Order.
991. Clause 4 places a statutory obligation on the Department to determine, regularly, priorities and objectives for the provision of health and social care. The Department has done that in the past, although it was never a statutory requirement as it will be when the Bill becomes law. The Department can revise those priorities and objectives. Before doing that, however, it must, generally speaking, consult with the bodies in question.
992. The Department believes it right and proper that if it is setting objectives for bodies, it should consult with them. However, subsection (3) releases the Department from that obligation and provides for the doomsday scenario — for example, during the outbreak of a disease — when urgent action is required and there is no time for consultation. In such a case, the Department must demonstrate why the matter was so urgent that it did not consult. In the normal case of events, however, it must consult with the bodies on setting priorities and objectives.
993. Mr Buchanan: The safeguard is that the Department must explain why it took an urgent decision.
994. Mr McMaster: Indeed. This Committee, or anyone else, could ask the Department why it did not consult. The general requirement for the Department is to consult, but the Department realises that it must explain why it considered a matter so urgent that it did not consult.
995. The Deputy Chairperson: The British Medical Association (BMA) has called for retrospective consultations in such cases. Would that be beneficial?
996. Mr Mitchell: What did the BMA (NI) mean by that?
997. The Deputy Chairperson: The BMA said that meaningful consultation must be at the core of an issue. It also said that it would like the Department’s emergency decisions to be subject to retrospective consultation.
998. Mr McMaster: That might be difficult in some cases.
999. Mr Mitchell: Given the nature of the service that is provided in health and social care, action without consultation would occur only in extremis, when an immediate risk called for immediate action.
1000. In fact, action would be expected, and failure to act would, rightly, be criticised. The BMA (NI), and, subsequently, anyone else, can challenge why certain action was taken in a particular set of circumstances and criticise or take legal redress if it considers that an individual has acted outside his or her authority.
1001. Mr Easton: To pick up on what Tom Buchanan said, I am slightly concerned that clause 4(3) could be open to abuse, in that the Department could take action without consultation. I accept the concept of a doomsday scenario, but I would like a bit more beef on what constitutes the doomsday scenario that would permit such action. I would hate to agree to clause 4, only for a silly situation to arise that becomes an excuse for taking such action. A list of doomsday scenarios would be helpful.
1002. Mr McMaster: It quickly comes to mind that there could be a national emergency or an outbreak of some highly infectious disease.
1003. Mr Easton: Are there any other scenarios beyond those two?
1004. Mr Mitchell: I would avoid using the word “doomsday”, because it implies that such a scenario is unlikely. Given the nature of health and social care, it is not unusual for situations to arise in which a Minister feels that he or she must intervene, either because there is an issue of public concern or a risk to patients, carers or staff. The scenario may be linked to an outbreak of illness or a failure of infrastructure that means that a service can no longer be provided in a particular building. That is not a fanciful situation; in my experience, when a boiler house blew up at 3.00 am and there was no power to a particular building, immediate action was required. The word “doomsday” paints a misleading picture; it is not that uncommon, given the nature of the profession, for the Department to have the right to intervene in the public interest and in the interest of patients, clients or staff.
1005. Dr Deeny: In clause 4(3), perhaps the word “extreme” could be inserted before “urgency”. As a doctor, I know that the discovery of an animal with rabies on the island would be an extreme situation. GPs receive not only urgent referrals but “red flag” referrals, because some cases are more than urgent. Perhaps “urgency” is not a sufficiently strong word and could be preceded by “extreme”.
1006. Mr Gardiner: I can imagine instances of extreme urgency, but surely there would be enough time to inform the Committee. Rather than have the Department take a decision and leave us high and dry, we would have an opportunity to have an input.
1007. Mr Mitchell: That may be an option, but I am not being fanciful when I say that there would be circumstances in which something happened during a holiday period, at night, on a Friday evening or in the early hours of a Sunday morning that required a response there and then. To ask for total commitment to prior discussion would be to tie the hands of the Minister of the day in a situation that demanded his or her response. How that is defined is another issue, but the underlying need is important for patients and clients.
1008. Mr Gallagher: We must all accept that Departments cannot be compelled to come before the relevant Committee before making every decision — that is simply a fact of life in any democracy. Everyone knows that unexpected events will happen but not what they will be. Kieran probably came up with the best solution when he suggested the phrase “extreme urgency”. We will just have to leave it at that.
1009. A matter has cropped up. Do not misunderstand me; we do not always agree with the Department. It might have been at the outbreak of clostridium difficile, and the Minister and officials came to the Committee immediately to ensure that members were briefed. This place also has an Executive. Therefore, there are safeguards. As Kieran said, we must leave the matter there and hope that it will work.
1010. Mrs Hanna: Briefly, Deputy Chairperson, we can all understand that, in some circumstances, there is not time to consult the Committee. However, it might be appropriate for there to be a report and review afterwards, rather than consultation, so that people understand why it happened, what expenditure was involved, et cetera. Perhaps, that would be more sensible.
1011. The Deputy Chairperson: I suggest, therefore, that the word “extreme” is included — “the extreme urgency of the matter”. Also, Carmel’s suggestion that there should be a report and review immediately after the decision —
1012. Mrs Hanna: As soon as possible afterwards.
1013. Mr McMaster: In cases in which no consultation had taken place, the report and review could be carried out afterwards.
1014. Mrs Hanna: It is a bit difficult to undertake retrospective consultation.
1015. Mr McMaster: I understand that. Sometimes, it would be difficult.
1016. The Deputy Chairperson: Are you happy to consider that suggestion?
1017. Mr McMaster: Yes.
1018. Clause 5 provides a statutory requirement on the Department to produce a document which is to be known as a “framework document” for health and social-care bodies. To clarify, it will apply not only to bodies that are created under the Bill, but also to special agencies, trusts and the RQIA. It will clearly specify to each body what is expected of it and the procedures that it must follow to perform certain functions.
1019. The clause sets out what the document should include: the body’s main priorities and objectives and the process that it must employ to determine any other priorities and objectives that it might have, because it is recognised that organisations might also have certain internal targets. The document will also prescribe the matters for which the individual body is responsible. The Department will be required to set out roles and responsibilities for each of the bodies. That sort of clarity is considered to be essential for performance-managing the organisation. The document will set out the manner in which each of the bodies is to discharge its functions and conduct its working relationship with the Department and, indeed, other bodies in the health-and-social-care family.
1020. As has been said by Committee members, effective operation of proposed new structures will not depend on that legislation or even on subordinate legislation. It will depend on what happens on the ground. The document will go some way towards setting guidelines. Those matters must be included. However, subsection (2) states that it can also contain:
“(a) such guidance relating to the carrying out by each health and social care body of its functions, and
(b) such other material pertaining to the body or its functions”
as the Department considers appropriate.”
The provision requires the Department to keep the document under review and to revise it as and when necessary. Certainly, parts of the document will be reviewed fairly regularly.
1021. Subsection (4) requires that the Department to ensure that the framework document is “best calculated to promote” health and social care. That relationship refers back to the Department’s general duty to promote health and social care. It must ensure that the document has a purpose and that it is not merely bureaucratic gobbledygook. Its purpose is, generally, the promotion of health and social care.
1022. Subsection (5) covers consultation. The Department should consult with each body in respect to its functions and may consult with any other bodies that it considers appropriate. That could be the BMA, the Royal College of Nursing, or any other individual who has a particular expertise. The subsection does not limit the Department’s consultation powers or compel the Department to consult with each body.
1023. Subsection (6) says that each health and social care body must have regard to the framework document. That means that the body will follow the document’s instructions unless there is a compelling and exceptional reason not to do so. That is a broad outline of clause 5.
1024. Dr Deeny: When will the Committee see the framework document?
1025. Mr Mitchell: The Department is required to make it available before April 2009. We intend to complete a substantive draft by the end of November. At the moment, there is no plan to bring that to the Committee. That is our current timetable.
1026. The Deputy Chairperson: A response to our consultation suggested that the wording “may consult” in clause 5(5)(b) is too weak. One suggestion is to replace that phrase with “must consult with stakeholders” drawn up in conjunction with the Committee for Health, Social Services and Public Safety. What is your opinion on that amendment?
1027. Mr Mitchell: That it is the difficulty with the rigidity of the process. An extremely lengthy list of folk would have an interest in a high-level framework document.
1028. The Deputy Chairperson: Even if the legislation said “must consult with stakeholders”?
1029. Mr Mitchell: Every individual reasonably considers himself or herself a stakeholder in health and social care.
1030. Mr McMaster: I am concerned about the definition of the term “stakeholders”. How broad should it be?
1031. The Deputy Chairperson: Do members have any views on that matter?
1032. Mr Buchanan: The phrase “may consult” is weak; it leaves it open-ended and suggests that the Department can decide whether to bother consulting. Use of the word “must” will compel the Department to consult.
1033. The Deputy Chairperson: Could we change the word “may” in clause 5(5)(b) to “must”?
1034. Mr McMaster: That still leaves a way out. If the Department does not consider consultation to be appropriate, the compulsion to consult is almost irrelevant.
1035. Mrs Hanna: There is no problem with agreeing the framework. However, it is difficult to envisage how the document will come together because there is so little detail. I am unsure whether there is anything we can do about that. However, there are several gaps in the legislation, and the framework does not flesh it out. I do not know if there is any way around that. To some extent, I think that was Kieran’s point.
1036. Dr Deeny: Subsection (2) states: “The framework document may contain”.
That is ambiguous. Furthermore, 5(5)(b) says that the Department.
“may consult any other bodies or persons the Department considers appropriate.”
We must examine the framework document, and we should, perhaps, substitute the word “must” for the word “may” in clause 5(5)(b).
It should not be the Department’s prerogative to decide whom it is appropriate to consult: that leaves uncertainty. The appropriate people should be consulted.
1037. Mr Mitchell: To provide a flavour of the document, I would like to outline in more detail what it might contain.
1038. The initial section of our work is concerned with the financial and planning cycle. That is not about determining the amount of money that is allocated to an individual place each year, rather it is about how the process of a planning and financial cycle would work. That part of the document will highlight the performance and financial-management issues that need to be addressed. It will set out how priorities and targets will be established and monitored and how resources will be distributed, monitored and performance-managed by the Department. It will show how efficiencies, value for money, regulatory and probity will be reviewed and secured. That opening section is about how the cycle of planning, finance and performance works at a high level.
1039. The second section is concerned with the issues of governance, accountability, internal controls, standards and risk management at a high level. That section also explains how standards would be managed across the health and social care sector, how they would be issued and where the responsibility would lie for the monitoring of those standards. That section also explains the regulation of standards that derive from a regulatory basis.
1040. The priorities and objectives of each body in carrying out its functions will be outlined, not on a year-by-year basis, but their roles and responsibilities will be outlined on a substantive rolling basis. It will outline the issues for which a body is responsible, how it would be expected to discharge those functions and the arrangements for the provision of information to the Department.
1041. As we work on the document and begin to flesh it out, that is how we think it will look. The end of document will outline how it will be regularly reviewed to ensure that it is kept up to date. I hope that that information helps the Committee to get a feel for what the document will look like.
1042. Mr Gardiner: The difficulty that was mentioned could be overcome if the word “may” were replaced with “will” in clause 5(5)(b). It would say that the Department will: “consult any other bodies or persons the Department considers appropriate”.
That would get over the difficulty. The responsibility for who would be contacted would still lie with the Department, but that wording would mean that the Department will, rather than may, consult with those it deems necessary.
1043. Mrs Hanna: That would be helpful. It is difficult because the Bill is so important, and we are going through it line-by-line. Our timing is not consistent with some of the development in the Bill, so we are working in the dark. I appreciate that some of the information is a broad frame, but it would be helpful to have it fleshed out.
1044. Mr Mitchell: We will do our best.
1045. The Deputy Chairperson: You are happy to consider that.
1046. Mr McMaster: Clause 6 is fairly self-explanatory. It gives the Department the power to issue general or specific directions to the regional board, the agency and the regional support services organisation in carrying out their functions. Directions are a legal requirement; if someone were not doing something correctly, the Department could issue a direction telling them that they have to do it correctly. Subsection (4) states:
“It is the duty of a body to comply with any directions given to it under subsection (1).”
It is not envisaged that that power would be used on an everyday basis. It would be used when a body, despite negotiation and reference to the framework document, still does not comply. As a last resort, the Department would take the stance of formally directing the body to do something. Given that the Department has an overarching duty of care, it is important that that power is ultimate. If a body is not performing, it should be directed to do so, and bodies will be required to comply with that direction.
1047. You may wonder why only the regional board, the regional agency and the regional support services organisation are mentioned in clause 6(1).
1048. There is legislation in existence that established bodies such as the trusts, the special agencies and the RQIA. The power to give direction is already in the pieces of legislation that established those bodies. Therefore, we are simply taking the power in relation to bodies that we are creating anew in this Bill.
1049. One body missing from that clause is the patient and client council. We felt that it was inappropriate for the Department to direct the operations of a body whose primary purpose is representing patients. We will give it objectives and targets to meet rather than specifically directing it in the performance of its duties. For that reason, it has been omitted from this clause.
1050. Mr Gallagher: I have noticed that the ambulance trust is also included in the clause.
1051. Mr McMaster: The legislation establishes the trusts and grants powers of general direction. It includes the ambulance trust.
1052. Mr Gallagher: My apologies.
1053. Mr Easton: Clause 6(3)(b) states:
“because of the urgency of the matter, it is necessary to act… without that consultation.”
I accept that there could be a time when that will have to occur. However, to beef it up and to keep me happy, could we again put “extreme” before “urgency”?
1054. Mr McMaster: Whatever resolution we make in relation to the initial “urgency,” I believe that we should consider the same with the “extreme.” The Department will report retrospectively if that is felt suitable. We can consider that along with the other one.
1055. The Deputy Chairperson: Are there any other questions?
1056. Mr Gallagher: It has come up before, but the acronym RAPHSW recorded in 6(1)(b) is dreadful. Could we perhaps replace that with RPA so that it makes sense to people?
1057. Mr Buchanan: Indeed, it does not make sense.
1058. Mr Gardiner: I raised that point at a previous Committee meeting held at Muckamore Abbey Hospital. My idea was that we should spell out exactly what we are speaking of or trying to speak of, rather than using than abbreviation.
1059. Mr Mitchell: The creation of the names was an extremely difficult process. We spent an inordinate amount of time trying to develop them and there are considerable sensitivities surrounding them.
1060. The very long name for the regional agency has actually worked, in so far as there was a grave concern that the social well-being agenda was not being addressed, and that it would be a medically driven process. The Department applied that principle throughout the process to ensure that we were comprehensive and inclusive.
1061. I know that representations have been made to the Committee on the name of the regional support services organisation and I await the Committee’s view on that. In relation to the other bodies, the names are in common parlance within the service now and have — colloquially — been shortened to “the agency” and “the board”. As a result, people now understand what those bodies are.
1062. It does give the Department an issue in designing a logo. However, I can only caution the Committee that there was very grave difficulty in reaching the names that we did and there has been a degree of acceptance of those names, leaving aside what has been said to you in relation to the RSSO.
1063. Mr Gardiner: Could the process be revisited again?
1064. Mrs Hanna: I take that on board. However, Mr Gardiner’s point must also be taken on board for the sake of the public. A name of a body with a long acronym must clearly state what that organisation is. It is fine for people who work within the Health Service, but when it is that length, I do not think that it can be remembered unless it is written out.
1065. Mr Mitchell: Publications such as ‘The Belfast Telegraph’ refer to “the agency” and “the board” and it will quickly become understood to be that. Trying to come up with an alternative that is not seen to be siding with one part of an agenda or another is quite difficult.
1066. The Deputy Chairperson: OK. That concludes our examination of the six clauses that the Committee was due to consider today. I will not propose that we attempt to gain agreement on the clauses today. There are some things which will be further examined. Perhaps we can receive some feedback and take our discussion further the next time the Committee meets. I thank the witnesses for coming along today.
2 October 2008
Members present for all or part of the proceedings:
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Ms Mary Hinds |
Royal College of Nursing Northern Ireland |
1067. The Deputy Chairperson (Mrs M O’Neill): I welcome Mary Hinds and Ann Marie O’Neill from the Royal College of Nursing Northern Ireland. I invite you to make a presentation, after which Committee members will ask questions. Thirty minutes have been allocated for the evidence session.
1068. Mrs Ann Marie O’Neill (Royal College of Nursing Northern Ireland): I am the chairperson of the Royal College of Nursing Northern Ireland’s board and a member of the UK-wide governing council of the Royal College of Nursing. In my other life as a practising nurse, I work as a night sister in Antrim Area Hospital. Members will, of course, be familiar with my colleague Mary Hinds.
1069. We welcome the opportunity to make an oral submission on the Health and Social Care (Reform) Bill. We hope that the comments and written information that you received from us in August will help the Committee in making your decisions. I will now ask Mary to highlight key issues and how they relate to the Bill.
1070. Ms Mary Hinds (Royal College of Nursing Northern Ireland): I thank the Committee for inviting us to give evidence. In the interests of brevity, our evidence will deal only with the areas of the Bill with which we have issue or concern, and not the entire Bill.
1071. The Royal College of Nursing Northern Ireland supports the Minister’s stated intention to put the public-health agenda at the heart of the health and social-care system, as well as his intention to ensure the involvement of local communities and professionals in commissioning decisions.
1072. How the local commissioning groups, the regional health and social care board and the regional agency for public health and social well-being work together is central to the delivery of those objectives. We have concerns about four key areas: the relationships between those bodies; the strength of local voices; the membership of those bodies; and the timescales that challenge us all.
1073. I shall start with the relationships between local commissioning groups, the regional board and the regional agency. The RCN considers the relationship among those organisations to be one of partnership, not conflict. The legislation as introduced indicates that the regional board must consult the agency and have due regard for any advice or information that it provides. That is repeated for local commissioning groups, which are asked to consult the agency and have due regard for any advice or information they receive. Our view is that the relationship between those organisations must be described in stronger terms if a truly public health-led service, which is informed by local communities and expert professionals, is to be delivered. Advice is not sufficient. Throughout many years, nurses in Northern Ireland have learnt, when holding advisory positions, that advice can be taken, but, unfortunately, can also be ignored.
1074. The RCN also considers the language of direction to be no more appropriate to the relationship between those organisations. We prefer the language of partnership. The RCN suggest that the Bill’s language should be strengthened and, at least, that all plans should be signed off jointly by the local commissioning groups, the board and the agency. In that way, no one body has primacy over the others. We believe that that will provide checks and balances that will help to ensure that good local decisions are made.
1075. As stated in previous responses to consultation, the RCN is extremely supportive of the Minister’s direction on inclusion of local voices in the commissioning of services. Our concern relates to the weight that is given to those local representatives and professionals, particularly at local-commissioning level.
1076. The legislation describes the local commissioning groups as committees of the board. The RCN is concerned about the involvement and level of authority that local professionals and communities, or their representatives, will hold in commissions’ decision-making. If commissioning is to be truly local, an agreed level of authority must sit with local commissioning groups; otherwise, groups will be relegated to no more than debating chambers.
1077. To strengthen partnership between those bodies, as mentioned earlier, is a start. To ensure that optimum levels of commissioning are carried out at local level is another. We also accept that local commissioning groups will have different priorities. Therefore, one solution will not necessarily fit all.
1078. However, the principle of decisions about local commissioning being close to patients and communities, informed by those communities’ representatives and professionals, is one that could be more explicitly described.
1079. I will now move to the issue of membership of the various bodies. The Bill does not provide detail about the composition of the regional board, the regional agency or the local commissioning groups. Although that had caused us some concern, we have since received a consultation paper on the membership of the regional board and the regional agency, and we will respond to that appropriately.
1080. As a general principle, the Royal College of Nursing Northern Ireland believes that clinical-and social-care professionals and community representatives should be central to the membership of all those groups. Indeed, nurses have, to date, successfully contributed to commissioning at regional board and local health and social care group level. However, we believe that it would be helpful to clarify, and if required, make explicit in the legislation, the role of district councillors as members of the regional board.
1081. The Royal College of Nursing Northern Ireland particularly welcomes the inclusion of local representatives in the structures. Health and social care is a public service, and the public should be a part of its governance. We know that that will not necessarily be easy, as it involves all of us balancing competing priorities and interests. However, we believe that problems must be owned, shared, understood and acted on. We can only do that if we do it together.
1082. We also recognise that building trust, confidence and governance capacity will take time. As nurses, we are committed to playing our part by working with colleagues, including our local councillors, to develop the capacity and understanding of the entire team. We look forward to learning from colleagues in return.
1083. The primary legislation does not provide information about the composition of the local commissioning groups. That may be entirely appropriate, given the level of detail. We wish it to be noted, however, that the proposal as it currently stands has the RCN’s support, with the following proviso: having discussed at length the membership of the LCGs, the RCN has chosen not to enter into a debate about who holds however many seats around the table. As we see it, the local commissioning groups must work as a collective team, and not as an adversarial committee in which one group outvotes the other. That said, we expect the nurse on the local commissioning group to be enabled to develop a network of nursing colleagues who will help inform decisions. We recommend that, in the knowledge that no one nurse can represent, on her or his own, the broad church of nursing.
1084. We are delighted that progress has been made, but having waited some time to get to this point, we urge all parties to this reform to work together in order to ensure that the legislative timetable is adhered to. To ask the service, our patients and our staff to endure any more delays in the reform process, which has already stretched over two years, is unacceptable. The staff, particularly of the regional board and the regional agency, who have been affected by this final set of reforms, have lived with uncertainty for too long.
1085. Thank you for listening to our submissions. I am happy to answer any questions.
1086. The Deputy Chairperson: Thank you very much. We will take on board the concerns that you have outlined today. The concerns about the strength of the local commissioning groups have been a common theme in our deliberations, as have concerns about local voices making local decisions and not being overruled at another level.
1087. Mrs Hanna: You are very welcome, Mary and Ann Marie. I have raised concerns, as have other members of the Committee, about who will be involved in decision-making. There is no point in being a member of a regional agency or a regional board unless those bodies have decision-making powers. No one that we have talked to, including the members of the regional board when we met them at Muckamore Abbey Hospital, knows what is happening. That is part of the problem; the situation has gone on for so long, and there is still a great deal of uncertainty about the detail. The devil is in the detail, and everyone at the table will agree with me that we must have sight of the composition of the various bodies before decisions are made.
1088. The need for partnership is essential, from the bottom-up as well as the top-down, or the new bodies will not work.
1089. We have a great opportunity, particularly with the establishment of the regional agency, and it is absolutely essential that everybody is involved. Especially with regard to the local commissioning groups, it is essential that you and other health professionals are involved in those, and work with local councillors to ensure that there is a capacity to make a difference, particularly considering the new powers that local councils will have to deal with health and well-being.
1090. Dr Deeny: Thank you again, Mary and Ann Marie. My contribution will be short, because the proposed changes seem to be on a consistent course, and I am delighted to hear it. I will repeat some of what Carmel has said; what the Committee heard last week from the chief executives of the health and social services boards; and what the patient watchdogs; health and social services councils; and now your organisation have told the Committee: what is needed is a bottom-up approach. I know that there are members of my own profession here today, representing the British Medical Association.
1091. The LCGs that preceded the new proposals did not work, because they were not seen to be taking a bottom-up approach. That message has been expressed by everybody, that there must be a bottom-up approach, and as a Committee we must see that that is the case. We have to stamp our authority on this, and make clear that all of the groups that have given evidence to the Committee have agreed that there must be a bottom-up approach.
1092. Not every decision made locally will be an easy one, or popular with the communities. We know that, but it has to be that way. It would be wrong to establish bodies that are merely advisory, and that can be overruled by a central authority in Belfast. If that were the case, I believe that, not just GPs, but other health professionals, would walk away. The established bodies must have authority, otherwise the proposed reform will fall flat on its face, and we will be back to the situation that has been the case until now. Currently, were one to ask the man or woman on the street, in Omagh or any other town, who is on the local health board, and who has responsibility for commissioning health care in the area, they would not know. There is no knowledge of who makes the decisions on commissioning health care, and there is no accountability. That has been the case for far too long.
1093. My question concerns the number of lay members on the LCGs. I have forgotten what the proposed makeup of those groups is, as the number of groups has changed from five to seven, and other changes have been made. I know that there will be four councillors, four GPs, a nurse, as you say, and different allied health professionals on the LCGs. You say that you do not want to become involved in this debate, but the Committee raised it last week with the representative of the health and social services council. From what I understand, with the establishment of the patient and client council, the patient will have a more of a say, and more authority, not just to complain, but to contribute. How many lay members will there, or should there, be in the new commissioning groups?
1094. Ms Hinds: I think the proposal at the minute is that there should be two. It must be remembered that, although it is appropriate that such lay members have a say, and they may represent particular specialist interest groups, we should not underestimate the closeness of local councillors to the public, and the public are those who become clients and patients. There are few of us who have not visited a GP over the past twelve months, for instance. The proposal makes provision for a lovely mix of both expert professionals and local representatives, whether local councillors or lay members.
1095. Mrs A M O’Neill: If the general public are included in the LCGs it would generate great public confidence in the system, and the support of the councillors.
1096. The Deputy Chairperson: The proposals as outlined by the Minister make provision for the inclusion of two voluntary sector representatives from the health and social care sector in the LCGs. Would those be the lay members?
1097. Ms Hinds: Yes, we think that that refers to lay members. As Carmel said, the devil is in the detail of such proposals.
1098. The Deputy Chairperson: No other members have indicated that they wish to speak. You have explained it so well that we do not need to ask any more questions. Thank you very much for coming along to this meeting, and we will take on board the issues that you have raised.
1099. Mrs A M O’Neill: I thank the Committee for allowing us to present the information that we have given. As you know, nurses deliver the majority of patient care, and it is essential that nurses have a voice on the commissioning groups, because performance and commissioning are key to what happens to our patients, and we want the best for patients, and for all of the people in Northern Ireland. Thank you.
9 October 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Mr Thomas Buchanan
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Witnesses:
|
Mr Craig Allen |
Department of Health, Social Services and Public Safety |
1100. The Chairperson (Mrs I Robinson): We shall now continue with the clause-by-clause consideration of the Health and Social Care (Reform) Bill. I welcome back the Chief Medical Officer — one might say that he is a glutton for punishment, appearing before the Committee twice in a row. I will not call you Pinocchio. I also welcome Ivan McMaster, Bernard Mitchell and Craig Allen from the Department of Health, Social Services and Public Safety. The officials are here to explain the meaning of each clause and to provide clarification or answer questions as required.
1101. At last week’s meeting, members considered the first six clauses of the Bill but deferred reaching any formal decision on them. The officials agreed to take away some suggested amendments for further consideration. Rather than going back over those clauses again today, I propose that, at this stage, we resume consideration where we left off and work through the remaining clauses, from clause 7 onwards. We will formally consider each clause at a later meeting.
1102. Before I ask the officials to explain the meaning of clause 7, which deals with the establishment of the proposed regional health and social care board, we should have a more general discussion on the overall structures. I understand that, at last week’s meeting, the need for a separate regional agency for public health and social well-being was raised. It is important that we begin by asking the officials to talk us through the rationale for creating a regional board and a separate regional agency for public health. Although there is strong support for a separate agency for public health, members will note that some of those who made submissions to the Committee had concerns about the lack of clarity about the relationship between the board and the agency and how responsibilities would be split between the two. I invite the officials to address that issue, and members can ask questions afterwards.
1103. Mr Bernard Mitchell (Department of Health, Social Services and Public Safety): I will start with the broad picture — the perceived role of the agency and the reason for the establishment of an agency as well as a regional board. In today’s earlier evidence session, the Chief Medical Officer outlined the many existing inequalities in morbidity and mortality rates in Northern Ireland. The need to address those inequalities was one of the driving factors underpinning all the reforms and structural models that we have put in place. We must consider the impact on the individuals concerned and whether effective resource utilisation is being achieved; there is an issue about whether the best use is being made of taxpayers’ money if treatment regimes have to be put in place because we have failed to address, at an earlier stage, prevention and health and well-being issues.
1104. One of our ongoing concerns has been to ensure that the profile of public health and social well-being is sufficiently focused and high on the agenda. If responsibility for public health and social well-being is to lie with a regional board that will inevitably be driven by the significant operational concerns and priorities that must be addressed, the prioritisation of funds specifically targeted at public health and social well-being can necessarily take second place. One of the reasons for proposing the creation of an agency was to ensure that that agenda and the important objective underpinning the reforms would be dealt with in a focused manner.
1105. Another important issue was the need to develop improved partnership, not only with local government but with the full range of public-sector stakeholders and others who have a strong influence and a role to play in improving public health and social well-being. Therefore, the new agency has been specifically charged with that responsibility, and it will be given a very high profile in its management structures and core remit. Indeed, that is a key reason for the establishment of an agency.
1106. Although the consultation responses showed that there is, and has always been, a great deal of support for the development of an agency for public health and social well-being, equally, there is a recognition of the need to ensure that the agency and the board work together in a fully integrated manner. Therefore, we have carefully considered — and will continue to consider carefully — the matter, and, at the end of the day, that approach will be embodied in the framework document to which we referred last week.
1107. I will make a couple of points by way of illustration. First, integrated working between the staff from the agency and the board is a prerequisite of the new structure. The local commissioning groups (LCGs) will operate efficiently only if the support that they receive from staff on the ground is professionally led but with all the other requisite management skills in place. That approach will heavily involve staff from both the agency and the board.
1108. It is our intention, as part of our planning process, to ensure that those units will be fully integrated and co-located, so that staff are working in the same place, many of them in their local communities. We feel that that is where they should be based.
1109. We are also considering how that integration will operate at a regional level. Having talked about the local arrangements, we are thinking carefully about the regional level and how a commissioning plan is developed in an integrated way and is genuinely a joint commissioning plan, with the ownership of the regional agency and the regional board. That will ensure that the regional agency not only has influence over the moneys directly allocated to it but has influence over the £4 billion or £4·5 billion expenditure that the regional board will spend every year on health and social care in Northern Ireland.
1110. There has been a driving imperative from the start and a real belief that the separation of the regional agency was fundamental to the objectives that we were all required to deliver. We were conscious of the resulting organisational issues that were raised, and we believe that we are addressing those issues sensibly, one-by-one.
1111. Dr Michael McBride (Department of Health, Social Services and Public Safety): May I add to that? Bernard has summarised the issues nicely. It is about achieving a balance, raising the profile of health improvement and health protection and working in partnership with local government and other important bodies in, for example, education and policing. It is about meeting the needs of local communities and working at local commissioning group level, as Tom Buchanan mentioned earlier, with staff outposted from the regional agency and co-located with other staff in support of the LCGs in order to establish services that meet the needs of local communities.
1112. I am sorry that Tom Buchanan has left the meeting, because he raised an important concern about duplication and about the pitch being too crowded. It is about integration, as Bernard said, without duplication. There must be absolute clarity about the respective roles and the shared roles and responsibilities. The operating framework document will provide that clarity. As Bernard also said, we have also considered joint commissioning arrangements and the suggestions about joint sign-off that were made by members of the Committee in a previous meeting. We are actively considering those alternatives in order to ensure that there is complete clarity about who does what in the new system.
1113. The challenges that we face in dealing with preventable ill-health and premature death, particularly in deprived areas, are very real and very stark. We must raise the profile of public-health challenges and increase our attention on them. I am concerned that if we opted for a unitary model, the pressures of which we are all too aware, and which are covered by the media day in, day out, week after week, will determine and drive that agenda.
1114. Regrettably — and tragically — we do not yet see headlines in the media about the fact that there is a difference in life expectancy of two years, four years or seven years, depending on whether one lives in a deprived area or an affluent one. We should be motivated and driven by that. I support the Minister’s view that public health and social well-being must be at the heart of all Government policy. There are clear benefits in added value to the economy. The Wanless and Appleby reports made it clear that investment in health and well-being makes sound economic sense in Northern Ireland. It gives people better life opportunities, better employability and, ultimately, it is a good thing to do. I strongly support the Minister’s outline proposals for the establishment of a separate regional agency for public health and social well-being.
1115. The Chairperson: I want to quote from a letter to the Committee from Paul McBrearty of the Mental Health Commission:
“One of the major strengths of the HPSS within Northern Ireland is its integrated structure which has been the case at senior levels within the Boards for more than 35 years and is now reflected within the Trust management and operational delivery structures. The proposal to now create two separate bodies (i.e. a Regional Public Health Agency and a Regional Commissioning Board) has significant potential to disrupt this integration. We can see no good reason why this proposal for separation is being made. If separate divisions are necessary to ensure that different interests are served, then so be it but this can surely be achieved while maintaining staff within a single corporate entity, single senior management leadership, and single point accountability.”
The Royal College of Nursing also has major concerns:
“The RAPHSW creates the potential for duplication of effort and waste of resources, and is illustrative of the overly complex and potentially problematic nature of the proposed governance and management relationships between the new bodies.”
Those two significant groups are making strong comments that are worth flagging up.
1116. Mr Easton: I have no problem with the establishment of the regional board; that is a good thing. However, I am concerned at the establishment of a separate regional agency for public health. I thought that the purpose of the reform was to create savings, create effective structures, reduce bureaucracy and make life easier. The establishment of a separate regional agency adds another layer to the health programme, and I am not convinced that such a separate structure is needed. It should be within the remit of the regional board, and it could work just as effectively as part of that board. It could do a more effective job and would certainly create efficiency savings, thereby saving a lot of money. I do not believe that there is a need for the establishment of a regional agency. It should be part of that whole structure. I am not content to support the Bill as it stands, with the regional agency separate from the regional board. That is my position.
1117. Mr Mitchell: The commitment to savings will be met within the new structures; it has been hard-wired into all the proposals. The figure of £53 million in savings, and the reduction of posts, is part and parcel of all the proposals, and the savings to which commitment has been given in the review of public administration (RPA) will be made. There are currently: four health and social services boards; the Central Services Agency; the Health Promotion Agency; the Mental Health Commission; and the Northern Ireland Regional Medical Physics Agency. Irrespective of the RPA, there would have been a shared services organisation, because there was commitment to a programme of shared services. Under the new arrangements, there will be a regional board, a regional agency and a regional support services organisation. Three new bodies will replace the agencies that I have mentioned, so there is a clear reduction in the number of bodies.
1118. One of the big questions raised by Paul McBrearty — with whose view I fundamentally disagree — is whether the same focus can be achieved within the regional board. That is the essence of many of the concerns. Would a board that faces the kind of financial pressures that a regional board will face — such as the Committee has been discussing — be able to prioritise the funding required for public health and social well-being in the way in which it should be prioritised? Would that aspect of healthcare receive the kind of additional investment that we think it needs? My argument is that it would not. That will happen only if there is a separate body, with its own focus and its own board. It is worth saying that, in developing the management structures for the two bodies, great care has been taken not to duplicate and to jigsaw the two organisations so that the senior posts and the professional input of each complement each other. We are not in the business of replicating all the functions of a board in an agency, or vice versa. We are in the business of making the two organisations work together as an integrated whole, because no one wants duplication or for us to waste resources in that way.
1119. Dr McBride: Although I am not familiar with the quotes that the Chairperson has just read out, I assure the Committee that there will be no duplication of effort; the operating framework will provide that clarity.
1120. The RPA savings are a given. Irrespective of what model we select — whether there is a board or an agency, for example — the £53 million savings will be realised. There will be no additional bureaucracy, because that will also be clarified in the operating framework.
1121. Returning to the economic argument, economist Derek Wanless has said that we must do more about the new public-health agenda. We must invest more upstream if we are to continue to have a publicly funded Health Service that is free at the point of delivery. Therefore, there is a solid economic argument supporting that. In the earlier evidence session, the Minister referred to the economic case for that renewed focus.
1122. Compared with how much of our budget we spend on acute services, the amount that is spent on public health pales into insignificance. The establishment of the agency is an opportunity to provide some counterbalances in the system. We will always need to provide, and invest in, acute services, community services and services to ensure that people who are unwell recover and are supported in their homes. However, we must, simultaneously, invest in the upstream side of the wider public-health agenda.
1123. I support Bernard in saying that the ethos and culture of those organisations will be different. Given the pressures that will be put on a single organisation, I am afraid that I know, from past experience, who the poor relative would be. It would be the public-health agenda and the challenges that we face in dealing with the health inequalities and the disproportionate impact that that has on the most deprived areas. Not everyone in Northern Ireland is equally well or has an equal life chance.
1124. Mr Easton: I do not see how it is not more cost-effective for the service to be provided within a board rather than its having a separate identity. I do not see how the services being managed together rather than separately will disadvantage certain areas. I appreciate what you said, but the agency would be an extra layer of bureaucracy and would be cumbersome, so I maintain that it is better if all services are provided through a single board. However, the matter should not be considered during the scrutiny of clause 7.
1125. The Chairperson: We will discuss clause 12 later and if a vote is required, so be it.
1126. Dr Deeny: Gentlemen, I want you to convince me of the need for the agency, as I believe that that is why you are here. I have heard it asked, not only in this Building or this Room, why the agency cannot be incorporated within the board. I am aware that Alex has also asked that question and that you had been explaining the reasons for that, Michael.
1127. I take your point, Bernard, that the amount of unnecessary bureaucracy is being decreased, but that must be done efficiently. How many people do you envisage working in the regional board, the regional agency and in the Department of Health, Social Services and Public Safety? The public ought to be told that.
1128. Michael, you said that you knew who the poor relative would be if there were a single organisation, but surely that day is gone. We now have a devolved Assembly, there is a Committee for Health, Social Services and Public Safety, and there is accountability. I know the chief executive of the Health Promotion Agency well and, as a GP, public education and public health are important to me. Therefore, I agree that those elements must play a major part in the future of healthcare in Northern Ireland. Nonetheless, even if public health were the poor relative, surely it would be up to the relevant organisations to come to the Committee, which would see to it that that was not the case.
1129. Mr Mitchell: We are in the final throes of a detailed staff-mapping exercise. It requires us to meet all the current employing organisations, and their staff, to resolve their current roles and responsibilities and, depending on what they do, allocate them to different bodies. It is a complicated exercise, which we are carrying out in partnership with the trade unions. It is nearing completion, but I cannot give you the final figures. However, I can give you the figures that are in the public domain.
1130. The Minister has given a commitment that the staffing of the board will be below 400. Earlier, the Minister said that the figure for the regional agency would be between 250 and 350 staff, although I suspect that it will be towards the former rather than the latter. The figure for the Department would be in the region of 700 staff. I emphasise that all those figures are subject to the completion of the staff-mapping exercise and to us working out definitive figures that we can bring back and share with the Committee.
1131. Dr McBride: I respect the views that have been expressed, and the Committee has listened attentively to my points. However, in relation to the “why”, I have not yet heard a reason that challenges the concept of having a separate regional agency. We are facing huge and stark challenges. As Bernard has said, the tendency will be to focus on the short to medium term, and that has always been the focus of the Health Service. We all agree that we need to address health inequalities, to invest upsteam and prevent ill health and premature death. However, when it comes down to the pressure decisions of where the money will go, we will put it where we always put it — into services.
1132. We need some balance and challenge in the system. The Health Committee has an important role in providing that challenge. Equally, we need that challenge to happen at the front line where the commissioning plans are being agreed: we need to work to support LCGs, local government and local authorities to decide and determine those interventions that will improve the outlook for people in communities. That is the challenge.
1133. I do not believe that we will have the same opportunity to achieve what we all want to deliver within a single body that will be fundamentally focused and directed to the significant challenges of developing, maintaining and sustaining service delivery. This is a unique opportunity.
1134. However, there are real tensions. If a single body is examining waiting times, access targets and the challenge of healthcare-associated infections, and it knows that there is an interrelationship between many of the factors that contribute to one and factors that address another, there must be a tension and an appropriate challenge in that system. I am concerned that the appropriate challenge will not happen in a single organisation. There must be a dynamic tension between the health-improvement and health-protection agenda and commissioning and delivering services, and that is why it is needed.
1135. The Chairperson: The Committee will raise that issue.
1136. Mrs Hanna: I will try to be brief. I have listened to your arguments, and I welcome the strong focus on public health. In all my time in the Health Service, I have never heard it being talked up so much. There have been arguments and pros and cons with the previous trusts about whether they should have responsibility for primary and secondary care. We have mostly considered those services in the acute hospitals. In some ways, I welcome the Belfast Health and Social Care Trust, although I wonder how it will balance its resources. It makes sense for the trust to put money into primary care and keep people out of hospital, although I do not know whether that will happen.
1137. However, if there is to be a separate agency — and I would be happy about that because we need to focus on public health — we must ensure that that body will be able to make decisions. If the agency cannot make decisions about expenditure on public health, there is no point in having it. It needs to communicate well, and public-health professionals and experts need to be represented on the agency if it is to make a difference and work with people in the communities.
1138. I take on board everything Michael and Bernard have said. The challenge is huge. I hope it works, but it will not unless genuine decision-making powers are given the agency.
1139. Dr McBride: I think that the Minister has been very clear on that.
1140. Mrs Hanna: Will the regional agency take responsibility for public health in trusts? Will it be responsible for the public-health function?
1141. Mr Mitchell: The Minister has said repeatedly that the regional agency for public health and social well-being should be at the heart of the full commissioning process. As I pointed out at the outset, one of the givens is the fiscal co-location of the agency and board staff working together to support the local commissioning groups, because that is where the bulk of the money will be committed and the bulk of the decisions will be made. If the agency, nurses, allied health professionals, various managers and other staff all work together, and if they are co-located and supportive of the local commissioning groups and doing what they are meant to be doing, the kind of integration and influence that Mrs Hanna wants is — by definition — built into the process.
1142. The other part of the task has been to try to ensure that that is mirrored on a regional level. Therefore, we have given careful consideration as to how to put in place the kind of joint ownership of the commissioning plan that Mrs Hanna has described. The challenge that we face is to ensure that the agency has influence, which it can bring to bear on the board’s total expenditure. If the agency falls into the trap of solely managing public-health streams, it will find itself in a rut. It needs to look at the full breadth of the health- and social-care system. We want to give the agency input into expenditure across the full range that the board is committing, through service and budget agreements, with the trusts. That will not just be reflected in the public-health aspect of the agreements but in every programme of care within them, whether they are for maternal and child healthcare, care of elderly people or anything else.
1143. Dr McBride: The difficulty is that the model is so new, and the thinking that underpins it is challenging. Sam Gardiner mentioned at the earlier evidence session that change is difficult for everyone, and everyone involved in healthcare is coping with significant changes. Michelle’s comments on trade unions and her stress on the need to keep staff informed and on board are important.
1144. I return to Tommy Gallagher’s point about local commissioning groups. Bernard is absolutely right: that is where it all locks together. That level is the interface with local government, other local authorities and communities. The teams work in an integrated and collective way to move forward the entire agenda. Alex Easton and Tom Buchanan have raised concerns about that; their questions are legitimate. However, I reiterate that this is about achieving more balance in the system in deciding health- and social-care priorities. By all means, we must continue to support and improve the services that we provide. We must provide better quality and safer services; however, at the same time, we must embrace, and take ownership of, the agenda for improving the health of the population.
1145. Investing for Health was a product of the previous Executive, and it had cross-party support. At the time, the Chief Medical Officer for England said that it was the best public-health document written in the English language; and whereas we have had significant improvements in the health of the population in Northern Ireland, we have not fully realised them. We have not fully delivered so that people in Northern Ireland communities are uniformly and equally well.
1146. To my mind, this process provides an additional opportunity to ensure that the appropriate challenge function is there when we are committing resources and determining commissioning plans so that, as Bernard has indicated, the agency has influence over the totality of the spend. That dynamic tension needs to be in the system if we are to realise the Wanless “fully-engaged” scenario that is recommended for the population of Northern Ireland in the Appleby Report, contain costs, improve the outlook for the population of Northern Ireland and, at the same time, reap the economic benefits. We are beginning to see that investment in health is investment in the wealth of the population and in the Northern Ireland economy.
1147. Mrs Hanna: At this stage, we must realise that all the issues have been identified. We must also realise that decisions must be made about where resources should be invested. That is why I asked that question. The agency must have some decision-making powers, otherwise it will be able only to identify the issues that we have already spelt out rather than actually make a difference. It must be able to make decisions about where resources are focused — such as prevention and early intervention — rather than to employ well-meaning, experienced, professional people who will tell us what we already know.
1148. Dr McBride: Perhaps that is at the root of some of the concerns that have been raised, such as whether the agency be sidelined or whether it will be a toothless body that sits on the sideline seeking to negotiate and influence, but yet, as Carmel said, has no real power, control, influence or decision-making powers. The Minister has made it clear that that will not be the case. Do you want to elaborate on that, Bernard?
1149. Mr Mitchell: We are building that into the entire infrastructure. Specifically, on 1 July, the Minister announced that he was committed to examining the issue of joint sign-off. We are examining the practicalities of that. That is a potential means through which the kind of influence that Mrs Hanna spoke about could be delivered.
1150. Mrs O’Neill: From an Investing for Health perspective, I support the principle of the regional agency. We must welcome the focus on prevention and promotion. That is essential. There are concerns about how that will filter down on the ground and whether commissioning plans will reflect the agency’s priorities. Among other groups, the Royal College of Nursing has proposed some amendments to strengthen that relationship. As a Committee we can examine those.
1151. The Chairperson: Michael, are you leaving now?
1152. Dr McBride: I am happy to stay, Chairperson, if there is anything else that members wish to ask.
1153. The Chairperson: I know that you came to talk about the specific issue of efficiency savings, but you are welcome to stay, if you wish.
1154. I invite officials to outline the meaning of clause 7 and schedule 1. Afterwards, I will invite questions from members. I remind members that in considering each clause, they may wish to take account of views expressed in written and oral submissions to the Committee.
1155. Mr Ivan McMaster (Department of Health, Social Services and Public Safety): Clause 7 establishes the regional health and social care board that will replace the four current health and social services boards. Clause 7(1) states: “There shall be a body corporate”.
1156. That means that the board has rights and responsibilities through interpretation of the Bill including: the right to regulate its own business and to employ its own staff; the power to enter into any contracts and to sue and be sued; and the right to decide its corporate name.
1157. Clause 7(2) states:
“Schedule 1 applies in relation to the Regional Board.”
1158. Paragraph 1(1) of schedule 1 sets out the status of the regional board.
1159. Paragraph 2(1) of schedule 1 sets out the regional board’s general powers:
“the Regional Board may do anything which appears to it to be necessary or expedient for the purpose of, or in connection with, the exercise of its functions.”
1160. The main restriction is that the regional board is subject to any directions that the Department may give. Obviously, the Department will monitor the work of the regional board.
1161. Paragraph 2(2) of schedule 1 states:
“But the Regional Board may not borrow money.”
1162. Paragraph 3(1) of schedule 1 sets out the membership of the regional board:
“The Regional Board shall consist of —
(a) a Chair appointed by the Department;
(b) a prescribed number of persons appointed by the Department;
(c) the chief officer of the Regional Board;
(d) such other officers of the Regional Board as may be prescribed”.
1163. The Department is currently working on the subordinate legislation that prescribes the details of those positions. Decisions have yet to be made on whether those positions should be designated to certain people on the board and what types of skills those employees would require or what types of posts they would have needed to have undertaken previously.
1164. Schedule 1 also deals with other issues such as remuneration allowances and terms of office — that is, when a person may resign or be removed from office. I can deal with any issues that members would like to raise on clause 7.
1165. The Chairperson: Members will have the opportunity to read through the schedule and raise any issues. I do not see the need to go through each of the headings.
1166. The Committee will revisit clause 7 at a later stage to agree it formally. Is there broad agreement among members with clause 7 as drafted?
Members indicated assent.
1167. The Chairperson: Schedule 1 is fairly straightforward, but, again, the Committee will revisit it at a later date to agree it formally. Is there broad agreement with schedule 1 as drafted?
Members indicated assent.
1168. The Chairperson: We now turn to clause 8, which deals with the functions of the regional board.
1169. Mr McMaster: Clause 8 sets out the statutory functions of the regional board. Those functions are dealt with in more detail in clause 24. Broadly speaking, clause 8 transfers all the statutory functions currently exercised by the health and social services boards to the new regional health and social care board or to the proposed regional agency for public health and social well-being. The functions dealing with health improvement and health protection will transfer to the regional agency, and everything else will transfer to the regional health and social care board.
1170. That provision does not seek to replace existing legislation. Therefore, all existing functions — contained in statutes such as the Mental Health (Northern Ireland) Order 1986 or the Children (Northern Ireland) Order 1995 — will remain extant and will transfer en bloc to the regional health and social care board.
1171. Clause 8(2) requires that the regional health and social care board, in carrying out its functions, examine specific areas. It requires that the regional board does so with the aim of:
“improving the performance of HSC trusts … establishing and maintaining effective systems ... managing the performance of HSC trusts … commissioning health and social care”.
1172. Those are the broad duties that the regional board will undertake.
1173. Clause 8(3) requires the regional board to carry out a “commissioning plan” each financial year, and there is a statutory requirement that that plan be published. It also provides a permissive power for the Department to specify what that plan should contain. However, it is expected that that would be used only as a fall-back option.
1174. As currently worded, clause 8(3) requires that the regional board consult with the regional agency and, having consulted with it, to:
“have due regard to any advice or information provided by it.”
1175. The Minister is considering strengthening that power in relation to joint sign-off.
1176. Clause 8(4) explains that the functions given to the regional board in clause 8(1) are deemed to be functions that the Department has directed the board to carry out. It is retrospective in approach, and it covers any future statutes that may also confer directions.
1177. Clause 8(5) relates to the Department’s general powers, which are laid out in clause 3. Clause 8(5) allows the regional board to exercise its wide-ranging power to the same extent. In other words, as the board takes its functions from the Department, the overarching duties of the Department should also be the duties of the regional board. It is a wide-ranging power and limited only to the extent that the action must facilitate, or be conducive to, the discharge of the board’s duty.
1178. The Chairperson: The Committee will formally agree the clause later. Is there broad agreement with clause 8 as drafted?
Members indicated assent.
1179. The Chairperson: The Committee will now consider clause 9, which deals with local commissioning groups.
1180. Mr McMaster: Clause 9 requires the regional health and social care board to establish a prescribed number of local commissioning groups. The regional board will have the power through schedule 1 to set up whatever committees and subcommittees it chooses. However, clause 9 is specific in requiring the creation of local commissioning groups as committees of the board.
1181. Clause 9(1) simply gives them the title “local commissioning groups” and allows for regulations prescribing their number. The current thinking is that there will be five, in line with the number of trusts. However, the Minister has indicated that he may reconsider that, in light of what emerges from the local government review. In any case, the introduction of those measures through subordinate legislation allows more flexibility.
1182. Clause 9(2) permits the Department to specify the geographical area for which the local commissioning groups will be responsible.
1183. Clause 9(3) provides the local commissioning groups with certain statutory functions. Clause 9 (3)(a) states:
“such functions with respect to the commissioning of health and social care as may be prescribed”.
1184. That is a fairly broad term. The subordinate legislation will go a stage or two further than that in breaking down that role.
1185. Clause 9(3)(b) provides for local commissioning groups to perform:
“such other functions as the Regional Board may, with the agreement of the Department, determine.”
1186. The LCGs were established principally to commission health and social care services, which is why the power granted to the regional board to provide the commissioning groups with other functions is restricted and is to be exercised only with the Department’s approval.
1187. Clause 9(4)(a) requires each local commissioning group to:
“exercise its function in accordance with any scheme for the time being having effect under article 18 of the Order of 1972”.
1188. Under the Health and Personal Social Services (Northern Ireland) Order 1972, health and social services boards were required to submit a scheme to the Department as to how they would carry out their functions. The technical terminology used in clause 9(4)(a) means that, as committees of the regional board, the commissioning groups must provide services for any scheme that the board submits on its own performance and function to the Department.
1189. Clause 9(4)(b) places an absolute requirement on a local commissioning group to consult with the regional agency. That is in addition to consultation on the commissioning plan. In the course of its general duties, a commissioning group must consult with the regional agency. The Department assumes the power to direct any other consultations that it requires the local commissioning groups to undertake. Again, the use of that directing power would be regarded as a last resort.
1190. Clause 9(5) sets out the specific aims that local commissioning groups must strive to meet. They include:
“improving the health and social well-being of people in the area … planning and commissioning health and social care to meet the needs of people in that area”
and:
“securing the delivery to people in that area”.
1191. I will not go through all the aims. They are listed in the Bill.
1192. Clause 9(6) provides the regulation-making power under which the Department makes provision for membership of the commissioning groups and is allowed to make any other provisions to the groups that are considered appropriate.
1193. Clause 9(7) makes it clear that:
“Before making regulations under subsection (6), the Department must consult the Regional Board.”
1194. Mr Gallagher: It may not be a matter for today, but my question relates to the prescribed number of local commissioning groups. There appears to be an assumption that there will be five groups to reflect the five trusts. I am not sure that that would deliver the best results, particularly in the west, in reflecting and responding to the needs of local communities.
1195. Dr Deeny: I declare an interest as a member of an LCG. The Committee has had worthwhile presentations over the past few weeks from the BMA, the Royal College of Nursing, the allied health professionals, the chief executives of the health and social services boards, the Regulation and Quality Improvement Authority and representatives of the health and social services councils — the patients’ advocates. We asked them for their views, and they all gave us consistent replies.
1196. Clause 9 deals with local commissioning groups. Clause 9(3) states:
“ Each Local Commissioning Group shall exercise —
(a) such functions with respect to the commissioning of health and social care as may be prescribed; and
(b) such functions as the Regional Board may, with the agreement of the Department, determine.”
1197. Who prescribes the functions? General practitioners and elected representatives share the views of the six groups that I have mentioned. The local health and social care groups that were their predecessors did not work because the GPs saw them as taking a top-down approach as opposed to a bottom-up approach. No one who is interested in becoming involved in local commissioning groups wants them to act simply as advisory bodies or talking shops, in which every decision has to go back to the regional board to be approved.
1198. I liked what Bernard said earlier about supporting LCGs. We must have that commitment from the Department. I spoke to an optometrist who was upset that his profession will no longer be represented on local commissioning groups. That is a backward step. This is national eye care week. Optometrists served on local health and social care groups up to now. We can deal with that matter later. I want to get that commitment from the Department.
1199. I do not want this idea to collapse because it is a wonderful opportunity to commission services according to the needs of our local communities. At the earlier evidence session, the Minister said that different areas will have varying needs. Local people know who is accountable and who will take decisions, some of which might be unpopular, but at least they are known to the local community.
1200. Last week, the editor of a major GP magazines said that what is happening in Northern Ireland is unique and that other countries would watch with interest to see if it works. I hope that the local commissioning groups will have the clout to make decisions. Those decisions will have to be approved by the regional board, which will be backed up by the necessary finance.
1201. Mr McMaster: The word “prescribed” as used anywhere in the Bill means prescribed by regulations made by the Department. That is defined in clause 31(1).
1202. Mr Easton: Clause 9(2) states:
“Each Local Commissioning Group shall exercise its functions as regards such area of Northern Ireland as may be prescribed.”
1203. That is a wee bit airy-fairy and does not include the new council arrangements, although you touched on that issue earlier. I would like that to be toughened up by stating that each local commissioning group shall exercise its functions within one of the Northern Ireland local government districts. That would take in the councils and ensure that the LCGs will not be spread all over the place but will take in a solid council area. I propose that wording, because it is tougher and more straightforward.
1204. Mr Mitchell: Coterminosity with local government is regarded as a fundamental part of the reforms. There is a proposal to have five local commissioning groups to match the existing five trusts; however, we are waiting for the outcome of local government reform and the redrawing of local government boundaries. We previously gave a commitment that the issue would be revisited when those decisions were made. It was always felt that it would embody coterminosity. However, it would not be on a one-to-one basis, but rather it would be between one or two councils and the local commissioning group. That is the intent that underpinned the wording.
1205. Mr Easton: That is not a definite commitment.
1206. Mr Mitchell: It is a commitment to review the boundaries after the outcome of local government reform.
1207. The Chairperson: The regulations will come to the Committee.
1208. Mrs O’Neill: I want to return to the issue of the work of the agency and the linking up with local commissioning groups. The Royal College of Nursing has made a suggestion that would help to allay any fears. It wishes to strengthen clause 9(4)(b) from: “in connection with the exercise of its functions —
(i) consult RAPHSW and have due regard to any advice or information provided by it;”
to the following:
“to work in partnership with RAPHSW and be able to demonstrate that the exercise of its functions reflects the priorities determined by RAPHSW”.
We talked about that issue earlier. The priorities for health promotion must be reflected in the commissioning plan.
1209. Mr Mitchell: I am a newcomer to some of the legislative processes; therefore, some of it comes down to my understanding of what a draftsman advises us. We were advised that “have due regard to” was the strongest legislative wording that could be used. In a sense, that is a belt-and-braces approach, because, for me, the real answer to the RCN query relates to the co-location of integrated commissioning support units and joint membership of the local commissioning groups. The local commissioning group will develop an annual commissioning plan, and public-health consultants, senior nursing staff and allied health professionals will be part and parcel of the development of the plan and its subsequent monitoring. That ensures that we achieve the kind of integration that we all want. We share that view with the RCN. The draftsmen advised us that the wording that we used was the strongest possible wording that could be used for the obligation that we were laying on the local commissioning group.
1210. Mrs O’Neill: I accept what you are saying, but members have expressed concerns about the role of the agency, and the RCN and other organisations have also expressed concerns about it. Therefore, the amended wording would go some way to allaying those concerns. Perhaps you could take away that wording and discuss it.
1211. Mr Mitchell: Will you give us the wording again?
1212. Mrs O’Neill: The wording needs to be strengthened and amended to read: “to work in partnership with RAPHSW and be able to demonstrate that the exercise of its functions reflects the priorities determined by RAPHSW”.
1213. Mr Mitchell: We will check that out.
1214. The Chairperson: The Committee requests that the Department re-examines clause 9 and considers implementing the suggestion made by Michelle O’Neill. Are members in broad agreement with clause 9 as drafted?
Members indicated assent.
1215. The Chairperson: We will now move on to clause 10, which deals with the power of the regional board to give directions and guidance to health and social care trusts.
1216. Mr McMaster: One of the duties being given to the regional board is the management and improvement of health and social care trusts’ performance. Clauses 10 and 11 give the regional board stronger powers to fulfil that duty. Clause 10 will give the board legislative power to guide trusts and to direct them to take certain courses of actions. The regional board must consult the trust concerned and obtain the Department’s approval before issuing that legislatively based direction.
1217. As we discussed at last week’s meeting, clause 10(4) deems that it would be inappropriate and impracticable for the regional board to consult in urgent matters of patient safety, for example. Clause 10(5) outlines that the regional board is not allowed to give direction that is inconsistent with that already given by the Department. Under the legislation that established the trusts, the Department has the power to direct trusts in how they carry out their functions. Clause 10(5) ensures that any direction issued by the regional board is consistent with what is already on the statute book.
1218. Clause 10(6) obliges a trust to comply with the duties given to it and to have regard to any guidance given to it by clauses 10(1) and 10(2). Clause 10(7) grants the Department the power to prescribe that the provisions of clause 10 can apply to any other organisation that may carry out functions on behalf of the regional board in the future. However, there is no thinking that clause 10(7) will have to be used in the near future.
1219. Mr Gallagher: Does clause 10 reflect only the current situation?
1220. Mr McMaster: At present, health and social services boards advise trusts and manage their performance, but they do not have a formal direction-making power to tell trusts how to carry out their duties.
1221. Mr Gallagher: Therefore, clause 10 will give boards a stronger power.
1222. Mr McMaster: Yes; clause 10 will give boards a stronger power and improve performance management in the trusts.
1223. The Chairperson: Are members in broad agreement with clause 10 as drafted?
Members indicated assent.
1224. The Chairperson: We will move on to clause 11, which deals with the provision of information, etc, to the regional board by health and social care trusts.
1225. Mr McMaster: Clause 11 is linked to the performance management role that the regional board will have. The Health and Personal Social Services (Northern Ireland) Order 1991 — which established the trusts — requires trusts to record and pass on certain information, mostly to the Department. Clause 11 will place a duty on trusts to record information under the direction of the regional board; trusts will have to provide the board with information and furnish its reports. Therefore, clause 11 further strengthens the role that the new regional board will have in managing the performance of the five trusts.
1226. The Chairperson: Are members in broad agreement with clause 11 as drafted?
Members indicated assent.
1227. The Chairperson: We will end the session now, as it is 5.20 pm. I appreciate that members of the Committee have long journeys home and will want to avoid bottlenecks. I am fortunate that I live just down the road. I thank Bernard, Ivan and Craig very much for their attendance. We will see them again next Thursday to examine the remaining clauses and schedules.
16 October 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mr Thomas Buchanan
r Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mrs Claire McGill
Ms Sue Ramsey
Witnesses:
|
Mr Craig Allen |
Department of Health, Social Services and Public Safety |
1228. The Chairperson (Mrs I Robinson): I welcome Mr Bernard Mitchell, Mr Ivan McMaster and Mr Craig Allen from the Department of Health, Social Services and Public Safety, along with Dr Michael McBride, the Chief Medical Officer, to the Committee’s continuing clause-by-clause consideration of the Health and Social Care (Reform) Bill. They are here to explain the meaning of the clauses of the Bill, provide clarification and answer questions as required.
1229. We will continue where we left off last week. Clause 12 establishes the regional agency for public health and social well-being. Before I invite the officials to explain the meaning of the clause, together with the corresponding schedule 2, I am conscious that we had a fairly detailed discussion about the merits of the proposed regional agency during last week’s meeting. I invite the officials to outline briefly the provisions in clause 12 and the corresponding schedule 2, after which members will have an opportunity to ask questions.
1230. Mr Ivan McMaster (Department of Health, Social Services and Public Safety): Clause 12 establishes a regional agency for public health and social well-being as a body corporate. As we discussed last week, that allows the organisation to do certain things on its own, such as regulate its own procedures and employ its own staff. Schedule 2 deals with the constitution and operation of the regional agency. Schedule 2 is almost an exact copy of schedule 1, which establishes the regional board. The one significant variation is that the regional agency’s board is granted permission to include a prescribed number of local elected representatives, the numbers of which will be determined by subordinate legislation.
1231. Mr Easton: I am not against a regional agency per se, but I am still not convinced of its merits as a stand-alone body that is separate from the proposed regional board. I see it as an extra layer of bureaucracy, the cost of which would be substantial at a time when we are expected to be making efficiency savings. I do not understand why it cannot be part of the regional board and still do just as good a job, if it is placed in the right context within the board, and if its funding is properly examined. I do not accept that it must be separate.
1232. Will the regional agency make its decisions independently, or will it need the separate agreement of the regional board or the Department? I am confused about that. The money for the agency would be better spent if it were an internal organ of the regional board. I propose that clause 12 be subsumed into clause 6 so that there is a joint body, rather than two bodies.
1233. Ms S Ramsey: I partly understand what Alex is saying. We must be careful not to make any decisions on that issue for the time being. I am conscious that many people who responded to the consultation see the proposals for a regional board and a regional agency as a positive way ahead. I am not saying that those people are right or wrong. When we talk about front-line services and front-line service delivery, we are talking about the organisations that provide those services.
1234. In its submission to the Committee, the Royal College of Nursing (RCN) argues that its proposed amendments to clauses 8(3) and 9(4)(1) would mean that:
“the relationship between RAPHSW on the one hand and the Regional Board and Local Commissioning Groups on the other will become one of strategic partnership rather than simply consultation and advice. This will, in turn, help to ensure that public health is firmly at the forefront of service design and delivery”.
1235. I want to tease that issue out, because if we are saying that organisations such as the RCN are the experts in certain matters, we could be going against what they and other service providers want to aspire to in the Health Service.
1236. Dr Deeny: I have to take on board what Michael McBride said last week, namely, that if the agency is incorporated into the board, public health may well become the poor relation. My understanding — and I would like verification from the officials and the Chief Medical Officer — is that the local commissioning groups (LCGs) will have the clout to commission services locally and that an important part of their work will be to work alongside the regional agency.
1237. Public health — and I have been in general practice for years — public education and health promotion are an important part of our future, so I would not like to think that the local commissioning groups would be working with part of a board that was treated like a poor relation.
1238. In addition, we are concerned about bureaucracy, and if we are thinking about decreasing bureaucracy, I do not want people losing their jobs. I asked Bernard last week about staff numbers, and the figures 700, 400 and 250 were mentioned. Some people would say that 1,400 members of staff is a large number of people administering the Health Service from Belfast for a population of 1?7 million.
1239. The answer, possibly, is to have fewer people in each of the bodies. To have 700 people in the Department seems to be a lot, when we have a population that is only the size of Yorkshire. I have come round to believing that the regional agency must be separate from the board because the local commissioning groups need to get top advice — and very important advice about public health and health promotion — from a body that is not treated as a poor relation. Will you confirm that that is the case and explain how they will work together?
1240. Dr Michael McBride (Department of Health, Social Services and Public Safety): That is the point that Tommy Gallagher made clearly about the locality level at last week’s Committee meeting. Staff from the board and the agency will support LCGs in delivering the service needs of local communities and populations, and in addressing the challenges of health inequalities in order that everyone is equally well.
1241. More importantly, agency staff will focus on, and work with, other partnerships in local government, local authorities, local policing and in education, because it is not services that determine whether someone is healthy, but good education, life and employment opportunities, and the communities, environment and network around people that make them feel supported and as valued members of society. That is what keeps people healthy and well: loving families and supportive communities. The Department will give emphasis and profile to public health.
1242. For once, we will not be saying one thing about public health and doing another, because we all talk the talk and say that it is important to address health inequalities so that everyone is equally well. However, if you ask me a question about the Department’s proportionate spend vis-à-vis health services compared with dealing with health inequalities, we spend less than 1% of our budget on addressing health inequalities and improving the health of the population with upstream interventions. That is the fact of the matter.
1243. By creating a separate agency, the Department will be saying to the public of Northern Ireland that public health is an important issue. We will also ensure that that agency is a key and equal player in negotiating leverage over the totality of the budget for the board and the agency. At that grass-roots level, you will not see the join: they will work in partnership because they have to do that.
1244. Dr Deeny: You spoke about elected representatives on the agency. That is new to me. Will you elaborate?
1245. Mr Bernard Mitchell (Department of Health, Social Services and Public Safety): Two elected representatives are provided for on the board of the agency.
1246. Dr Deeny: Will they be councillors?
1247. Mr Mitchell: They will be district councillors.
1248. Mr McMaster: Paragraph 3(1)(f) of schedule 2 provides for:
“a prescribed number of members of district councils appointed by the Department in such manner as may be prescribed.”
1249. Mrs Hanna: I support the establishment of a separate agency for public health for the very reasons that have been outlined: addressing health inequalities, early intervention and prevention. However, I have raised concerns about the agency having teeth. It must be a real partnership, bottom-up as well as top-down. That is my only concern. I understand that, in the day-to-day running, the issue of public health could get lost if it is linked into the regional board.
1250. However, I still need to be convinced that it will have teeth and will make a difference. It must not be a talking shop: it needs to have public-health professionals on board, and they must be able to make decisions.
1251. Mr Mitchell: We will provide a detailed framework — and I do not mean the framework document. We are doing specific work at present, following on from the Minister’s advice that he wishes to give consideration to joint sign-up. We are doing detailed work on the relationship between the board and the agency to ensure that the product of their work is an integrated commissioning plan, of which both have ownership, both approve and — as I said at last week’s meeting — which gives the agency not only direct input into the smaller amounts of money that it will commit but very significant influence over the £4 billion that the board spends in total. In that way, the agency can begin to shape the pattern of expenditure, target it, and achieve the outcomes in public health and social well-being that we want.
1252. I have no difficulty whatsoever in assuring members that a clear, solid framework will emerge that will describe exactly how the two organisations will work in an integrated way to a common agenda.
1253. Mrs Hanna: That is fair enough. It is helpful that you have articulated that in detail.
1254. Dr McBride: That is at the root of Alex’s important appeal for absolute clarity about this — eye-watering clarity. As the discussion that we have just had illustrates, the difficulty is that such clarity is not outlined in the legislation. That is part of the challenge.
1255. Sue asked about consultative responses: we have had an unprecedented response to this consultation exercise. From what we have heard, and from what people have told us, some 59% of all respondents support the development of a separate agency for public health; 20% were undecided —
1256. Mr Mitchell: If I may correct you, 59% of those who discussed the issue of the agency —
1257. Dr McBride: I am sorry: 59% of those who discussed the issue of the agency were in support of it; 20% were undecided; and another 21% of those who had discussed that issue were not supportive.
1258. It is worth mentioning the bodies that were supportive: the Royal College of Physicians of Ireland; Royal College of Midwives UK Board for Northern Ireland; the Health Promotion Agency; the Northern Ireland Chief Environmental Health Officers Group; the Northern Ireland Association for Mental Health; the Institute of Public Health in Ireland; the British Dental Association; the British Psychological Society; and the Health Protection Agency in London.
1259. Sue referred to a submission from the RCN: it emphasised the need to put public health at the centre. It qualified its response by saying that it needed to see more detail. That is entirely appropriate. The Committee also needs more information and discussion to ensure that it has all the details.
1260. Mr Gardiner: I support what Sue and Carmel have said, and I concur with their views. It is a little like the relationship between this Committee and the Department: we oversee what the Department and the Minister does. If we do not establish an independent agency to oversee what the board is doing, we allow the Minister and the Department to run the show as they see fit. However, we are here as elected public representatives. We are doing a good job, and I encourage and support the establishment of the agency.
1261. Mr Buchanan: My views are well known. I do not see the need to set up another agency. I take on board the positive aspects of setting up an agency and putting public health in the forefront, but I cannot see why that cannot be incorporated within the board. It should be one body rather than a separate agency that would need up to 400 staff to administer.
1262. For example, across Northern Ireland, district policing partnerships and community safety partnerships were set up; they run in tandem and work is duplicated. There is no need for those two partnerships. We will be setting up a board and an agency, and there will be a duplication of work that is not required. I cannot see why the two bodies cannot be in the one board.
1263. It was mentioned that the Committee may need more clarification to find out what the regional agency would do and what powers it would have. Perhaps the matter should be deferred. I cannot see why we need to set up another agency to run alongside the board. The work could be incorporated into one body that could do as good a job as a separate agency.
1264. Dr McBride: The important point is that there would be no more staff. Staff numbers would remain exactly the same whether there is to be a separate agency or a unified model. The efficiency savings will be realised, and there will be no more staff in either model.
1265. To answer the question about why there should not be a single model: we have 20 years’ experience of a single model, albeit separated into four boards. We still have not seen the problems associated with health inequalities or improvements in healthcare being addressed successfully. Mr Buchanan is right to challenge our thinking on a unitary model. I do not know whether the unitary model will deliver anything different from what was delivered previously.
1266. The Committee has met the community and voluntary sector, and it knows that, frequently, because of acute pressures and the issues about the financial balance of trusts, the projects that are working well at a local and community level are not being disseminated widely across Northern Ireland and implemented on the ground. Indeed, many of those organisations are surviving on short-term funding from year to year with end-of-year-slippage money from boards. Public health is not central and is not a major priority for boards at present. However, that is not because the boards do not want to do it; it is because they are distracted with more immediate and pressing issues, and they cannot get round to the longer term, more sustainable issue of building on a foundation of public health.
1267. In a single organisation, the public-health agenda would disappear. The health-protection agenda, which we have not discussed, is important. Canada, post-SARS 2003, moved to establish an agency for public health for the sole reason that it recognised that a separate agency would give a higher profile to the health-protection challenges, whether those challenges might be healthcare-associated infections or multi-drug-resistant bacteria, such as listeria or tuberculosis, which are on the increase in our communities, or whether it might be a pandemic flu outbreak. It is about building resilience and capacity into the system so that public health is strong — and that is not only about health services.
1268. Mr Mitchell: The staff would be senior professional medical, nursing and allied health staff who currently work in the boards and have a significant input to the commissioning process. They also have a significant input into the public-health and well-being agenda.
1269. Whether there is a unitary body or two bodies, those people’s work must still be done. In a single-body model, rather than those people working for the agency, they would work for the board because their jobs must still be done. Any savings that would be made would be fairly limited and would come primarily from the positions of chairperson, chief executive and a small number of directors’ posts that may be lost.
1270. When working on the new organisations, we were careful not to replicate support services functions so that the agency would not be seen, for example, to set up its own human resources, finance and corporate services machinery. We envisage that the organisation will get those services from other parts of the system. That is why the somewhat anomalous situation exists, in which it appears that there are an additional 200 staff to run the new agency. That is not the case. If, tomorrow, there were to be no new agency, the bulk of those staff would belong to the new board because their work must still be done. Any savings would be made at the upper echelons and would not be that significant. I welcome the opportunity to explain that.
1271. The Chairperson: I am sorry, Sue. I want to invite Tommy to ask a question.
1272. Mr Gallagher: Will Sue get a chance to ask another question?
1273. The Chairperson: I will bring Sue back in at the end.
1274. Ms S Ramsey: Thank you.
1275. Mr Gallagher: I support the idea of there being two separate bodies. I am happy that we proceed on that basis. We must decide soon whether there will be one or two organisations.
1276. A much stronger public-health message is needed. The best way to do that is with separate authorities. The problem with the public-health message is that several authorities seem to be responsible for it; the Health Promotion Agency and the trusts all carry out health promotion and such activities. We are worse off for that as regards hammering out a strong message on health promotion and public health. Therefore, I am happy that the two authorities be separate.
1277. Will the situation continue in which trusts do essentially the same work? They are not mentioned in the Bill because they do not need to be. Are they empowered under the relevant legislation, the Health and Personal Social Services (Northern Ireland) Order 1991, to carry out a certain health-promotion function? If they still have that function under legislation, that will result in duplication of functions. Perhaps someone can throw some light on that matter.
1278. Mr Mitchell: This issue featured prominently during consultation. At its conclusion, many people cautioned against wholesale centralisation of trust staff who are currently based in local communities where they do work that is valued highly. We certainly got that message from the trusts. We also got it strongly from the community and voluntary sector, who said that we must be careful: if it ain’t broke, don’t fix it. They value the interaction by local trust staff. Their advice was not to pool all those functions managerially at a central point.
1279. Our response was to limit the functions that are taken over by the new agency — those that relate to the work of the health action zones, for example — where we felt that we could bring improved partnership and better regional focus to the provision of those services. We seek to strike a balance, therefore, between what is brought into central management and what is left to local control. That was in direct response to views that we heard during consultation.
1280. Dr McBride: Tom Buchanan made an important point about ensuring that there is no duplication and used the example of community safety partnerships. We will try to ensure that staff in the health action zones and the Investing for Health partnerships work as one team.
1281. Later in the legislation, we have placed a duty of public health and social well-being on trusts. That goes back to Dr Deeny’s important point: it is about ensuring that those who work in health and social care do not regard their primary role on the front line as treating the sick, such as patients with acute myocardial infarction or diabetes. Instead, it is about working proactively to ensure that someone who has had acute myocardial infarction, for example, is given advice about diets, exercise programmes and smoking cessation. It is important that the staff in trusts retain their patient focus.
1282. We want a Health Service where all staff, regardless of whether we are cardiologists or work with people who live with diabetes, say that their target is to no longer have people arriving at clinics with illnesses such as diabetes. For that to happen, we all must address the problem of obesity.
1283. The fundamental aim of the Bill is to realign health and social care and take it upstream. We must turn off the tap, because if we do not — as Derek Wanless stated — the Health Service will not be able to cope with the demographic changes in our population, the increase in life expectancy, people living with long-term conditions and the problems related to obesity and the diseases of modern society. Therefore, we must fundamentally change tack, move upstream and ensure that the majority of staff who work at the service end of health and social care regard that task as an important part of their job.
1284. Mr Mitchell: That is referred to in clause 21.
1285. Ms S Ramsey: Although I sympathise with what Alex and Tom are saying, investment is always made in acute care rather than community care. We must prevent illnesses; in my constituency, as with any other, the source of the problem must be tackled. If one organisation has control, the money will be lost, because it will be spent on treating illnesses rather tackling their source.
1286. Mr Easton: I do not agree that money would be lost if there were a single organisation — that will not happen if the correct structures exist. If the Committee agrees, I could withdraw my proposal and the issue could be discussed next week when we could be provided with information on the cost of establishing the new agency and more details on its structures.
1287. The Chairperson: I would suggest that we do not have a formal vote now. The risk is that the vote could go either way, and that could have significant implications for other parts of the Bill. I would prefer if we parked that proposal until we receive some clarification on costings and other points that were raised, including a better explanation on the points that Alex and Tom raised. I do not want to divide the Committee on the proposal.
1288. Paragraph 7(3) of schedule 2 is wrongly drafted and, unless corrected, will result in a situation where RAPHSW committees have to comprise exclusively of regional board members. The words “regional board” should be replaced by “RAPHSW board”.
1289. Mr McMaster: Yes; that is on page 29 of the Bill and is a drafting error caused by cutting and pasting.
1290. The Chairperson: If the wording is not fixed now, we could be in trouble later.
1291. We now move to clause 13, which details the functions of the regional agency for public health and social well-being. I invite Ivan to explain that clause.
1292. Mr McMaster: Clause 13 details the agency’s functions and provides clarification in relation to those. In very broad terms, clause 13(1) explains that the agency will have health-improvement and health-protection functions. Clauses 13(2) and 13(3) provide further details about those functions. Clause 13(2) refers to health improvement and to the agency’s requirement to take proactive steps to develop programmes and initiatives that will be targeted at improving the health and social well-being of the Northern Ireland public.
1293. It should be noted that those are not solely targeted at health. Given our uniquely integrated service, those programmes and initiatives will also improve the social well-being of the public and will reduce health inequalities.
1294. Clause 13(3) gives details of the agency’s envisaged health-protection functions that will protect the community — or any part of it — against communicable diseases. Currently, the main communicable diseases that are being dealt with are: measles; mumps; rubella; polio; tuberculosis; and hepatitis A, B and C.
1295. Those functions will also deal with any other dangers to the health and social well-being of the public. Those wide-ranging duties are designed to cover anything that could be regarded as a danger. The power, therefore, is not limited at all, although it will often refer to more common dangers, such as environmental or public-health issues.
1296. Clause 13(4) provides details of the areas in which the new agency will become involved in the exercising of those functions, such as undertaking research or providing laboratory, technical or clinical services. Clause 13(5) provides the Department with the power to alter the functions of the proposed new agency, either by adding or removing functions. That is a fairly new departure, and — in light of experience — the Department of Health, Social Services and Public Safety reserves the right to change those functions. Clause 29 will ensure that no Order that amends those functions will be made unless it is placed formally before, and debated in, the Assembly, so the Department will not be able to amend the functions without the Assembly’s approval.
1297. Clause 13(6) states that the proposed new agency will be required to co-operate with other bodies. There is no limit on the bodies with which the agency must co-operate, and it is clear that the list is not even restricted to health- and social-care bodies. The agency will be required to co-operate with local councils in relation to environmental health functions and with such other bodies under any arrangement for joint working.
1298. Clause 13(7) is a mirror image of clause 13(6), in that it requires any body referred to in that subsection to co-operate with the agency. Clause 13(8) is a technical inclusion that will provide the new agency with protection, because it will be compelled to provide information by clauses 13(6) and 13(7). Any provision of information will not be regarded as a breach of restrictions on the disclosure of information that might apply. However, the agency must note that that does not formally authorise the disclosure of information that contravenes the Data Protection Act 1998.
1299. Dr Deeny: Before the Committee considered the Bill, I was unclear about the proposed agency and its functions. However, I increasingly agree with my medical colleague Michael. I have spent 28 years of my life looking after the sick and treating diseases. More focus should be given to — and more finance should be provided for — disease prevention, as opposed to only the treatment of diseases. That is the future, particularly as the population is getting older, as Michael pointed out. If we have the resources, the time, the financial back-up and the support of an agency such as the one that is proposed, we would be able to prevent many diseases.
1300. In the past, we waited until people became sick and then treated them. We are now trying to focus on preventing heart attacks, diabetes, strokes, and so forth, so I am increasingly seeing the benefits of the proposed agency.
1301. Mrs McGill: Disability Action made the point that clause 13(2)(b) needs to be expanded to better outline the health-promotion function. Is that a valid point?
1302. Mr Mitchell: Did it suggest a form of wording?
1303. Mrs McGill: I have not seen a form of wording, but it may be included in its substantive response.
1304. Mr Mitchell: Forgive me, but what was Disability Action’s concern?
1305. Mrs McGill: It felt that clause 13(2)(b) needs to be expanded to better outline the health-promotion function. It may have suggested a form of wording, but I do not have that information in front of me.
1306. The Chairperson: Disability Action’s opinion on this piece of legislation is that clause 13(2)(b) needs to be expanded to better outline the health-promotion function.
1307. Mr Mitchell: We will take that away and consider a form of wording.
1308. Dr McBride: We have not been restrictive at all. I am merely echoing the point that was made earlier about the health-protection or health-promotion function. The regional agency will be responsible for health and social well-being. We are happy to go away and consider any issues that you may have.
1309. The Chairperson: Disability Action:
“commends the comprehensiveness of clause 13(2)(a) but believes that 13(2)(b) should be expanded to better outline the Health promotion function.”
1310. It is not a very detailed point, but perhaps you could consider it. Members are generally happy, but obviously there will be an impact, depending on whether there are one or two authorities.
1311. Mr Buchanan: The British Red Cross has suggested a form of wording to strengthen the clause. It suggests including the words “and risk reduction” after “health promotion”.
1312. The Chairperson: Bernard, we are happy to give you a copy of the responses from those organisations, and you can come back to us with responses to them.
1313. Ms S Ramsey: It would be useful if the Department were provided with a copy of those responses, because the Association of the British Pharmaceutical Industry has suggested that clause 13(4)(e) should be amended to read:
“make available to any other body, after consultation with the Assembly Committee for Health, Social Services and Public Safety, such persons, materials, information and facilities as are deemed appropriate.”
1314. I know that we are nuisances, but the Committee should be included in clause 13.
1315. The Chairperson: We are simply protecting our backs. The devil is in the detail.
1316. Mr McMaster: May I just clarify that we are talking about clause 13(4)(e)? At the moment it reads:
“make available to any other body”.
1317. Ms S Ramsey: We are the real body.
1318. Mr McMaster: You are not simply “any other body”. [Laughter.]
1319. The Chairperson: We could not possibly comment on that.
1320. Dr McBride: I increasingly get the feeling that I am the Health Committee’s personal physician, and I am sure that Sue will not require smoking cessation services or anything else.
1321. The Chairperson: At this stage, I must rein everyone in and say that enough is enough.
1322. We are generally happy, but we will come back to the issue of the two authorities next week when we get more detail on it.
1323. Clause 14 relates to the regional support services organisation. Will you talk us through the clause together with the corresponding schedule 3. It is worth noting that the Central Services Agency had concerns about the title of the organisation and its acronym — RSSO.
1324. Mr Mitchell: Are you content for the Chief Medical Officer to leave at this point?
1325. The Chairperson: Of course. Thank you for your additional help on the issue of breast screening. I appreciate your speedy response to the matter.
(The Temporary Chairperson
[Ms S Ramsey] in the Chair)
1326. Mr McMaster: Clause 14 creates a regional support services organisation as a body corporate — much like the organisations that we have been dealing with so far — and introduces schedule 3, which deals with the establishment of that organisation. Schedule 3 is somewhat different from schedules 1 and 2. It takes a different tack as the support services organisation will not provide services to the public. It is something of a new venture, so many of the provisions in relation to tenure of office and circumstances in which people can be removed or suspended from office, the appointment of committees, and so forth, will be provided through subordinate legislation, as set out in schedule 3. Initially, it is likely that that subordinate legislation will create an organisation that is a little different from the board and the agency. That is why schedule 3 differs from schedules 1 and 2.
1327. Mr Easton: I have no problem except for the new organisation’s acronym. Will you consider that? We do not want the organisation to be a laughing stock; it is a serious matter.
1328. Mr Mitchell: There is a proposal to change the name of the organisation to the “regional business services organisation”. We would be content to consider that.
1329. Mr Easton: That sounds better.
1330. Mr McMaster: It started life as a “common services organisation”, but the use of the word “common” is not suitable, because the organisation must provide services for more than one body. The technical term “common” cannot be used, because it might be required to provide a particular service for one of the bodies. That is how we arrived at the regional support services organisation. I am afraid that we were not really thinking about acronyms at the time.
1331. Mr Gallagher: Briefly, what services will the organisation provide?
1332. Mr McMaster: I will come to that.
1333. The Temporary Chairperson: The Committee agrees to come back to the title of the organisation at next week’s meeting. We will now move on to clause 15.
1334. Mr McMaster: Clause 15 sets out the services that the organisation — I will call it the regional support services organisation, for the moment — is to provide. Clause 15(1) gives a general description that the organisation is to provide:
“support services to other health and social care bodies in accordance with directions under subsection (4).”
1335. Clause 15(2) broadly lists the services that need to be carried out on behalf of health and social care bodies. They are:
“(a) administrative support, advice and assistance;
(b) financial services;
(c) human resource, personnel and corporate services;
(d) training;
(e) the management and maintenance of buildings, equipment and land;
(f) information technology and information management;
(g) the procurement of goods and services;
(h) legal, medical, scientific or other professional services;
(i) contractual compliance, internal audit and fraud prevention.”
1336. Those services are relevant to the contracts that boards currently hold with practitioners. Those are the services that the organisation is designed to provide.
1337. Clause 15(3) requires the organisation to ensure that its arrangements for providing those services represent value for money for its customers and that they are provided in the most economic, efficient and effective way. To ensure that that is done, the organisation will be required to have those arrangements approved by the Department. It is implicit that, without such approval, the provision of the services to the bodies concerned cannot be commenced.
1338. Clause 15(4) provides the Department with the power to control the flow of services to the new support services organisation by giving directions. The organisation will not take on everything from day one; there will be a drip-feeding of responsibilities. Some of the services will have to be provided by the organisations themselves, but, as time goes on, the services will be provided by the new support services organisation.
(The Chairperson [Mrs I Robinson] in the Chair)
1339. This provision by direction gives a number of safeguards. It will ensure that health and social care bodies will use the organisation and not go elsewhere for their functions because that will be required under the directions. It will allow the Department to be satisfied that the organisation is properly equipped to carry out its functions, and it will enable a phased approach to be taken to the central provision of those functions. It will also ensure that health and social care bodies do not ask their organisations to carry out functions that are inappropriate. Anyone could ask this organisation to do something simply because it is too difficult or they do not like it — for example, the job of firing someone. This clause will prevent that type of action.
1340. Clause 15(5) permits the regional support services organisation to charge its customers for the services that it provides. Clause 15(6) again provides the power for the Department to alter the functions of the new organisation and, similar to that provided by the proposed new agency, this will be done by an Order which will be brought before the Assembly. The Assembly would, therefore, have a say in that change — either adding to, or taking from, those functions.
1341. Mrs McGill: Clause 15(3)(a) is mentioned in the responses to the Committee. The Northern Health and Social Services Board asks that the word “equitable” be added after “economic” and before “efficient”, so that the clause would read:
“secure that those services are provided in the most economic, equitable, efficient and effective way”.
1342. I support that. Is that possible?
1343. Mr Mitchell: I suppose that comes down to an assessment of what “equitable” means in the type of services that we are discussing. We are talking about supplies services, human resource functions, payroll functions and payments of accounts — operational, day-to-day transaction functions. That is largely what this new body is concerned with. The body’s customers are other health and social care bodies. When one asks if that works in an equitable way, all health and social care bodies are required to meet the obligations laid on them by section 75 of the Northern Ireland Act 1998, which informs how they do their business. It is difficult to give a commitment in legislation, given the nature of the services that the new organisation will provide. One wonders how it could be demonstrated that the type of service that I am talking about had been provided in an equitable way.
1344. Mrs McGill: I understand what you are saying, but every Health Service is supposed to be equitable in all aspects. I do not find that to be the case. It depends, in many instances, on where you live. I would like to see the word “equitable” included, and I wonder why the Northern Board has asked for that in its response. Whatever the service happens to be — and you have outlined the services — I think that it would be good to have the word “equitable” included.
1345. Mr Mitchell: I will take that away with me. We can think about the implications, but the new organisation’s support services will not be patient- or client-related.
1346. The Chairperson: I understand your point about responsibilities under section 75, and I wonder why the Northern Board insisted on making that response.
1347. We will formally agree clause 15 later . We will now move on to clause 16, which deals with the patient and client council.
1348. Mr McMaster: Clause 16 establishes a new body to be known as the patient and client council, which will replace the four existing health and social services councils. Its function is explained in clause 17; however, it will deal primarily with patient and client representation in the new system. It introduces schedule 4, which deals with the status, membership and construction of the new body. Schedule 4 is almost the same as schedule 3, which is about the creation of the regional support services organisation. Details about appointments, tenure of office and the constitution of committees will be provided for in subordinate legislation, which will come before this Committee at some stage.
1349. The Chairperson: We will formally agree clause 16 and schedule 4 at a later stage. That brings the Committee to clause 17, which deals with the functions of the patient and client council. Will you briefly talk members through that clause, Ivan?
1350. Mr McMaster: Clause 17(1) sets out the four main functions of the proposed patient and client council, which include representing the interests of the public. That involves ascertaining the views of the public and ensuring that their views are conveyed accurately. It must be noted that they should be the public’s views and not those of the staff of the patient and client council.
1351. Clause 17(1)(b) states that the patient and client council will have a role in “promoting involvement of the public”. That refers to the active role that the body must play in encouraging people to become involved in such things as consultation exercises and other processes that lead to decisions that may affect the public’s health and social well-being.
1352. Clause 17(1)(c) explains the council’s role in providing assistance to individuals who seek help with complaints against health and social care bodies.
1353. The council will also engage in “promoting the provision” of advice and information in relation to health and social care bodies. It should be noted that the intention contained in clause 17(1)(d) is not necessarily that the patient and client council prepares and issues advice but that it should proactively encourage and drive other bodies to get out information on appropriate matters.
1354. Clause 17(1)(e) refers to “such other functions” as the Department would take a power to prescribe by regulations. That provides some flexibility to add other functions to the first four paragraphs that I have explained.
1355. Clause 17(2) gives more detail about the issue of representing the public. Similarly, clause 17(3) provides further detail about the function of promoting the involvement of the public. Likewise, clause 17(4) gives more information about the function of providing assistance to individuals making complaints. Clause 17(5) requires the patient and client council to seek examples from any source of “best methods and practices” in order to promote the participation of the public in how health and social care is designed, commissioned and delivered.
1356. Clause 17(6) reverts back to clause 17(2)(b), which requires the patient and client council to consult with the public. Clause 17(6) also requires the patient and client council to report publicly on any issues on which it has consulted.
1357. Clause 17(7) defines “the public” as widely as people may wish to interpret it. The clause is simply there in order to clarify that “public” may refer to:
“individuals, a group or community of people and a section of the public”.
1358. Clause 17(8) lists the bodies to which the provisions of clauses 17, 18 and 19 apply. Clause 18 deals with the duty to co-operate with the patient and client council, and clause 19 deals with public involvement and consultation. All the health and social care bodies that are referred to in the Bill are on that list, with the exception of the regional support services organisation and the Regulation and Quality Improvement Authority. That is mainly because those bodies do not provide services to the general public.
1359. Clause 17(9) clarifies what is meant by the phrase, a body which is:
“responsible for health and social care”.
1360. If the Committee wishes, I will deal with issues related to that.
1361. Mrs McGill: Disability Action is concerned that disabled people can be excluded from consultation, and it suggests adding the words “in an accessible way” to clause 17(2)(a), so that it would read:
“consult the public in an accessible way about matters relating to health and social care.”
1362. Mr McMaster: Like any public body, the patient and client council falls under the requirements of section 75 of the Northern Ireland Act 1998, and, therefore, it is bound to ensure that no member or part of the community is excluded from any consultation.
1363. Mrs McGill: I quoted what Disability Action said, and I do not want to ignore that. That organisation did not make that point because it believes that consultation is always accessible.
1364. The Chairperson: That issue is also raised by Disability Action’s second point.
1365. Mrs McGill: In its response to clause 17(4), Disability Action states:
“It needs to be clarified if this clause refers to reasonable adjustments under the Disability Discrimination Act or not.”
1366. The Chairperson: I presume that the officials will take those points away for consideration and that they will come back to the Committee when we get to the stage of formally agreeing the clause.
1367. We will now move on to clause 18, which deals with the duty to co-operate with the patient and client council.
1368. Mr McMaster: Clause 18 is intended to place some sense of duty on the bodies to co-operate with the patient and client council in the carrying out of its functions and, for the first time, to put that requirement in statute. Up until now, there has been an almost tacit agreement that the bodies will co-operate with the patient and client council. Clause 18 puts that into statute.
1369. Clause 18(1) places an onus on the health and social care bodies to co-operate. The Bill does not define “co-operate”; the definition is as broad or narrow as it can be taken. Clause 18(2) states:
“In particular, such a body must —
(a) consult the Patient and Client Council with respect to such matters, and on such occasions, as the body considers appropriate”.
1370. We considered that the consultation should be on such matters as the patient and client council considered appropriate. To do that, however, would run the risk of tying the body up in consultation all the time, so it was felt that leaving it to the body to consult with the patient and client council as it considers appropriate was the right way to go. The patient and client council has the option of asking the Department to take action if it believes that the bodies are not playing the game.
1371. Clause 18(2)(b) places a duty on the bodies to furnish to the council — in this case, the patient and client council — with such information that it considers necessary. It is considered that that provision of information would not tie up the body to the same extent that formal consultations would. Therefore, it should provide information that the patient and client council considers to be appropriate.
1372. Clause 18(3) provides that, in order for the patient and client council to carry out its functions effectively, officers will need to have access to premises that are controlled by health and social care bodies and, indeed, certain other bodies. Clause 18(4) sets out the other types of premises that the patient and client council are entitled to enter, in addition to those of the health and social care bodies. Those are other buildings that belong to them, such as surgeries, pharmacies and opticians.
1373. Clause 18(5) confirms a limitation on that right to enter. The right to enter is limited to allowing the patient and client council to carry out its functions. In other words, it cannot use that right to do anything it likes on those premises; it is limited to carrying out its functions of representing the interests of the public and promoting the public’s involvement in health.
1374. Clause 18(6) explains that health and social care bodies must have regard to the views expressed by the patient and client council. The phrase “have regard to” means that those bodies must think strongly about those views, and only where there are strong reasons for doing otherwise should they not agree with the patient and client council.
1375. Dr Deeny: I prefer the expression “patient council” over “client council”; I do not like the word “client”. One need not be sick in order to be called a patient. I have 8,200 patients, not clients.
1376. I am concerned about clause 18(1):
“A body to which this section applies must co-operate with the Patient and Client Council in the exercise by the Council of its functions.”
1377. That is too general. What is meant by a “body”? Does that include, for example, the trusts, local commissioning groups, agencies, boards and, indeed, the Department?
1378. Mr McMaster: Yes, it does. Clause 17(8) states:
“This section and sections 18 and 19 apply to —
(a) the Department;
(b) the Regional Board;
(c) RAPHSW;
(d) HSC trusts; and
(e) special agencies.”
1379. Dr Deeny: They must all co-operate.
1380. Clause 18(6) states:
“A body to which this section applies shall have regard to any views expressed by the Patient and Client Council”.
1381. To “have regard to any views” is non-committal; I might have regard for your views, but then say to hell with them. I suggest that the phrase:
“and act on any views expressed”
1382. should be inserted. There is no point in having regard to any views expressed — perhaps on behalf of the public and perhaps making suggestions about what healthcare the public requires — by the patient and client and council. Inserting the phrase that I suggested would mean that some action will be taken rather than merely listening to opinions.
1383. The Chairperson: Perhaps it should say “due” regard, which would mean that one could have input, even though that input may not be correct. Kieran’s suggestion implies that someone’s input should be acted on even if it is incorrect. “Due” regard would address that point but retain discretion.
1384. Mr McMaster: We will certainly consider that.
1385. The Chairperson: We will formally agree the clause later. We will move on to clause 19, which concerns public involvement and consultation.
1386. Mr McMaster: Clause 19 will apply to the same list of bodies. It is about public involvement in the planning and delivery of statutory services, and it places a duty on bodies to provide information, to research the population’s requirements and to encourage and assist people. In particular, health and social care bodies will be required to demonstrate, by producing a consultation scheme, how they intend to consult with the public about service provision. It will not be sufficient for such bodies to wait to be asked; they will have to publish information proactively about requirements and make that information known to the public. Users to whom care is provided will have to be proactively told about services and encouraged and assisted to use them appropriately. That obligation is about promoting cost-effectiveness in the health- and social-care system — for example, if the assistance required by patients can be provided cheaper by their consulting with pharmacists rather than with GPs, such means must be encouraged.
1387. Given that prevention is better than cure, bodies will be required to encourage and assist people to help themselves mentally and physically, and to be aware of how to look after themselves, using diet, fitness and self-examination.
1388. Clause 19(2) places a statutory duty on each body to produce a consultation scheme within nine months of the day appointed, and to send that consultation scheme to the Department, which will then examine the scheme and decide whether to approve it.
1389. Mrs McGill: Disability Action suggests that, in clause 19(1)(a), the words “in accessible formats” should be inserted so that it reads:
“to promulgate information, in accessible formats”.
1390. Perhaps you could consider that when you are looking at the Disability Discrimination Act 2005.
1391. The Chairperson: Ivan, apart from that, we are in agreement. We will formally agree the clause later.
1392. We will now move on to clause 20, which deals with public involvement and consultation schemes.
1393. Mr McMaster: The main function of clause 20 is to provide some detail on the consultation schemes. It specifies that the scheme must show clearly what arrangements the body will employ to canvas the views of the patient and client council and service users, or their representatives — including their carers — on matters specified in clause 20(2) relating to health and social care. Those matters are: the planning of how the services are to be provided — that is, the nature and delivery of the service; the development and consideration of change, however big or small, and the way in which those services are provided; and operational decisions around the delivery of that care, which will include such factors as surgery opening hours, for instance.
1394. Clause 20(3) provides details on what a health and social care body to which this clause applies must do with the responses. It must have regard to those comments, and I appreciate that the Committee has concerns about the phrase “have regard to”. The body must also prepare a written statement that sums up all the comments received and sets out the body’s response to the comments.
1395. Clause 20(4) states that the consultation scheme must provide that the body to which it is to apply will give adequate publicity to the statement. In other words, it is not enough for the body to make a mere statement; it must publicise the fact that it has made a statement on the issues raised.
1396. The Chairperson: We will formally agree the clause later. We now move on to clause 21, which deals with the duty on health and social care trusts in relation to improvement of health and social well-being.
1397. Mr McMaster: In general, the Bill bestows a number of functions on all the newly established bodies that directly or indirectly provide health and social care. Amid all the other competing priorities, it is important that the organisations do not lose sight of the overarching drive for improvements in health and social well-being.
1398. Those duties already apply to the Department, because it has a general duty of care under clause 2 of the Bill. It also applies to the regional board, because it is charged with carrying out the Department’s general duties. It also applies to the regional agency, as is mentioned in clause 13(2)(a), which states that the agency is to develop and secure programmes designed to secure the improvement of health and well-being.
1399. Clause 21 ensures that the overarching desire to secure such improvements is an integral part of the work of the trusts, despite any competing priorities that those trusts might have. It makes it clear that trusts, in the exercise of their functions, must also do this:
“with the aim of improving the health and social well-being of those for whom it provides”.
1400. Bernard referred to clause 21 earlier.
1401. Mrs McGill: The Community Development and Health Network has asked that, in clause 21, the words: “and reducing health inequalities between”
1402. be inserted so that it would read:
“It is the duty of an HSC trust to exercise its functions with the aim of improving the health and social well-being of, and reducing health inequalities between, those for whom it provides, or may provide, health and social care.”
1403. That goes back to the issue of inequalities that were previously discussed. Could that insertion be considered?
1404. The Chairperson: Would that be absorbed under section 75?
1405. Mr McMaster: Yes, but it is one of a number of responses that you have asked us to consider.
1406. The Chairperson: We will formally agree the clause later. We move on now to clause 22, which deals with public-private partnerships.
1407. Mr McMaster: Clause 22 provides for the Department, the regional board, the proposed regional agency, the regional support services organisation, special agencies and trusts to participate in public-private partnerships (PPPs) with companies to provide facilities or services to persons or bodies. That path is open to all those bodies and the clause is intended as a clarification not an advocation; it is more of a permissive power, and it simply sets out the provisions for that. We are establishing a number of new bodies, and clause 22 simply highlights the fact that public-private partnership is an avenue that is open to them.
1408. The Chairperson: The health and social services councils have some concerns. They:
“believe that this clause should include a reference to ensuring the long-term financial viability and value of any such public-private partnership before entering into it.”
1409. All of us have a major concern about the long-term costs and that it should provide value for money. Perhaps you could take on board that this cannot be a short-term fix that will take a long time to pay back.
1410. Mrs Hanna: Will you clarify if this is a new arrangement? I am very sceptical of PPPs, and certainly will not be ticking the box on anything that increases their number. I do not think that PPPs should be in the Health Service at all, or at least, if they are, absolute best value for money must be demonstrated. Will you explain again what is happening?
1411. Mr McMaster: Trusts have some legislative provisions for PPPs, but I cannot honestly tell you which pieces of legislation they are. We are establishing a new structure, and the purpose of clause 22 is to make it clear that public-private partnerships are a viable option, and to which bodies that will be applied. At the moment, trusts can enter into those partnerships.
1412. Mrs Hanna: Does clause 22 clarify that they have the power to make that decision?
1413. Mr McMaster: It clarifies that not only trusts but other bodies have the power to enter into public-private partnerships.
1414. Mrs Hanna: Have they always had that power?
1415. Mr McMaster: They have always had that power.
1416. Mrs Hanna: I thought that the Department would have taken that decision.
1417. Mr McMaster: No; at the moment, there are some powers directly bestowed on the trusts to do that.
1418. Mr Mitchell: My understanding of clause 22 is that it eliminates any uncertainty. Those bodies listed have the legal right to enter into an appropriate private-finance arrangement, subject to passing those hurdles that the Chairperson mentioned. Any arrangement will have to be as a result of a business case, be best value for money and pass all those hurdles. There was no particular scheme in mind when this proposal was; it was proposed to avoid doubt. If the service needs to use a scheme such as this, it has to be quite clear to the bodies, and to the private sector with which they are dealing, that there is a legal basis for that partnership. That is the only reason that the clause is here.
1419. Mrs Hanna: There is concern about clause 22; may we leave it until next week? We are supposed to be making things clearer, but, as somebody who is opposed to PPPs, if I tick that box, I am saying that PPPs are fine. Tommy Gallagher is not here, and, if he were, he would also want to comment on clause 22.
1420. The Chairperson: We can agree on that next week. We will now move on to clause 23, which deals with schemes for the transfer of assets and liabilities.
1421. Mr McMaster: The simplest way of explaining clause 23 is that, in some cases, it requires the Department, and, in other cases, gives the Department the power to make schemes that provide for the transfer of assets and liabilities. That includes the transfer of staff from the bodies that are being dissolved and subsumed into the new organisations.
1422. Clause 23(4) is important, because it extends the Department’s powers to make one or more schemes “at any time” for the transfer of designated assets or liabilities. Under Clause 23(2), the Department must have schemes in place into which it can transfer the assets and liabilities of the bodies that it dissolves now, whereas clause 23(4) provides for adjustments that we may have to make at some stage in the future. It confers the power, if needed in the future, to make further schemes for the transfer of designated assets to the health and social care bodies.
1423. Schedule 5, which I will address with clause 23, contains further detail and clarification about those transfer schemes. Paragraph 2 of schedule 5 deals with the transfer of employed staff. Paragraph 2(2) states that the Transfer of Undertakings (Protection of Employment) Regulations 2006 — known as the TUPE regulations — will apply to transferring employees.
1424. Paragraph 2(3) of schedule 5 states:
“The scheme shall —
(a) in relation to each transferee, identify the transferring employees (whether by name or otherwise);
(b) include provision securing pension protection for such employees;
(c) include provision for procedures designed to resolve any grievances of such employees arsing in relation to matters dealt with by the scheme; and
(d) include provision for the payment of compensation by the Department to any such employee who suffers loss or detriment in consequence of the scheme.”
1425. Paragraph 2(4) of schedule 5 states:
“Before making the scheme the Department must consult —
(a) in the case of a scheme which identifies transferring employees by name, those employees”.
1426. Paragraph 4 of schedule 5 deals with the completion of accounts and reports of dissolved bodies. Obviously, those bodies will not exist after April 2009 so their accounts must be completed by someone. The accounts of the four health and social services boards will be completed by the proposed new regional board. The Central Service Agency’s accounts will be completed by the regional support services organisation, or whatever it will be called in the future, and the Mental Health Commission’s reports will be completed by the RQIA. Paragraph 4 provides a continuation of those types of issues following the transfer of staff and assets.
1427. The Chairperson: We will formally agree clause 23 and schedule 5 later. We will move on to clause 24, which deals with the transfer of functions of the health and social services boards.
1428. Mr McMaster: Clause 24 provides for the transfer of functions of the existing health and social services boards. After the date of transfer, functions that relate to health-improvement functions or health protection will be exercisable by the agency.
1429. The Chairperson: We will formally agree clause 24 later. Ivan, will you explain the purpose of clause 25?
1430. Mr McMaster: Clause 25 provides for the transfer of functions from the Mental Health Commission to the RQIA.
1431. The Chairperson: We will formally agree clause 25 later. Will you explain the purpose of clause 26?
1432. Mr McMaster: Clause 26 provides for the transfer of functions from the Central Services Agency to the new regional support services organisation. However, clause 26(3) states:
“The Department may by order provide that subsection (1) is not to apply to any specified function.”
1433. The Chairperson: We will formally agree clause 26 later. We will move on to clause 27, which provides for the amendment of statutory and other references to dissolved bodies.
1434. Mr McMaster: Clause 27 deals with any references in legislation to the bodies that are being dissolved. Throughout legislation there are numerous mentions to the health and social services boards, and the other bodies that are being dissolved. Therefore, clause 27 grants generic provision for those references to be construed as references to the new bodies.
1435. Clause 27(2) states:
“In relation to any time after the transfer date, any reference in any statutory provision or document to a Health and Social Services Board (whether general or particular) shall —
(a) in relation to any function transferred by section 24(1), be construed as a reference to RAPHSW;
(b) in relation to any function transferred by section 24(2), be construed as a reference to the Regional Board.”
1436. The same applies for references to the Central Services Agency and the Mental Health Commission for Northern Ireland. The clause provides for a generic way of correcting those references rather than our having to amend every single one.
1437. The Chairperson: We will formally agree clause 27 later. We will now move on to clause 28, which deals with the dissolution of special agencies.
1438. Mr McMaster: Under clause 28, two special agencies are being dissolved — the Health Promotion Agency and the Northern Ireland Regional Medical Physics Agency. Those agencies were established under the Health and Personal Social Services (Special Agencies) (Northern Ireland) Order 1990. However, when we were formulating the Bill, we discovered that the provisions of that Order were defective and did not contain a power that allowed us to transfer the assets and liabilities of those special agencies; the agencies could be wound up, but we could not do anything with their assets or liabilities. Therefore, clause 28 is an amendment to that Order that allows us the capacity to make that transfer.
1439. The Chairperson: We will formally agree clause 28 later. We will now move on to clause 29, which deals with orders, regulations, guidance and directions.
1440. Mr McMaster: Clause 29 outlines what sort of procedure should be used in respect of the subordinate legislation Orders, regulations and directions. For example, clause 29(1) relates to instances when the functions of the regional agency or the regional support services organisation are altered, or when an Order is made that allows a Department to do something that will give full effect to the Bill. Such Orders cannot be made until they are laid before, and approved by resolution of, the Assembly. In general, regulations are made through negative resolution and will, at some stage, come before the Committee. Therefore, clause 29 outlines a technical procedure that allows such Orders to be made.
1441. The Chairperson: You have mentioned regulations being made subject to negative resolution; was any consideration given to affirmative resolution in relation to clause 29(2)?
1442. Mr McMaster: At the moment, the provision is for negative resolution.
1443. Clause 24(4) relates to instances when the functions of the health and social services boards will not be split as is specified in the Bill, and clause 26(3) relates to instances when the functions of the Central Services Agency will not be as directed in the Bill. The Bill states that the functions of the health and social services boards will, generally, be split between the regional agency and the regional board and that, broadly, the functions of the Central Services Agency will go to the regional support services organisation. Those regulations relate to instances when the contrary would apply. As the Bill is drafted, that would be done by negative resolution.
1444. The Chairperson: Will you humour me and tease out when it might be regulations as opposed to Orders — can you explain that to me, please?
1445. Mr McMaster: No, I cannot. [Laughter.]
1446. The Chairperson: Good grief.
1447. Mr McMaster: That is the draftsman in me. They are both pieces of subordinate legislation that confer different powers. I will come back with clarity on that for you next week, if you wish.
1448. The Chairperson: Yes, please do that. We will leave that until next week. We will now move on to clause 30, which relates to further provision.
1449. Mr McMaster: Clause 30 is a general provision in the Bill. It allows the Department to make, by subordinate legislation, any provisions that it feels are necessary to give effect to the Bill. It provides for instances when it is found that something has, accidentally, been left out of the Bill. Rather than producing a piece of primary legislation to provide for something that has been missed out when the Bill was formulated, it allows us to provide for that by subordinate legislation. Such subordinate legislation will still come before the Committee; it is simply a quicker method of ensuring that what we want to happen will happen on time. It has been included just in case we have forgotten bits and pieces, which we all do.
1450. The Chairperson: Yes; we are all human, we can err. We will formally agree clause 30 later. We will now move on to clause 31, which relates to interpretation.
1451. Mr McMaster: Clause 31 contains a list of definitions for terms that are used in the Bill.
1452. The Chairperson: That is straightforward. We will formally agree clause 31 later. We will now move on to clause 32, which deals with minor and consequential amendments.
1453. Mr McMaster: Clause 32 simply introduces schedule 6, which lists a considerable number of amendments that are consequential to the changes that are being made. It mainly involves the names of organisations, and so on.
1454. The Chairperson: We will formally agree clause 32 later. We will move on to clause 33, which deals with repeals.
1455. Mr McMaster: Clause 33 introduces schedule 7, which deals with legislation that must be repealed. As I said at an earlier meeting, we are not repealing legislation in general, but some specific provisions must be repealed, such as those that establish the boards, the Central Services Agency and the health and social services councils.
1456. The Chairperson: We will formally agree clause 33 later. We will move on to clause 34, which deals with commencement.
1457. Mr McMaster: Clause 34 details when the various provisions of the Bill will come into operation. Those listed at clause 34(1) will come into effect immediately upon Royal Assent. They include: the duties and powers to make schemes in relation to the transfer of assets; the insertions into the Health and Personal Social Services (Special Agencies) (Northern Ireland) Order 1990; and technical provisions that allow for the making of Orders and regulations, and so on. Those provisions need to be in effect from day one.
1458. Subsection 34(2) states:
“The following provisions come into operation on Royal Assent insofar as they confer power to make regulations or orders —”
1459. It goes on to list those provisions. All other provisions will require a commencement Order, which is subordinate legislation that will come before the Committee. The Order will simply state that the provisions will come into effect on a particular date. It may be that the target date for the establishment of the new structures —1 April 2009 — cannot be met, so that provision allows for some flexibility.
1460. The Chairperson: We will formally agree clause 34 later. Clause 35 deals with the short title, which is self-explanatory. We can all grasp that, so there should be no need for any questions. We will formally agree the clause at a later meeting.
1461. We now move on to the remaining schedules. We have already dealt with schedule 5, which covers the transfer of assets, and so on. Schedule 6 deals with minor and consequential amendments.
1462. Mr McMaster: There are a couple of technical changes to schedule 6. Again, there were drafting errors — perhaps I should not call them that; our draftsmen would not particularly like it. At page 53, line 39, paragraph 18(1) provides for an amendment to sections 51(1) and 51(2) of the Health and Personal Social Services Act (Northern Ireland) 2001. It reads:
“in subsections (1) and (2) for ‘or the Agency’ substitute ‘, the Regional Board or RAPHSW’;”.
1463. That line deals with the Central Services Agency, and it should read the “regional support services organisation”. That is a mistake. It does not reflect any change in policy; it should always have mentioned the regional support services organisation, or whatever name it will be given in future.
1464. The Chairperson: That is everything except for schedule 7, which deals with repeals.
1465. Mr McMaster: That schedule simply lists the legislation that we are repealing.
1466. The Chairperson: I do not think that, at this stage, we will start the formal clause-by-clause scrutiny — I see the relief on members’ faces. I thank Ivan, Craig and Bernard for their much-appreciated help in explaining the Bill so clearly. A number of issues were queried, and DV, I hope that we will get more clarification on them. We can then begin to agree each of the clauses and schedules formally. Thank you for your attendance.
23 October 2008
Members present for all or part of the proceedings:
Ms Sue Ramsey (Temporary Chairperson)
Mr Thomas Buchanan
Mr Alex Easton
Mr Tommy Gallagher
Mr Sam Gardiner
Mrs Carmel Hanna
Mr John McCallister
Mrs Claire McGill
Witnesses:
|
Mr Craig Allen |
Department of Health, Social Services and Public Safety |
1467. The Temporary Chairperson (Ms S Ramsey): We now move on to the Committee’s formal clause-by-clause consideration of the Health and Social Care (Reform) Bill.
1468. The Committee Clerk: This is the Committee Stage of the Health and Social Care (Reform) Bill. The Committee must formally consider the Bill’s clauses and agree whether each clause, as it is drafted, should stand. In the past couple of weeks, members have raised concerns about several clauses. The Department agreed to consider whether the Committee’s proposals were acceptable. The Committee can decide to table any proposal that has been rejected by the Department as an amendment at the Bill’s Consideration Stage and include it in the report. It may be useful for the Committee to consider the acceptable clauses today and defer the others until the next meeting.
1469. Mr Buchanan: The Department has accepted some of the Committee’s proposals and rejected others. I ask that the clause-by-clause consideration is deferred until the next meeting so that the Committee has sufficient time to establish what the Department’s problems were with the proposals that it rejected.
1470. Mrs McGill: Are all the issues that the Committee raised — such as my point about equality — dealt with in the correspondence?
1471. Mr Bernard Mitchell (Department of Health, Social Services and Public Safety): To the best of our knowledge, the correspondence that has been provided to the Committee covers every point that was raised. We have highlighted a couple of additional items for the Committee’s attention. We have tried to ensure that the Department’s letter to the Committee, dated 22 October, is comprehensive and that there are no surprises for the Committee.
1472. Mrs McGill: Did we just get that letter now?
1473. The Temporary Chairperson: Yes, we did.
1474. Let me clarify the situation. There are some clauses in the Bill that the Committee had concerns about and wished to amend. The Department has accepted some of those amendments and rejected others. The first suggestion is that we deal with the non-contentious clauses and defer the others until a later date. The other proposal is that we defer everything today.
1475. Mr Gallagher: I am happy to deal with the non-contentious clauses today.
1476. The Temporary Chairperson: We are under pressure to complete the Committee Stage of the Bill.
1477. Mr Gardiner: If that is the case, we should deal with the amendments that the Department has accepted and not hold the Bill back.
1478. Mr Buchanan: We have continuously raised the issue of the regional agency. I do not see anything on the list of recommendations from the Department that suggests that it has either accepted or rejected our proposal on that issue. I made the point very strongly that there was no need for such an agency and that its functions could be carried out by the regional board.
1479. The Temporary Chairperson: We will not even discuss that clause today, because it is contentious.
1480. Mr Buchanan: If I can have an assurance that the issue will be discussed at a later date, I will be happy to defer it today.
1481. The Temporary Chairperson: Bernard, I am suggesting that we deal with the non-contentious clauses.
1482. Mrs McGill: I raised several concerns about disability-related matters. Issues were raised by Disability Action, if I remember correctly. I have not had time to consider these amendments. I know that the Department has rejected some of them.
1483. The Temporary Chairperson: That is the Department’s job now. It will report back and let us know which amendments it has accepted or rejected.
1484. Mrs McGill: Is that in front of us? I see no point in a process in which a Department, or any Government body, asks organisations such as Disability Action to respond to a consultation, and a member of the Committee picks up on that response and raises it with departmental officials. A paper then comes before me, but I cannot see what the situation is; it is too rushed for me. Such a paper might be brilliant, but I do not see any point in asking organisations such as Disability Action for their views. I mention Disability Action only because I remember raising a couple of points about disability and equality.
1485. The Temporary Chairperson: Let me just clear things up for the record. Several concerns have been raised in the past few weeks by members of the Committee and by respondents to the consultation. What we now propose to do is deal with the amendments that the Department has accepted. The amendments that have been rejected by the Department will not be dealt with today. We will defer discussion of those amendments.
1486. Mr Mitchell: I will clarify things from our perspective. We were asked to present a separate paper with some additional facts on the issue of the regional agency. We have done that. It is not that we are trying to avoid the issue.
1487. We expect that to be discussed under the heading of the separate paper. The issues from Disability Action to which you are referring are issues that we have not accepted, so they would be deferred for discussion at a later date.
1488. Where the Department has not accepted recommendations, generally — not exclusively — the only two reasons for rejection are because the draftsman has told us that he thinks that there are difficulties with the form of wording that is being proposed or that the issue is covered by other legislation, and, consequently, we think that it would result in duplication if it were to be included in the Health and Social Care (Reform) Bill. I am happy that we get the chance to discuss those points one by one, including the issue of the agency.
Clause 1 (Restructuring of administration of health and social care)
1489. The Temporary Chairperson: Issues were raised about clause 1; the Department has rejected one of the Committee’s recommendations.
1490. Mr Ivan McMaster (Department of Health, Social Services and Public Safety): There were two issues about clause 1. The suggestion that the agency be called the “health and social care RQIA” has been rejected; the suggestion that the acronym RAPHSW is unwieldy and should be altered has been accepted. May we refer the clause?
1491. Clause 1 referred for further consideration.
1492. Clauses 2 and 3 agreed to.
Clause 4 (Department’s priorities and objectives)
1493. The Temporary Chairperson: It was suggested that the word “extreme” be inserted before “urgency”, and the Department’s recommendation is that it be rejected.
1494. Clause 4 referred for further consideration.
Clause 5 (The framework document)
1495. Mr McMaster: The existing wording in clause 5(5)(b) is that the Department “may consult”, but the suggestion was made that the wording be changed to the Department “will consult”. The Department accepts that.
1496. Mr Gallagher: Does this clause refer only to the Department?
1497. Mr McMaster: Yes, it does. The Department:
“may consult any other bodies or persons the Department considers appropriate.”
1498. The suggestion was that “may” should be changed to “will”, and we accept that.
1499. Mr Gallagher: At some point, I raised concern about the trusts’ duty to consult with the users. Is that something that comes up in the regulations?
1500. Mr Mitchell: There is a legislative requirement for all the bodies to produce a consultation scheme that indicates how they would consult with service users and other stakeholders. That is provided for.
1501. Mr Gallagher: It would be useful to know where that is.
1502. Mr Mitchell: That is in clause 20.
1503. Mr McMaster: There are issues to be raised when we get to that clause.
1504. Mr Gallagher: We can leave those issues until we reach that stage in consideration.
1505. The Temporary Chairperson: The Department has agreed to accept the recommendation from the Committee.
1506. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1507. Clause 5, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
1508. Clause 6 referred for further consideration.
1509. Clause 7 agreed to.
Clause 8 (Functions of the Regional Board)
1510. The Temporary Chairperson: During previous discussions, members were otherwise content with this clause as drafted, but there was an issue about the Minister’s views on joint sign-off.
1511. Mr Mitchell: The Department was keen to ensure that there will be no surprises for members when the Bill is presented. The Department has stated a couple of times that it is considering a joint sign-off. The fact that that was happening was merely being put on the record, and a form of words was being sought on the issue.
1512. Clause 8 referred for further consideration.
Clause 9 (Local Commissioning Groups)
1513. The Temporary Chairperson: Members were concerned about the wording of clause 9(4)(b)(i), which states that the groups must:
“consult RAPHSW and have due regard to any advice or information provided by it”.
1514. Officials had agreed to consider a call from the Royal College of Nursing (RCN) to strengthen that provision. The Department is recommending that the Committee accepts clause 9(4)(b)(i) with an amended form of wording. Bernard, will you explain that?
1515. Mr Mitchell: Michelle O’Neill presented, on behalf of the RCN, a form of wording that included what, for me, was the most important part — that local commissioning groups must work in partnership with the regional agency. The Department has consulted with the legislative draftsman, and a form of words has been produced that I hope addresses that point while at the same time embracing the requirement to have due regard to the advice and information provided by the agency. In all fairness, since the point was raised by Michelle, the Committee may wish to consider her view on that.
1516. Clause 9 referred for further consideration.
1517. Clauses 10 and 11 agreed to.
Clause 12 (The Regional Agency for Public Health and Social Well-being)
1518. The Temporary Chairperson: Is Thomas Buchanan not here? The Committee should slide in clause 12 while he is not here. [Laughter.] I am joking.
1519. Mr Gardiner: Will that be done on the Temporary Chairperson’s recommendation? [Laughter.]
1520. Clause 12 referred for further consideration.
Clause 13 (Functions of RAPHSW)
1521. The Temporary Chairperson: During previous discussions, members raised questions about clause 13(2)(b) — health promotion — and suggested that a new provision be included in clause 13(4)(e), which requires that the RAPHSW:
“make available to any other body such persons, materials and facilities as it thinks appropriate”.
1522. The Department has agreed to accept that, in relation to clause 13(2)(b), officials will suggest a wording along the following lines to the legislative draftsmen:
“the health promotion function is the process of enabling people to increase control over, and to improve, their health and social well-being”.
1523. However, the Department rejected a suggestion to include the words:
“including the Assembly Health, Social Services and Public Safety Committee”
1524. after the words “any body” in clause 13(4)(e), which states that the RAPHSW may:
“make available to any other body such persons, materials and facilities as it thinks appropriate”.
1525. Clause 13 referred for further consideration.
Clause 14 (The Regional Support Services Organisation)
1526. The Temporary Chairperson: Members were content with clause 14 and its related schedule, apart from the name of the proposed body, which the Committee wants to call the “regional business services organisation”. The Department’s response is that it would consider a change in the name of the organisation to the “regional business support organisation”.
1527. The Committee Clerk: The current name used in the Bill is the “regional support services organisation”; the suggestion from the Committee was “regional business services organisation”.
1528. Mr Mitchell: The Department accepts that suggestion.
1529. The Committee Clerk: I am sorry, your letter of response states that the Department will accept the name “regional business support organisation”?
1530. Mr Mitchell: That is a typo. It should read “regional business services organisation”.
1531. The Temporary Chairperson: So we were right.
1532. Mr Mitchell: You were right, and we were wrong.
1533. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1534. Clause 14, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 15 (Functions of RSSO)
1535. The Temporary Chairperson: The wording of clause 15(3)(a) was mentioned last week. It relates to the inclusion of the word “equitable” alongside “economic, efficient and effective”.
1536. Clause 15 referred for further consideration.
1537. Clause 16 agreed to.
Clause 17 (Functions of the Patient and Client Council)
1538. The Temporary Chairperson: During previous discussions, members highlighted the concerns raised by Disability Action relating to the clause.
1539. Clause 17 referred for further consideration.
Clause 18 (Duty to co-operate with the Patient and Client Council)
1540. The Temporary Chairperson: The officials agreed to consider the recommendations, and they have accepted our suggestion to change “have regard to” to “have due regard to”.
1541. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1542. Clause 18, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 19 (Public involvement and consultation)
1543. The Temporary Chairperson: During previous discussions, members were content with the clause as presently drafted apart from a question in relation to clause 19(1)(a) about the provision of information. The Department has agreed to reject it, so we will defer it.
1544. Clause 19 referred for further consideration.
Clause 20 (Public involvement: consultation schemes)
1545. The Temporary Chairperson: During previous discussions, members were content with the clause as presently drafted. Have officials given any consideration to the change in wording from “have regard to” to “have due regard to”?
1546. Mr McMaster: When we were going through the Bill, the change in wording was not mentioned. However, for consistency, we feel that the words “to have regard” in clause 20(3)(a) should be changed to read “to have due regard”.
1547. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1548. Clause 20, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 21 (Duty on HSC trusts in relation to improvement of health and social well-being)
1549. The Temporary Chairperson: The Department has agreed to accept our recommendations.
1550. Mr Gallagher: What were our recommendations?
1551. The Temporary Chairperson: During previous discussions, members had suggested the inclusion of a reference to reducing health inequalities, and officials agreed to consider that further. A suggestion has been made to include “and reducing health inequalities” after the words “health and social well-being”.
1552. Mr Gallagher: It is the trusts’ duty to consult with the people for whom they provide the services. Is that included?
1553. Mr McMaster: In common with the organisations that we are creating under the legislation, the trusts will have an obligation to complete a consultation scheme that will show how they will consult with the people for whom they provide the services. They are required to submit a scheme to the Department in nine months; we will scrutinise and approve that scheme if it is suitable.
1554. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1555. Clause 21, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 22 (Public-private partnerships)
1556. The Temporary Chairperson: During previous discussions, members expressed concern about the principle of public-private partnerships.
1557. Mrs Hanna: In clause 22, is it possible to include appropriate wording to reflect some members’ concerns generally about PFIs, and not just in cases into which public-private partnership is to be entered? I accept the Department’s formal response to the Committee’s suggestion, but is it possible to include appropriate wording to reflect some members’ general concerns about PFIs?
1558. The Temporary Chairperson: If members still have concerns about that issue, we will refer the clause.
1559. Mr McMaster: Do you want that to be included in the legislation?
1560. Mrs Hanna: Is that possible? I understand that it might not be, because it is a principle.
1561. The Temporary Chairperson: Will the Department examine whether that is possible?
1562. Mrs Hanna: We can refer that clause until the next time.
1563. Clause 22 referred for further consideration.
Clause 23 (Schemes for the transfer of assets and liabilities)
1564. Mr McMaster: When we re-examined schedule 5, we discovered that an explanation was missing. Schedule 5 provides the details of schemes whereby staff are transferred. It also lists the three types of bodies that should not be present at any hearing of resolution of disputes.
1565. When schedule 5 was initially drafted, we thought that we did not need to include the transferor body — the body from which employees are transferred — because we considered that those bodies would be done away with on day one. However, employees may be transferred after that date. Therefore, we will include the appropriate wording in schedule 5 to ensure that a body from which employees are transferred is not involved in any dispute resolution. That will bring the Bill into line with the Libraries Act (Northern Ireland) 2008.
1566. Question, That the Committee is content with the clause, put and agreed to.
1567. Clause 23 agreed to.
1568. Clauses 24 to 28 agreed to.
Clause 29 (Orders, regulations, guidance and directions)
1569. The Temporary Chairperson: The Committee has received further information from the Examiner of Statutory Rules since the Department’s paper. Therefore, I suggest that we refer clause 29.
1570. Clause 29 referred for further consideration.
1571. Clauses 30 and 31 agreed to.
Clause 32 (Minor and consequential amendments)
1572. The Temporary Chairperson: Officials have explained that some technical changes must be made to schedule 6.
1573. Question, That the Committee is content with the clause, put and agreed to.
1574. Clause 32 agreed to.
1575. Clauses 33 to 35 agreed to.
1576. Schedule 3 agreed to.
1577. Schedule 4 agreed to.
1578. Schedule 5 referred for further consideration.
1579. Schedule 6 referred for further consideration.
1580. Schedule 7 agreed to.
1581. The Temporary Chairperson: I would love to say that that concludes the Bill’s formal clause-by-clause scrutiny; however, it does not, because several clauses have been referred for further consideration. Nevertheless, thank you for your patience, and we shall return to those matters at the next meeting.
1582. Mr Mitchell: Would it be helpful if the Department drew up a paper for the next meeting, outlining any referred matters and changes that were suggested during this discussion?
1583. The Temporary Chairperson: Yes, that would be helpful.
1584. Mrs McGill: Will members receive that paper in advance of the next Committee meeting?
1585. Mr Mitchell: You will. The turnaround time did not permit earlier submission on this occasion.
1586. The Temporary Chairperson: We will be in recess for a week.
1587. Mr Mitchell: Do you require any further information on, for example, agency matters? Should we bring any additional material?
1588. The Temporary Chairperson: No, but we will get in touch with you if we require anything further. Thank you for attending today.
6 November 2008
Members present for all or part of the proceedings:
Mrs Iris Robinson (Chairperson)
Mrs Michelle O’Neill (Deputy Chairperson)
Dr Kieran Deeny
Mr Alex Easton
Mr Tommy Gallagher
Mrs Carmel Hanna
Mr John McCallister
Ms Sue Ramsey
Witnesses:
|
Mr Craig Allen |
Department of Health, Social Services and Public Safety |
1589. The Chairperson (Mrs I Robinson): We now move to the clause-by-clause consideration of the Health and Social Care (Reform) Bill. I welcome Bernard Mitchell, Ivan McMaster, Craig Allen and the Chief Nursing Officer, Martin Bradley. At last week’s meeting, the Committee agreed the non-contentious clauses and those where our proposals were accepted by the Department.
1590. We will consider the remaining 12 clauses and three schedules. The Department has not accepted — or fully accepted — our proposals regarding those clauses. After listening to the views of the Department, the Committee must decide whether it is content with each clause as it is drafted or agree amendments that will be included in the Committee’s report and tabled for debate at the Bill’s Consideration Stage.
1591. Members will be aware that the Assembly agreed to grant a short extension to the period in which the Committee Stage must be completed. However, I strongly suggest that we complete the Bill’s clause-by-clause consideration today. The Committee’s report will be prepared after the meeting.
1592. The papers that have been provided for members include a follow-up letter from the British Medical Association (BMA) about the evidence session that took place on 2 October; a revised version of the Department’s response to the various clauses; the Hansard reports of previous meetings; and a briefing paper from the Examiner of Statutory Rules.
Clause 1 (Restructuring of administration of health and social care)
1593. The Chairperson: Officials outlined the meaning of clause 1 at a previous meeting. It deals with the generality of the restructuring of the organisations and the bodies that will be dissolved. Clause 1 also provides for several bodies’ names to be changed and defines the proposed health and social care bodies.
1594. Members raised two concerns about clause 1 during the previous discussions. The first of those concerns regarded the use of the initialism “RQIA” — to refer to the health and social care regulation and quality improvement authority — in clause 1(2)(b) and throughout the Bill. The Committee suggested that the abbreviation “health and social care RQIA” should be used instead. The Committee also regarded the initialism “RAPHSW” — to refer to the proposed regional agency for public health and social well-being — as cumbersome.
1595. I invite the officials to brief the Committee on the Department’s response to those concerns.
1596. Mr Ivan McMaster (Department of Health, Social Services and Public Safety): After discussions with the Office of the Legislative Counsel, the Department felt that the initialism “RQIA” should continue to be used throughout the Bill. Initialisms and acronyms are designed to provide a shortened version of terms. We do not feel that the term “health and social care RQIA” fulfils that purpose. In any case, RQIA is a widely accepted initialism.
1597. The Chairperson: Therefore, the Department does not accept the Committee’s first suggestion.
1598. Mr McMaster: The Department agreed that the initialism “RAPHSW” is something of a tongue-twister. We propose that the term “regional agency” should be used in its place throughout the Bill.
1599. The Chairperson: One of the Committee’s two recommendations was accepted. I suppose that that is not a bad outcome.
1600. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1601. Clause 1, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 4 (Department’s priorities and objectives)
1602. The Chairperson: Officials explained that clause 4 will make it a statutory requirement for the Department to determine its priorities and objectives for the provision of health and social care regularly. The Department can revise those priorities and objectives, but it must consult with the bodies in question before doing so.
1603. Officials also pointed out that clause 4(3) releases the Department from the obligation to consult when urgent action is required, and there is no time for consultation. Members had concerns about that provision and asked the officials to consider two possible amendments. First, the word “extreme” should be inserted to make the clause read thus:
“because of the extreme urgency of the matter”.
1604. Secondly, the Department should be required to report and review instances retrospectively when it acted without consultation because of the urgency of the situation. I again invite officials to brief the Committee on the Department’s response to those points.
1605. Mr McMaster: We propose to reject the suggestion that the phrase “extremely urgent” should be used. The difficulties concern the definition of the word “extremely” and trying to separate that from “urgent”. More importantly, if a provision is included that exempts the Department from consulting in extremely urgent cases, it means that we would have to consult in ordinary urgent cases, which seems to defeat the purpose of the provision in the first place. It is because of that difficulty that we propose to reject that suggested amendment.
1606. The second issue concerns reporting afterwards. We propose the following wording:
“Where the Department is of the opinion that because of the urgency of the matter it is necessary to act under subsection (1) without consultation —
subsection (2) does not apply; but the Department must as soon as reasonably practical give notice to such bodies as it thinks appropriate of the grounds on which the Department formed that opinion.”
1607. In other words, if the Department acts in a case of urgency, it is required to consult with those bodies and provide the reasons that it formed that opinion.
1608. The Chairperson: Again, it is a case of one amendment being accepted and another being rejected.
1609. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1610. Clause 4, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 6 (Power of Department to give direction to certain bodies)
1611. The Chairperson: Similarly to clause 4, members had concerns about the provision in clause 6(3)(a), which states that the Department is not required to consult: “because of the urgency of the matter, it is necessary to give directions without that consultation”.
1612. Officials agreed to consider similar amendments as in clause 4, which is to insert “extreme” before “urgency” and to report retrospectively when action is taken without consultation.
1613. Mr McMaster: The Department again rejected the suggested amendment because of the same reasons in clause 4 — the difficulties around the phrases “extreme urgency” and “urgency”. However, we accept that there is a need for the Department to explain its reasons for doing so. We propose an amendment to clause 6(3), so that it would read: “Where the Department is of the opinion that because of the urgency of the matter it is necessary to give directions under subsection (1) without consulting the body concerned —
(a) subsection (2) does not apply; but
(b) the Department must as soon as reasonably practicable give notice to that body of the grounds on which the Department formed that opinion.”
1614. We also propose to insert new clause 6(3A):
“Where the Department is of the opinion that (for any reason other than the urgency of the matter) it is not reasonably practical to comply with subsection (2) —
that subsection does not apply; but
the Department must as soon as reasonably practicable give notice to the body concerned of the grounds on which the Department formed that opinion.”
1615. Therefore, the Department is committed to explaining to the bodies concerned why it formed an opinion that it could not consult in advance.
1616. The Chairperson: What is the purpose of proposed new clause 6(3A)?
1617. Mr McMaster: Proposed new clause 6(3A) is slightly different. There are two situations in which the Department does not consider consultation to be necessary. The first situation is because of the urgency of the matter, and the second is because it is not otherwise practicable. In order to achieve clarity, the draftsman entered a second subsection to deal with cases in which it is not reasonably practicable.
1618. The Chairperson: I understand the logic — I think.
1619. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendments, put and agreed to.
1620. Clause 6, subject to the Committee being content with the wording of the Department’s proposed amendments, agreed to.
Clause 8 (Functions of the Regional Board)
1621. The Chairperson: Officials explained that clause 8 outlines the functions of the regional board, which are chiefly those transferred to it from the four existing boards and any other function that the Department directs. The officials explained that clause 8(3) requires the board to draft a commissioning plan. In doing so, it must consult the regional agency and have due regard to its views. Members should note that uncertainty about the various bodies’ relationships — particularly the relationship between the regional board and the regional agency — is a recurring theme in written submissions received by the Committee.
1622. The officials explained earlier that the Minister is considering strengthening that provision by requiring the board and the agency to sign off the commissioning plan jointly. After initial consideration, members were content with that clause as presently drafted, subject to consideration of the joint sign-off proposal.
1623. Mr McMaster: Unfortunately, I am unable to outline the wording. The Department is committed to suggesting an amendment to provide for joint sign-off of the commissioning plan. The wording has not yet been agreed. The Department intends, before Consideration Stage, to clarify that amendment.
1624. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1625. Clause 8, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 9 (Local Commissioning Groups)
1626. The Chairperson: Clause 9 deals with the establishment of the local commissioning groups. Members raised concerns about the wording of clause 9(4)(b)(i), which refers to consultation with the regional agency. The Royal College of Nursing called for that provision to be strengthened, and officials had agreed to consider that suggestion.
1627. Mr McMaster: We have drafted an amendment. The Department believes that it is preferable that the wording of the clause now compels each local commissioning group, in the exercise of its functions, to: “work in collaboration with the regional agency and have due regard to any advice or information provided by it;”.
1628. The draftsman raised concerns about the previously suggested wording. The term “in partnership” has legal connotations and may suggest a formal relationship. The Department does not want to tie two bodies to such a relationship, because it is difficult for two separate organisations to have regard to each other’s priorities.
1629. Mr Easton: I am happy enough with that.
1630. Clause 9(2) states:
“Each Local Commissioning Group shall exercise its functions as regards such area of Northern Ireland as may be prescribed.”
1631. Should we not try to change that to:
“exercise its functions within local government districts.”?
1632. I do not want local commissioning groups to criss-cross all over the place. Do you see where I am coming from?
1633. The Chairperson: The areas will be prescribed in the regulations, and the Committee will have an opportunity to scrutinise those.
1634. Mr Easton: Will we?
1635. The Chairperson: They will be subject to scrutiny.
1636. Mr Bernard Mitchell (Department of Health, Social Services and Public Safety): At a previous meeting, I was asked for, and gave, a commitment that, on completion of local government reform, the boundaries of the local commissioning groups would be reviewed to ensure appropriate coterminosity. I am prepared to restate that commitment.
1637. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1638. Clause 9, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
Clause 12 (The Regional Agency for Public Health and Social Well-being)
1639. The Chairperson: We move now to clause 12 and the corresponding schedule 2. During earlier consideration, members were divided on the merits of a separate regional public health agency. The issue has been discussed in some detail at Committee meetings on 2, 9 and 16 October 2008, and members have a copy of the transcripts.
1640. Some members questioned the merits of setting up a separate agency, arguing that it would create another layer of bureaucracy, be contrary to the aim of creating more efficient structures, and its functions could be dealt with by the regional board. Other members strongly supported a separate agency, arguing that a much stronger public-health message is required. Officials agreed to provide additional information on the likely structures and costs involved. Ivan, I invite you to talk us through clause 12 because it received a good airing, and two opposing opinions were expressed.
1641. Mr Mitchell: In response to the request at a previous meeting, we have tried to provide a clear illustration of the respective position of the agency. We have provided a diagram in which we tried to map the agency’s position and the interrelationships between it, the Department, the board and other bodies. We also outlined in more detail the specified functions of the agency. I am happy to go through the reasons that the Department advocates a separate agency.
1642. The Chairperson: Please do, because it is a contentious subject that, if possible, we would like to resolve.
1643. Mr Mitchell: The case for the agency that underpinned its inclusion in the package of reforms, of which it is considered an important element, relates to public health. The most recent figures available compare public health and well-being in 1999, 2001 and in 2004-06. They show that life expectancy remains worse in the most deprived areas than in Northern Ireland overall: the life expectancy of males is 3·8 years lower and that of females is 2·6 years lower. We consider that the issue of public health and well-being that we are seeking to address is a key challenge faced by the health and social care system in the years ahead.
1644. The feeling was that the arrangements that have been in place in the past, although they have certainly made improvements, have not made the degree of improvement that is considered necessary, and it is felt that a different, more radical, approach is required.
1645. The concept of the agency acquired significant support in the responses to the public consultation, including from: the Royal College of Physicians in London; the Northern Ireland Chief Environmental Health Officers Group; the Royal College of Physicians of Edinburgh; the Institute of Public Health in Ireland; the Health Promotion Agency; the Royal College of Midwives; the Health Protection Agency in London; the British Dental Association; and the Advisory Committee of the Allied Health Professions (Northern Ireland).
1646. The proposed agency would, in partnership with local government and other key stakeholders, provide a focus on issues of public health and well-being, anticipating, and consistent with, proposals for community planning and would seek to have pilot schemes in operation in 2009-10. It is the view of the Department that, under the remit of the proposed regional health and social care board, there remains a risk that public health and well-being will not be prioritised, because of the very significant pressures that will otherwise be faced by that body.
1647. It has been pointed out in previous discussions that the staff of the agency will be co-located and work in a fully integrated way with the staff of the board in supporting the work of the local commissioning groups. The agency will have real influence over the full range of the £4 billion committed annually by the regional health and social care board, and that influence will be spelt out in legislation, including the need for formal approval of the commissioning plan. That point was discussed earlier, in relation to clause 9.
1648. That is a key issue: the agency is not simply concerned with the funding that it receives directly from the Department and which it allocates for health improvement and health protection, and so forth. It also brings real influence — with teeth — to bear on the full £4 billion worth of expenditure that the regional board will commit every year to ensure that public health and well-being achieve the necessary priority.
1649. The staffing of the new organisation is estimated to consist of around 200 to 250 staff, subject to the completion of a staff-mapping exercise. Those staff are currently employed by boards and trusts, the Health Promotion Agency and the research and development office, and are doing work that will continue to be required, irrespective of the organisational structures that are put in place. No matter what structure is established, the great majority of the staff that might be employed in the agency will still have to do that work, whether in a board or in another organisational arrangement. Those are not 200 or 250 additional staff who would not be required if the agency were not established; the great majority of those staff will continue to be required. As we sit here today, they are working in all those bodies, carrying out commissioning work, research and development, and so forth.
1650. We have sought to design the two bodies to avoid duplication as far as possible. It is estimated that, if the agency were to be merged with the board, the savings would primarily be in the boardroom and would be made on positions such as the chairperson, the chief executive, one or two directors, the non-executive directors and any associated costs. The bulk of the staff in question are carrying out functions that will be needed no matter what structure is established. That is a fundamental point.
1651. Mr Martin Bradley (Department of Health, Social Services and Public Safety): I am very conscious that there is a division of opinion about the agency and the board, and how those two organisations can be brought together to work in tandem. I do not want to rehearse the arguments that the Committee has heard from the Chief Medical Officer, but, speaking as a nurse and as the Chief Nursing Officer, there are still unacceptable variations in health outcomes in Northern Ireland. That is in spite of having 60 years of the Health Service. We are still not getting something right. We have a real opportunity to do something different that will put us ahead of the rest of the United Kingdom, and having an agency that is dedicated to solving some of the fairly wicked problems that we are faced with would do that.
1652. I meet health visitors, school nurses and hospital and community midwives regularly. They are aware of the conditions that people in Northern Ireland have to live with. We must try to do something about that and articulate a much better vision as to how we get ahead of some of the lifestyle choices that we must make if we are to have a better outcome for the people of Northern Ireland and the next generation — particularly mothers and children.
1653. If we always do what we always did, we will always get what we always got. We have a real opportunity to get ahead of the game, do something different and, in particular, build a cohort of staff who can focus in a new way, without the encumbrance of having to do all the firefighting that we do daily in the Health Service. We must try to get ahead and have some dedicated time to have a dedicated resource and the expertise, the thought and the intelligence to put us ahead on some of the major issues that we continue to face.
1654. Without rehearsing all the arguments that the Chief Medical Officer outlined, as Chief Nursing Officer, I see a real opportunity for us to do something different.
1655. The Chairperson: Although I am Chairperson, I have a concern about a further tier of bureaucracy; if the regional agency is going to be part and parcel of the board in any case, why make it a separate stand-alone agency? I have concerns about equality. What patterns are we using to target social need and areas of high need that will ensure that both communities receive a fair coverage of moneys and input into healthcare promotion and all that that entails? On what are you basing your areas? What mapping is being used? I make no apology for being concerned that some communities — particularly unionist communities — have not seen the same input of moneys down through the years. I am not being politically obstinate or trying to raise a red flag to a bull. It is a fact that some of the most deprived areas are unionist, and areas such as the Shankill Road and Tullycarnet come to mind.
1656. I am afraid that it will be the same old, same old, where there is a wide proofing — if that is needed or if that is the proper word — but unionist communities have suffered quite considerably in not being able to project their needs as well as the Roman Catholic community; I say that without any bias. That is a major worry, and it is the reason that I am concerned about what you are establishing as areas of need and where that goes back to.
1657. Mr Bradley: Your points are well made. We can have a much better public debate about how some of the problems will be tackled if we can establish a more coherent agency to deal with those issues. The main factors that drive the issue are education and unemployment. Yesterday, the Institute for Public Health in Ireland published a report showing the clear link between educational outcomes and life chances.
1658. It is true that, in our communities, people achieve different educational outcomes, and people have a different attitude towards education, which does affect how they go through their lives and the consequences that that can have for local communities. Part of this discussion has to be about empowering people and local communities, but it is also about consistent, persistent, concentrated public-health action. It is about mobilising a significant resource. In the world in which I live — of health visiting, district nursing and, in particular, community midwifery — the focus must be on the real areas of need.
1659. I am currently conducting a review of health visiting and school nursing, one of the outcomes of which will be a more focused attempt to target those families that are in the most need. They are spread across both communities. You are right; there are issues in Northern Ireland on how communities access services and how services are best used. A public health agency would be empowered to begin to raise the profile of those wicked issues and begin that debate — not only with the public but with Departments. Part of the conversation a while ago was about the need for more co-ordinated working — for instance, between the Department of Education and the Department of Health, Social Services and Public Safety.
1660. Mr Mitchell: The information that I quoted earlier came from the Department’s report, ‘Health and Social Care Inequalities Monitoring System: Changes in the Life Expectancy Gap 1999/01–2004/06’. It is worth highlighting one of the issues underpinning the reforms — that is, democratisation. The proposal is that the agency will have two local government representatives on its board. The agency will also be charged with leadership in progressing local government partnerships across Northern Ireland and with the intention of our trying to put in place, in theory, pilot schemes from April 2009, which would anticipate community planning and wider community engagement.
1661. The issue of democratisation can also be read across into the membership of local commissioning groups, and so forth, which will include four local government representatives. There is a vein of democratisation running through the reform package, which, I hope, would give appropriate political input.
1662. Mr Easton: I had the chance to speak to representatives from different health agencies and bodies who attended the DUP party conference last weekend. We have been led to believe that everybody is in favour of the new public health agency. I am not against it, but I am against an extra layer of bureaucracy and the associated costs. I think that that can be done in the regional board, and I cannot see the point of the agency being a separate body.
1663. Many representatives of the health bodies with whom I have spoken do not see why the agency’s functions cannot be kept within the regional board. The same functions would be carried out; the board could be toughened up and could do the new things that we require of it. I do not care what anyone says — it will cost money to set up the agency. It will create an extra layer of bureaucracy, which we are meant to be doing away with as we enhance, and create a better, Health Service. Given the extra bureaucracy and cost, I would be happier if the agency’s functions were kept within the regional board. I have heard no arguments to convince me otherwise. At the risk of being on my own on this issue, I propose that the public health agency is incorporated into the regional health and social care board under clause 7.
1664. Mr McCallister: I oppose Alex’s idea. The public health role is too important not to have an agency focusing on it. Last year’s debate on the Budget highlighted to me — as did Professor Appleby’s evidence to the Committee, and also what Martin has said — that, if we fail to engage the public with their health, we are sitting on a funding time bomb for health services in years to come.
1665. We must raise our game. Health promotion is one positive way to do that. I support the creation of a regional agency that focuses on that agenda. Previously, the Minister has talked about the need to work with local government in order to deliver some of that agenda on the ground. Members all know of areas of deprivation and inequality where public health must be promoted, as well as among the general population.
1666. Ms S Ramsey: My party does not support Alex’s proposal. At previous meetings, the point has been made that the issue is health promotion and the Investing for Health strategy. The body that is involved with that must be proactive. All the Committee’s discussions during the past few weeks have been about the need to tackle illness in all communities, because all areas suffer from poor health and illness. We must be proactive on public health.
1667. I am interested in the connection that was made between poor health and poor educational attainment. It is important, therefore, that a collective body exists that is involved in proactive health promotion and will have the authority — for want of a better word — to hold other Departments to account, whether that be DSD, DCAL, DE or DEL, and so on. My party does not support Alex’s proposal.
1668. Mrs Hanna: The SDLP will not support the proposal either. I will certainly raise my concerns. I want the focus to be on public health. For years, I have been a champion of public health. I raised concerns about how the regional agency would have teeth and would have a meaningful relationship with communities. We have been given some answers. However, the proof of the pudding will be in the eating. We understand that.
1669. Inevitably, there will be costs. However, if lives are saved through prevention and early intervention, money will be saved down the line. I firmly believe that if the agency can work, money will be saved. We must watch it and ensure that it works.
1670. Dr Deeny: I want to respond as someone who is interested in public health and who has worked in the Health Service for many years. I have taken on board Alex’s point. We all accept that, for many years, the Health Service has been over-administrated and over-bureaucratised. That has now been addressed.
1671. My worry is that, if the agency is incorporated into the board, it will be low on the pecking order of importance and priority — as, indeed, the Chief Medical Officer has mentioned. Public health, health promotion and disease prevention are major elements of the future of healthcare. For far too long, we have waited until people become sick before we treat them, which costs a lot of money. As I have said before, my worry, as a doctor, is that, if the agency is incorporated into the board, public health, health promotion and disease prevention will not have a strong enough voice.
1672. I understand that the agency needs to work with local commissioning groups. I like the terminology: “democratisation”. That is important; every area of health must be represented and have input, not only from political representatives but from GPs in local areas. It is important, too, for the future of commissioning for the health needs of local areas’ populations.
1673. I asked you about the number of administrative staff in the Health Service, Bernard. You mentioned that 700 people are employed by the Department, 400 people by the regional board, and 250 to 350 — let us say 300 — by the agency. That is a total of 1,400. I know that there is a bigger picture and that staff are employed outside Belfast. However, the public will see that as 1,400 people, who are mainly based in Belfast, administering for a population of 1·7 million people. That seems like an awful lot of staff. Therefore, I agree with Alex on that point.
1674. I do not suggest that people should lose their jobs, as has occurred in trusts and boards. The Minister has explained that some of those staff will leave the Health Service through “natural wastage”, without any enforced or compulsory redundancies. Has the Department reviewed its staff numbers — which exceed 700 — with a view to making efficiency savings? To those 700 staff in the Department must be added 400 and a further 300; that comes to 1,400 people. The point is often made to me that one could slim down the bureaucracy and still have sufficient staff to man the agency.
1675. Mr Mitchell: The answer in respect of the Department is yes. The Department’s staff total will be reduced from over 1,000. My bitter experience is that staff numbers of any organisation, considered in isolation, always sound large. One must consider what it is the officials do before one can decide whether the number of officials is justified.
1676. Those staff were never envisaged as being entirely based in Belfast. The Minister has made it clear to workshops that I have attended that we envisaged maintaining a significant local presence across the Province. The majority of the staff about whom we are talking will probably be based in local environments. They cannot support local commissioning groups and local family practitioner services from a base in Belfast. It has never been our intention to base all those folk in Belfast: we have always been clear that we will maintain a strong local presence.
1677. One must not lose sight of the overarching savings to which the Department is committed: £53 million and a reduction of 1,700 posts, primarily in administrative and managerial grades. That remains the case irrespective of the structures. Those targets must still be met.
1678. The Chairperson: I will put the question; however, even if this proposal falls, no party is precluded from tabling amendments at Consideration Stage.
1679. Question proposed:
1680. That the regional public health agency be incorporated into the proposed regional board under clause 7. — [Mr Easton.]
1681. Question put.
1682. The Committee divided: Ayes 2; Noes 6.
AYES
Mr Easton, Mrs I Robinson
NOES
Dr Deeny, Mr Gallagher, Mrs Hanna, Mr McCallister, Mrs O’Neill, Ms S Ramsey
1683. Question accordingly negatived.
1684. Question put, That the Committee is content with the clause.
1685. The Committee divided: Ayes 6; Noes 2.
AYES
Dr Deeny, Mr Gallagher, Mrs Hanna, Mr McCallister, Mrs O’Neill, Ms S Ramsey
NOES
Mr Easton, Mrs I Robinson
1686. Question accordingly agreed to.
1687. Clause 12 agreed to.
Clause 13 (Functions of RAPHSW)
1688. The Chairperson: When clause 13 was previously considered, members raised three concerns about the drafting of the clause, which were highlighted in written submissions.
1689. Disability Action called for clause 13(2)(b) to be expanded to better outline the health-promotion function, and the British Red Cross asked for the same paragraph to be strengthened by including a reference to risk reduction. The Association of the British Pharmaceutical Industry called for the regional agency to be required to consult the Committee for Health, Social Services and Public Safety before making persons, materials and facilities available to other bodies. I invite Ivan to talk us through this.
1690. Mr McMaster: We accept the suggestion to expand the wording with regard to the health-promotion function of the regional agency. We propose to table an amendment so that clause 13(2)(b) would read as follows: “The health promotion function is including, in particular, enabling people to increase control over, and to improve, their health and social well-being.”
1691. That, incidentally, is the recognised World Health Organization definition of health promotion. Our intention is to make it clear what health promotion actually means. It also has the benefit of retaining the phrase “health promotion”, which is a recognisable phrase.
1692. We do not propose to include the phrase “risk reduction”. It was felt that risk reduction was already included. If one is increasing control over, and improving, one’s health and social well-being, risk reduction is considered to be a part of that, without having to say so specifically.
1693. A third issue was raised: to include, in clause 13(4)(e), the words:
“including the Assembly Health, Social Services and Public Safety Committee”
1694. after the words “any other body”. We decided not to accept that change. This provision is intended to allow the agency, in carrying out its functions, to be able to work with other bodies on matters such as promotions and other day-to-day activities. To constrict the agency in a way that would prevent it from providing those bodies with materials, personnel or facilities would be a significant inhibitor of the agency’s day-to-day performance of its duties and could prove to be extremely bureaucratic if it had to come back and consult each time before it did that.
1695. The Chairperson: I should point out to members that the Committee can table an amendment if we do not agree with your decision not to accept that change. Again, we got 50% of what we wanted.
1696. Question, That the Committee is content with the clause, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1697. Clause 13, subject to the Committee being content with the wording of the Department’s proposed amendment, agreed to.
Clause 15 (Functions of RSSO)
1698. The Chairperson: During an earlier meeting of the Committee, members raised an issue that had been highlighted by the Northern Health and Social Services Board. It was suggested that in clause 15(3)(a), in relation to securing the provision of support services, the word “equitable” should be included as well as the words “economic, efficient and effective”.
1699. Mr McMaster: We do not propose to insert the word “equitable”. The regional business services organisation (RBSO), as we are now proposing to call it, will be bound, as are all newly created bodies, by the legislative requirements of section 75 of the Northern Ireland Act 1998, which requires such bodies to be equitable in all their dealings. However, this clause puts in place arrangements to: “provide, or secure the provision of, support services to other health and social care bodies”
1700. on demand. Therefore, we felt that it would not only be unfair but difficult for a new organisation to demonstrate that its services were being provided in an equitable way. The services that the RBSO will provide are support services. To ask it to provide those services in an equitable way places a duty on it that we believe it cannot meet.
1701. The Chairperson: Are you saying that those services are already equality proofed?
1702. Mr McMaster: All the RBSO’s dealings are equality proofed. It will be called on to deliver services. The bodies that ask the RBSO to deliver services must ensure that their dealings are equality proofed. You are asking an organisation that is acting as an agent to second-guess whether the client body is equitable in its dealings.
1703. Mr Gallagher: Can it be amended later?
1704. The Chairperson: The Committee can propose amendments now or parties can add amendments —
1705. Mr Gallagher: Do you mean in the Chamber?
1706. The Chairperson: Yes, during the Consideration Stage debate. The enunciator informs Members when amendments are being accepted for debates.
1707. Question, That the Committee is content with the clause, put and agreed to.
1708. Clause 15 agreed to.
Clause 17 (Functions of the Patient and Client Council)
1709. The Chairperson: In the previous consideration sessions, members raised two matters relating to clause 17. First, in clause 17(2)(a), Disability Action proposes that the council should be required to consult the public “in an accessible way”. Secondly, Disability Action questioned whether clause 17(4) refers to reasonable adjustments, as defined in the Disability Discrimination Act 2005.
1710. Mr McMaster: We reject the suggestion that the patient and client council should consult in an accessible way. Although there were considerable discussions with the draftsman about the wording of that subsection, the patient and client council will be bound by the requirements of the Disability Discrimination Act 2005. Therefore, the draftsman concluded that there is no reason to repeat that Act’s provisions in this Bill. The Act already stipulates that consultation must be carried out in an accessible way. In carrying out the its functions, the council must promote positive attitudes to, and encourage participation by, disabled people. Indeed, it is a drafting principle that existing primary legislation should not be duplicated in new legislation. Therefore, given that the patient and client council will be bound by the 2005 Act, those provisions will not be repeated in this legislation.
1711. The second matter is covered by the same response. Given that the patient and client council is bound by the provisions of the 2005 Act, the council will be required to make reasonable adjustments to meet individuals’ requirements.
1712. Ms S Ramsey: I appreciate that; however, whether we are discussing section 75 or the Disability Discrimination Act 2005, when bodies such as Disability Action — which deals day and daily with clients who are directly and indirectly affected by legislation — submits such proposals, is it not worthwhile attempting to reach an agreement that suits everybody? I accept what you said about clause 17(4), but what is the difficulty with inserting “in an accessible way” into clause 17(2)(a)? Although the draftsman says that that is already covered in the 2005 Act, we should not be prevented from including that phrase in the new Bill. When a body such as Disability Action makes a suggestion, I cannot understand why we must get into a fight about it. Disability Action is not asking for everything to be changed; it is merely making a positive suggestion for the Bill.
1713. Mr McMaster: I understand your point. Although we recently had long discussions about that subsection with the draftsman, he is bound by what he calls “drafting principles”, which prohibit repeating provisions that are elsewhere.
1714. Ms S Ramsey: You may say that you do not accept that; however, we are in a new dispensation, and my concern is that, although we have the Disability Discrimination Act 2005, Disability Action found it necessary to suggest those four words — “in an accessible way” — so it must conclude that the 2005 Act does not go far enough. Whatever the draftsman said, is there any point in getting into a fight about those four words?
1715. The Chairperson: Everyone who has made known their opinion and who wishes additional words to be inserted would, from their perspective, attempt to safeguard that opinion.
1716. Mr Mitchell: Our presumption concerning all the Committee’s proposals was to say yes as much as we could. That is the position from which we began, and we attempted to accept the Committee’s proposals when it was possible for us to do so. I asked the draftsman to go through that specific issue because Claire had raised a couple of matters, and I was conscious that the Department was saying no to two or three issues that were raised by members. Therefore, I pushed it a wee bit.
1717. As Ivan explained about precedents, if the response to individual requirements were to include excerpts from other pieces of legislation, the process would become endless. Every piece of legislation would then replicate every insert that any particular group wished to have included in order to highlight its concerns. The draftsman said that there was no end to that process and that once words are used they must be defined. Therefore, if the phrase “in an accessible way” is used, there is guidance running to several pages on what that means. In the same way, “reasonable adjustment” is defined in several pages of guidance. The difficulties snowball.
1718. I assure the Committee that the Department’s starting point, and the reason that I asked to meet the draftsman, is summed up simply — we should be able to do this. However, his counter-argument was reasonably substantive. I started from the same position as the Committee. That was my wish, and I wanted to include the proposal.
1719. Mr Gallagher: I have some sympathy with Sue, and I have the highest respect for the legal profession. However, the Committee must listen carefully when legal people state that nothing more can be done. Nevertheless, there is no such thing as perfect legislation. If the Committee accepts this precedent, it may not be possible to tackle a serious problem that might arise in the future. Other than being here for a year, however, I cannot see how the Committee can proceed. It must accept the advice.
1720. Is it possible for the Committee to go back to Disability Action in order to establish why it made that suggestion? The Committee could then pick up on the issue again with the Department later.
1721. The Chairperson: The problem, Tommy, is that the Committee is trying to agree all the clauses today. An individual member may want to make contact with Disability Action and propose an amendment as a party at Consideration Stage. That may be an appropriate course of action. The Committee is tied for time, but that does not prevent members submitting amendments on behalf of their parties.
1722. Question, That the Committee is content with the clause, put and agreed to.
1723. Clause 17 agreed to.
Clause 19 (Public involvement: consultation schemes)
1724. The Chairperson: At an earlier consideration, members were content with the clause as presently drafted, apart from a question in relation to clause 19(1)(a) about the provision of information in accessible formats.
1725. Mr McMaster: The provision of information in accessible formats involves the same principle as consulting in an accessible manner.
1726. Question, That the Committee is content with the clause, put and agreed to.
1727. Clause 19 agreed to.
Clause 22 (Public-private partnerships)
1728. The Chairperson: During previous consideration, members expressed concerns about the principle of public-private partnerships (PPP) and referred the clause for further consideration. Members also proposed that the clause should include a reference to ensuring the long-term financial viability and value of any PPP schemes.
1729. Mr McMaster: The clause was considered, and the Department decided not to include such a reference. The thinking behind that was that to provide in legislation a requirement to ensure that the long-term financial viability would be an open-ended requirement and that, although for the foreseeable future — which could be 10, 15, 20 or 25 years — a project could be financially viable, it might subsequently prove not to be. It might be financially viable only as far as one can see. If long-term financial viability were to be included in the legislation, someone could come back after 30 or 40 years and say that a project was not financially viable and question why it was done.
1730. As I said before, the provision is merely enabling the new organisations to use public-private partnerships. Any organisation in Northern Ireland, when procuring anything, is bound by Department of Finance and Personnel guidance, which is taken from Treasury guidance. I will quote to the Committee from a “Dear accounting officer” letter, which is issued by the Department of Finance and Personnel to all organisations:
“The central concern in taking procurement decisions is as always the achievement of VFM. PFI or any other PPP should only be pursued where it delivers VFM, defined as the optimum combination of whole of life cost and quality (or fitness for purpose) of the good or services to meet the user’s requirement; and does not always mean choosing the lowest cost option. In order to ensure that consistently good VFM procurement decisions are made, it is important that VFM assessments should take place as early as possible”.
1731. That applies to any procurement route that is followed. It continues:
“and that Departments ensure there is the flexibility to pursue alternative procurement routes if at any stage PFI/PPP does not offer the best VFM.”
1732. Guidance from the Treasury and the Department of Finance and Personnel, which all Departments must follow, makes it clear that value for money is the starting point, and one must consider it before one can consider not only public-private partnership agreements but any procurement route that they chose to follow.
1733. Therefore, we do not propose to include the requirement for value for money, because it is firmly set out in guidance. Value for money is the beginning and the end of all procurement that is directed by the Department of Finance and Personnel.
1734. Mrs Hanna: Many people are, at best, sceptical about PPPs. I had to make an attempt to get that provision in somewhere. I accept your point, but you used the word “consider”. Your letter of 22 October 2008 states: “where a public-private partnership is to be entered into, the body concerned must ensure that option demonstrates best value for money and long-term financial viability.”
1735. PPPs should demonstrate value for money when they are being considered, before a decision is made. The following wording would be preferable:
“When a public-private partnership is to be considered, it must demonstrate value for money.”
1736. The paragraph, as it stands, can be read as though the decision has already been made on the public-private partnership, and it is subsequently demonstrating value for money.
1737. Mr McMaster: After an earlier Committee meeting, we considered that proposal. Having considered it with the draftsman, we decided not to include it.
1738. Mrs Hanna: You will not include any of that?
1739. Mr McMaster: We will not include in the legislation the requirement that one must guarantee that an agreement represents value for money before one enters into it.
1740. Mrs Hanna: I am not saying “guarantee”. The legislation should state that, while considering a PPP, one should demonstrate that it provides best value for money. There is a lot of concern that it does not demonstrate best value for money.
1741. Mr McMaster: The process is such that before anyone can procure anything — a building, goods or whatever — the initial guidance and policy from the Department of Finance and Personnel is that one must consider value for money: that must be the first consideration.
1742. Mrs Hanna: That it taken as read.
1743. Mr McMaster: Yes, and it is important that it is taken as read. This provision will ensure that, if value for money turns out to be down the public-private partnership route, the bodies that we are creating can enter into those partnerships. The first consideration is value for money, and, having considered value for money, any of those bodies can go down several different routes. Once they have said that public-private partnership is the route, the provision simply enables that to happen. Without the provision, none of the bodies that we are creating could enter into a public-private partnership. The provision is not saying that it has to do so; it is saying that it will follow DFP guidance, consider value for money and come up with the preferred route. That preferred route may not be a public-private partnership, and, if so, this provision does not matter. However, if the best value-for-money route were to be a public-private partnership, this provision would allow that to happen.
1744. Mr Gallagher: I note that you are taking best Treasury guidance, and all the rest, which frightens me. However, I understand why you are doing that. If the Treasury guidance is fine and good, how did the car park at the Royal Victoria Hospital end up to be such poor value for money — in fact, to be a real rip-off? That is why we are worried about getting the matter right.
1745. Mr Mitchell: The question is whether one tries to preface what is in the legislation with some kind of explicit reference to the obligations that are laid on public bodies to do what Ivan quoted from the “Dear accounting officer” letter, and we put that explicitly to the draftsman. In one sense, there is no disagreement between us at all in the requirements that are laid down and what Ivan quoted, which are fully consistent with your concerns. The question is whether they can be made more explicit in the legislation.
1746. Mr McMaster: The difficulty with saying that a public-private partnership must be value for money before it is entered into is the fact that it could come back to haunt someone further down the line. Treasury guidance states that one must look as far ahead as possible. However, once the provision that it must guarantee value for money is in legislation, it is there for ever, beyond the period of normal Treasury guidance, which, I imagine, has a limited lifespan — although I am not a Treasury expert. Value for money stretches to a certain point, and one cannot see beyond that point. However, once a provision is inserted into legislation, it remains there for ever or until the legislation is amended to remove that provision.
1747. The steps that are used in the process are important. When one wants to do something that is considered value for money, one must select the options. This provision simply permits one option: it does not advocate that option. The first step is to agree on value for money. We could talk all day about whether the current guidance on assessment of value for money is right or proper, but that is a separate issue altogether. However, there is guidance, and the first step must be to ask what the best value-for-money option is. After that, one can select an option. If an organisation has followed all the necessary steps and a public-private partnership arrangement turns out the best value-for-money option, the clause will simply allow that organisation to enter into an agreement. Without that provision, none of the bodies could enter into an agreement because there would be no legislation permitting them to do so. The clause does not state that they have to enter into a PPP or that they should do it, and neither does it say that they should override all other steps that are taken to try to secure value for money.
1748. Dr Deeny: You talked about PPPs, PFIs and value for money. The important word here is “demonstrate”. There is nothing private about a PPP or a PFI; they involve public money that has to be repaid over a long period. Tommy mentioned the Royal Victoria Hospital car park, and we know about the case of Balmoral High School. Across the water, several health projects were entered into as PPPs, but the public sector had to pay to get out of the contract. Therefore, we are talking about public money not private money. Private groups may provide the initial finance, but they are then paid back, out of the public purse, over 25 years or whatever. Therefore, if a PPP or PFI turns out to be the most cost-effective and best value-for-money option, it is vital that that it is clearly demonstrated to the public why that is the case. I have studied examples of PFIs and PPPs across the water, and I know that the repayments come out of the health budget — and there may be an impact on other services. Therefore, it is very important that whatever option is taken — and let us not forget, clause 22 is not about other options; it is about PPPs — it is clearly demonstrated to the public that value for money will be achieved. There have been cases in the past in which value for money had clearly not been achieved and in which PPPs have had a very negative impact.
1749. Mr Mitchell: The issue takes us a step away from the legislation. It relates more to the Committee’s concerns about the current guidance that informs the use of PPPs or PFIs. It seems that we are discussing whether the general guidance that is issued throughout the public sector is applicable and whether your concerns can be addressed.
1750. Mr McMaster: I could not agree more that value for money has to be demonstrated, and that is why the Department of Finance and Personnel requires every organisation to carry out a value-for-money assessment on any project into which they enter. That assessment should show what is producing the best value for money and why, and the reasons that other options are being rejected. As I said, that is part of the consideration process, and, by all means, that process should be open, available and clear.
1751. We could argue at length about how those decisions are reached. Dr Deeny is right; those value-for-money assessments must be carried out. However, this provision deals with the point beyond that; it simply allows an organisation that has carried out an assessment that demonstrates that a public-private partnership is the best value for money to enter into that contract and deliver on it. The provision enables delivery; it has nothing at all to do with the assessment that leads up to the decision, although it is absolutely essential that those assessments are carried out. I hope that the Department of Finance and Personnel will exercise control and ensure that value-for-money assessments are carried out correctly. I cannot speak about cases whereby assessments have been wrong. Clause 22 simply enables an organisation to enter into a contract once everyone is satisfied that the best value for money would be delivered through a PPP. It has nothing to do with the assessment that goes before it; that is done long before getting to that stage, if it represents best value for money and if DFP agrees to do that. That has all gone before this stage is reached. Clause 22(1) refers to that as:
“A body to which this section applies may form, or participate in”.
1752. Nothing is mentioned about the assessment prior to that; it is about forming a partnership to deliver on that.
1753. Question, That the Committee is content with the clause, put and agreed to.
1754. Clause 22 agreed to.
Clause 29 (Orders, regulations, guidance and directions)
1755. The Chairperson: At an earlier consideration, members questioned what consideration had been given to whether regulations under clause 29(2) should be subject to negative resolution or affirmative resolution. Subordinate legislation that is made under different procedures is subject to different levels of scrutiny and approval in the Assembly. The Examiner of Statutory Rules has provided advice to the Committee on that issue, and his paper is tabled today. That paper has been shared with the officials.
1756. Mr McMaster: Further consideration was given to clause 29. Clause 29(1) sets out areas in which it is considered that affirmative resolution should be used. That will allow Orders to propose altering the functions of the new regional agency, the new regional business services organisation or any Order that allows legislation to enable the Bill to come into operation. Those are the areas that are likely to merit the most discussion and that should be formally approved by the Assembly.
1757. Any other regulations and Orders that are proposed will relate more to the day-to-day organisation of the various new bodies, and, therefore, it would be considered to be more appropriate to the negative resolution procedure. As with all subordinate legislation, the Department is required to submit a formal SL1 proposal, by which we must set out the purpose of any set of regulations or any Order, and the reason that those are being made. Those will be scrutinised by the Committee for Health, Social Services and Public Safety. The Department considers that clause 29 should remain as drafted.
1758. Question, That the Committee is content with the clause, put and agreed to.
1759. Clause 29 agreed to.
Schedule 1 (The Regional Health and Social Care Board)
1760. The Chairperson: At an earlier consideration, members were content with schedule 1 as drafted, but the schedule was not formally agreed at the last meeting.
1761. Question, That the Committee is content with the schedule, put and agreed to.
1762. Schedule 1 agreed to.
Schedule 2 (The Regional Agency for Public Health and Social Well-being)
1763. The Chairperson: Schedule 2 is linked to clause 12, which we agreed earlier. At the earlier consideration, the officials accepted that there was an error in paragraph 7(3) of schedule 2, in that the reference to the regional board should read “RAPHSW”.
1764. Mr McMaster: The Department proposes to table an amendment that will insert a new schedule 2 to take on board the change that we suggested. It would amend all references to “RAPHSW” to “regional agency”. The insertion of a new schedule will cut down the number of amendments that would have been required at Consideration Stage. There are already around 175 references, and we trying to cut that down as much as possible. Inserting a new schedule and changing the references will reduce the number of amendments that must be moved. We propose to insert a new schedule 2 that amends “RAPHSW” to read “regional agency” in every case.
1765. We noted another error. I point that out to ensure the Committee is kept up to date on everything. The provisions of each of the schedules allow for people who are appointed to the boards of those organisations to resign or to be removed by the Department. The provisions, as previously stated, apply only to the chairperson and other non-executive directors. However, as Bernard pointed out, the board of the regional agency will also include some local councillors, who are appointed by the Department. Therefore, the provision must be extended to those people as well.
1766. Question, That the Committee is content with the schedule, subject to the Committee being satisfied with the wording of the Department’s proposed amendments, put and agreed to.
1767. Schedule 2, subject to the Committee being satisfied with the wording of the Department’s proposed amendments, agreed to.
Schedule 5 (Transfer of assets, etc)
1768. The Chairperson: At the earlier consideration, the Department advised that it proposed to make an amendment to paragraph 2(6) of schedule 5 to insert a reference to the transferor organisations.
1769. Mr McMaster: Paragraph 2 of schedule 5 deals with the transfer of employed staff. When that schedule was drafted initially, it stated that certain people should not be involved in the consideration of grievances.
1770. As currently drafted, the paragraph states that a member, or member of staff, of a transferee —the body to which the assets are being transferred — or a member of staff of the Department should not be involved in those grievances. That is correct; no one who has a vested interest should be involved in the consideration of grievances. Unfortunately, the term “transferor” was left out. The transferor is the body from which the assets or liabilities are being transferred. The term was left out because it was thought that all the bodies from which assets are being transferred would be dead in the water by the time the legislation was enacted. However, the provisions allow certain assets to be transferred after 1 April 2009, if needs be. For example, functions for shared services may be transferred at a later date. Therefore, if a body from which the staff are being transferred is still in existence, its staff should not be involved in the consideration of grievances. That brings the Bill into line with similar provisions in the Libraries Act (Northern Ireland) 2008. The Department of Finance and Personnel brought that to our attention.
1771. Question, That the Committee is content with the schedule, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1772. Schedule 5, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, agreed to.
Schedule 6 (Minor and consequential amendments)
1773. The Chairperson: At the earlier consideration, the Department advised that it proposed to make a technical amendment to paragraph 18(1)(a) of schedule 6.
1774. Mr McMaster: The amendment to paragraph 18(1)(a) of schedule 6 is consequential. It deals with the provision of information as to births and deaths, which we got wrong. Paragraph 18(1)(a) of schedule 6 states: “for ‘or the Agency’ substitute ‘, the Regional Board or RAPHSW’”.
1775. That is wrong, because those functions are transferring to the regional business services organisation. Therefore, we propose that the wording be amended to reflect that.
1776. Question, That the Committee is content with the schedule, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, put and agreed to.
1777. Schedule 6, subject to the Committee being satisfied with the wording of the Department’s proposed amendment, agreed to.
1778. The Chairperson: That concludes the formal clause-by-clause consideration of the Bill. A draft report to the Assembly on the Committee Stage of the Bill will now be prepared and considered by the Committee at the next meeting.
1779. I thank Martin, Bernard, Ivan and Craig for their attendance today. No doubt, we will see you again.
1780. Mr Mitchell: There have been five or six sessions, and members have had to take in a lot of detail. On behalf of my colleagues, I wish to express my gratitude for the way in which members have conducted themselves and for the care and attention that they have shown throughout. It is very much appreciated.
Appendix 3
Written Submissions
Table of Contents
Health and Social Services Councils
Central Services Agency
Ards Borough Council
Eastern Health and Social Services Board
Belfast City Council
Southern Area Children and Young People’s Committee
Mental Health Commission
Western Health and Social Services Board
Regulation and Quality Improvement Authority
Royal College of Nursing
Children in Northern Ireland
Northern Health and Social Services Board
Northern Ireland Association for Mental Health
Northern Ireland Commissioner for Children and Young People
Health Promotion Agency for Northern Ireland
Age Concern (NI)
British Medical Association NI
The Northern Ireland Confederation for Health and Social Services
Optometry NI
NCH NI
South Eastern Health and Social care Trust
The Association of the British Pharmaceutical Industry
Disability Action
Pharmaceutical Society of Northern Ireland
Royal College of Obstetricians and Gynaecologists
Ulster Cancer Foundation
RNIB Northern Ireland
British Red Cross
The Community Development and Health Network
Lisburn City Council
Health and Social Services
Councils for Northern Ireland
The Health & Social Services Councils (HSSCs) were set up by Government in 1991 to represent the view and opinions of the public in relation to health and social care. The HSSCs are independent from those who plan, manage and provide health and social care services.
The comments below seek to represent a broad public interest perspective on the Health & Social Care (Reform) Bill.
Department’s Role in Promoting and Providing Health and Social Care.
Clause 2
The HSSCs welcome the clear, strategic role set out for the Department.
Clause 3
The HSSCs also welcome the continued promotion of integrated health and social care services.
Clause 5
We suggest that there is a need for the early production of the framework document outlining the roles and functions of each health and social care body. Each health and social care body (and other bodies and persons) must be consulted in the preparation of this framework document.
The Regional Health and Social Care Board
Clause 7
The HSSCs welcome the establishment of the Regional Board.
Clause 8 (1)
We support the functions of the Regional Board as set out in the draft legislation. Our preference would be to see an additional primary function confirming the duty to engage with its population in regard to the health and social care needs as one of its core functions.
Clause 8 (2)
There is no reference in the Board’s functions about balance of regional, strategic commissioning and locally responsive commissioning which will be delegated to the Local Commissioning Groups. The HSSCs believe that the achievement of such as balance will be pivotal to the success of the new commissioning arrangements.
Clause 9
Local Commissioning Groups are welcomed by the HSSCs as a way of responding to local issues and aspirations but clearly these structures do not have autonomy and are fully accountable to the Board. There needs to be a fit between the regional commissioning needs of people with a rare condition and their need for locally responsive services.
Clause 9 (5)
The HSSCs would welcome a specific requirement to meaningfully engage with local communities and communities of interest as part of their commissioning remit.
Power of the Regional Board to give Guidance to Trusts
Clause 10
We believe that the powers set out in the legislation are required in order to ensure proper accountability of the Trusts. It is important that there is a clear line of accountability and performance management from the Trust to the Regional Board and then on to the Department.
The Regional Agency for Public Health and Social Wellbeing
Clause 13
The HSSCs feel that RAPHSW should be accountable to the Regional Health and Social Care Board. If it is accountable to the Department, this potentially fragments the role of the Regional Board and causes confusion.
Clause 13 (6)
Subordinate legislation will need to clearly set out the relationship between the RAPHSW and other bodies, in particular the RHSCB.
The Regional Support Services Organisation
Clause 14
The HSSCs support the establishment of the Regional Support Services Organisation. We believe that this will assist in reducing duplication and in delivering economies of scale.
Clause 15 (2)
The efficient delivery of services from a regional body to local service providers and commissioners should be supported by the creation of service standards that will allow the RSSO to be held accountable to the Department for the way in which it meets its core functions.
The Patient Client Council
Clause 16
The HSSCs support the establishment of the Patient Client Council.
Clause 16 (2)
The HSSCs support the PCC model of a single organisation strengthened by a local council of members associated with each of the five offices. The HSC Reform Bill refers to a body corporate known as the Patient and Client Council. It makes no reference to local offices or local councils of members.
Clause 17 (1)
Within the functions of the Patient Client Council is the responsibility to represent the interests of the public. The ‘public’ includes individuals, a group or community of people and a section of the public. It will need to be clarified the extent to which the PCC can represent individuals and appropriate resources made available.
Clause 17 (1) (e)
The core function of advocating for patients, clients, carers, communites and interest groups should be specified.
Clause 18 (3)
The monitoring of service provision by the PCC is not specifically mentioned. However the Bill refers to Regulations which may make provision authorising members of the PCC to enter Health and Social Care premises to exercise its functions.
Subordinate legislation will be required to address many of the proposals and detail submitted by HSSCs.
Public Involvement and Consultation
Clause 19 (1)
The HSSCs welcome this provision. We believe that this can only be effectively discharged by a requirement on HSC bodies to proactively engage with their population and communities.
Duty on HSC trusts in Relation to Improvement of Health and Social Wellbeing
Clause 21
The HSSCs welcome this additional responsibility for the HSC Trusts.
Furthermore we would like to see this strengthened by reference to the Trust’s duty to engage with local communities and service users in carrying out this reference.
Public - Private Partnerships
Clause 22
The HSC notes this facility. We believe that this section should include a reference to ensuring the long term financial viability and value of any such public-private partnership before entering into it.
Schedule 1 – 3 (1) (d)
We welcome the appointment of a Board comprised of members appointed by the DHSSPS and such officers as the Regional Board prescribes.
Schedule 4 – 5 (c)
The nature of the PCC’s work will require proactive and credible engagement with local communities. This is likely to require a physical presence within each Trust area and the capacity to create committees or ad hoc groupings to advise/influence local and regional action.
Schedule 4 - 5 (f)
The DHSSPS may require to prescribe a local delivery system through which local community engagement is facilitated.
The HSSCs welcome the opportunity to comment on this important piece of legislation. We note however, the importance of the secondary legislation that will set out the detail of the relationships between the new bodies. This secondary legislation will be very important to the successful fit of the new structures. We look forward to the opportunity to being able to comment on future developments in due course.
Central Services Agency
The Central Services Agency would wish the Health, Social Services and Public Safety Committee (the Committee) to consider a proposal that the name of the body referred to in the Health and Social Care (Reform) Bill as the “Regional Support Services Organisation” be changed to the “Regional Business Services Organisation”. This change is suggested for the following reasons:-
1. The name contained in the Order should reflect the nature of the business being provided. “Support Services” does not adequately describe such professional services as those provided by solicitors, accountants, dentists, pharmacists, procurement specialists and human resources practitioners. These professional services are an integral part of the delivery of health and social care services.
2. In the private sector context the type of services provided by the new organisation would be regarded as partners with the primary services. The new organisation’s services provide the business underpinning to front line Health and Social Care practitioners.
3. The primary health and social care services are already supported by clinical support services, eg pharmacy laboratory, hygiene and disinfection services and it is important that these remain distinct from the non clinical business services.
4. The acronym, RSSO, for the new organisation could have an unfortunate and clearly unanticipated sound when it is used in that form to refer to the formal organisation. This would be inappropriate for a new public sector statutory body.
I would be grateful if you would ask the Committee to consider this proposal. Officers from the Agency would be happy to meet with you or to brief the Committee on this matter or any others relating to the CSA.
Ards Borough Council
The Department is seeking your views on the functions, constitution and governance proposals for the new Regional Health and Social Care Board.
The Council largely welcomes the functions, constitution and governance proposals of the new Board and is supportive of the Minister’s decision to prioritise investment, efficiency and public engagement. Further, it welcomes the proposed democratisation of the existing health structures, the intent to streamline services and the drive towards performance management. It is hoped that there will be effective liaison between the Board and local Commissioning Groups to avoid overlap in service provision.
The Department is seeking your views on the functions, constitution and governance proposals for the Local Commissioning Groups, including membership.
The Council continues to hold the view expressed in earlier correspondence with the Minister that LCGs should include an appropriate number of locally elected representatives. The Council is supportive of NILGA’s view that elected representatives should make up 50% of the members of each LCG to ensure that that the voice of public representatives is strong in an extremely professional and technical environment.
It is important that LCGs should link into the community planning process at an appropriate level.
The Council believes that each LCG should include a representative from the dental profession, given the current debate on the accessibility of affordable dental services. It would also like to see an optometrist appointed to LCGs.
The Department is seeking your views on the process for obtaining local government representation on the Boards of the Local Commissioning Groups.
The Council believes that local government representatives serving on LCGs should be appointed by local Councils themselves rather than via the Public Appointment route.
The Department is seeking your views on the functions, staffing and governance proposals for DHSSPS.
The Council welcomes the proposals to have more partnership focused relationships between DHSSPS, other central government departments and local authorities.
The Department is seeking your views on the additional functions, staffing and governance proposals for the common services organisation.
The Council welcomes the DHSSPS’ acknowledgement of the Bain Review on the Location of Public Sector jobs and encourages a move towards decentralising health related jobs to support local economies.
The Department is seeking your views on the proposal to create a Regional Public Health Agency and the functions it would undertake.
Integration. The Council broadly supports the creation of a Regional Public Health Agency (RPHA) as this has the potential to consolidate and integrate future public health planning and delivery in a way which could benefit health improvement and health protection. However, the level of investment in public health should be kept under review to ensure it remains proportionate to need. The relationships between Community Plans, Public Health Plans, Commissioning Plans and the mechanisms for ensuring mutual accountability between the sponsor organisations for each will be vital.
Caution may be necessary to ensure that regionalisation of public health and health improvement does not create new silos, but that the opportunity to bring about real multi-disciplinary, cross-agency and departmental working is utilised in a way which balances medical and social approaches to improve health.
Community Planning and Public Health. There is a relationship between the functions of the new Public Health Agency and the Community Planning and Well-being functions to be given to local government. The community planning process has potential to impact significantly on the wider determinants of health. The Council welcomes the fact that this is recognised in the consultation document. It is important that performance management and accountability frameworks put in place in respect of public health are able to align with those of the proposed future community planning frameworks. Freedoms and sanctions are mentioned and it is strongly recommended that consideration be given to the application of Local Area Agreements as used in GB between Central and Local Government to provide a suitable governance framework for the delivery of the broader health and wellbeing agenda.
The role of local government in community planning is expected to be driven in advance of RPA by the emerging local government modernisation agenda. Formal linkages would be beneficially established between emerging strategic community planning partnerships and the Department of Health and the Regional Public Health Agency at a regional level. Similar relationships should be established at a more local level linking local government and its community development partnerships with local offices of the Public Health Agency, Local Commissioning Groups and the HSC Trusts.
After a period of transition to allow the modernisation agenda to roll out, local government may take a co-ordinating responsibility for streams of community plans in order to bring about a co-ordinated overall community plan from the bottom up. Integration of the health stream into the community plan would be reinforced by the power to promote well-being and further strengthened when other functions, such as neighbourhood renewal, are transferred. It is paramount that the health improvement agenda should be fully integrated into the functioning of strategic and local community planning partnerships. For this reason the establishment of joint local public health units to provide support and expertise to the local community planning structure and process is seen as important.
It is envisaged that any joint local public health unit would be commissioned by the Local Commissioning Group to deliver local health improvement and health protection outcomes through for example, a local public health improvement plan. This should form an element of the overall community plan for the area. Therefore there would need to be formal (preferably legally constituted) relationships established between the local community planning partnerships and public health commissioning at all levels. Only if this happens can there be an effective accountability framework for the social aspects of any public health improvement plan and a framework within which there can be negotiated agreements on the plan at all levels and with the relevant partners.
Community Engagement. Community Engagement is a significant part of community planning and Councils are currently working on putting community engagement structures in place. There is considerable opportunity to integrate this work with the work of the Trusts and the new Public Health Agency to avoid unnecessary duplication and dissipated effort. There also needs to be a mechanism for ensuring that the community needs are reflected in decision making. It is suggested that this mechanism would need to extend beyond elected member representation and community representation on the Boards of Local Commissioning Groups.
There is little mention within the document of the role of the voluntary and community sectors, but clearly they have a significant role to play within the local public health agenda.
The Agency Structure. The proposal that The Regional Public Health Agency will support local government in improving the health and well-being of local communities is a very positive step that is welcomed by local government as a possible means to formalise access to expert advice, support, data and research.
It is vital that the Public Health Agency acts as an organisation that ‘spans the boundaries’ of its partner agencies and does not become seen, or see itself, as ‘the only body that does public health’. The Agency should be a ‘facilitator’ to help organisations link functions and outputs to health outcomes. There is mention within the document of co-location of the agency with Trusts, LCGs and local government. The council would recommend that this co-location should extend to establishing multi-disciplinary teams at regional and local level, with representation from partner agencies who can commit their organisations to joined up working on health improvement.
The Council contends that the multi-disciplinary team within the Agency should be as wide as possible and should include non-medical disciplines. An example would be the involvement of environmental health professionals, given that the review of the Public Health Function in 2004 recommended establishing Environmental Health Practitioner posts linking local government, regional health protection and health improvement bodies and Public Health departments. It is suggested that the concept of joint appointments with local government should be further considered at both regional and local level.
There will clearly be a challenge in bringing together these multi-disciplinary functions into one integrated organisation; particularly in creating a culture which facilitates co-ordination across disciplines and organisations from the outset. This needs to be considered in the design of the agency at this stage.
The Public Health Agency should also ensure it has a capacity to join in development of national and international policy and good practice. It would be beneficial if the Agency were to establish links with the World Health Organisation, the Public Health Observatory etc. to create a range of networks regionally, nationally and internationally.
If the Agency’s role is to be established by statute then, in addition to the proposed requirement for local government to consult with the RPHA on its community plans, a statutory requirement for the Agency to support local government would also be appropriate, given the other competing priorities that will exist. This should also include ensuring linkages between the commissioning framework and the community planning framework.
The Department is seeking your views on the proposal that, in the future, local government could be required, through legislation, to consult with the Regional Public Health Agency when developing its community plans.
It is clear that there needs to be co-operation between local government and the health service if the potential symbiosis of the respective roles is to be realised. A consultative role for the RPHA in the development of Community Plans would be welcomed given the scope for the public health agency to make a significant contribution to the evidence base for the community plan and to commit resources to common objectives. As currently proposed in the Ministerial announcement on RPA, local government will be the lead organisation in the development of the community plan which will reflect a wider range of community needs than health, although that aspect will obviously be of great importance.
The Department is seeking your views on the proposal to appoint the Chief Executive or a senior Executive of the Regional Public Health Agency as a non-Executive of the Board of the Regional Health and Social Care Board.
It is appropriate that there are strong links, effective liaison and good communication between the Regional Public Health Agency and the Regional Health & Social Care Board. If this is how these aims can be achieved, the Council would be supportive of the proposal.
The Department is seeking your views on the proposals for the Agencies referred to in Section 8.
The Council is supportive of proposals for the Agencies, provided a high level of efficiency and productivity ensues and that there is only a positive impact on the delivery of health services to the public.
The Department is seeking your views on the proposals for the two options, set out in Section 9, to replace the HSS Councils.
The Council welcomes the proposals in Point 9.2 and is keen to see locally elected representatives playing an active role in Patient Client Councils as was the case with the former Health & Social Services Councils.
The Council would prefer Option 2 (Point 9.5.2) – five separately constituted independent local bodies.
The Department is seeking your views on the constitution of the new organisation(s) under each of the proposed options, set out in Section 9, to replace the HSS Councils.
The Council, while satisfied in principle with the requirement that at least 4/10 of members are appointed from nominations from relevant District Councils, would wish to make sure that those appointed represent the entire geography of Northern Ireland.
Eastern Health and
Social Services Board
Introduction
The Eastern Health and Social Services Board welcomes the underlying themes of the review of Public Administration including reducing bureaucracy, simplifying systems and avoiding duplication. We particularly welcome the significantly enhanced profile for public health and well-being inherent in the package of proposals outlined in the consultation document.
At the same time, we recognise the challenges inherent in delivering the benefits of reduced bureaucracy in the context of the new organisational arrangements envisaged in the proposals. Addressing this challenge will be particularly important in terms of the interface between the new Regional Health and Social Care Board and Regional Public Health Agency where the functions formerly carried out, in the main by the HSS Boards, will move to one or other of these new organisations.
We would emphasise the importance, at the outset of the creation of new organisations, of recognising the decades of integration of health and social care here, the advantages of which have been recognised locally and much further a field for many years. Close collaborative working between the new organisations and other stakeholders will be a prerequisite to successfully improving the health and well-being of the people of Northern Ireland. It is critical in particular that there is the closest possible strategic and operational collaboration between the Regional Board and the Regional Public Health Agency.
As such, we would particularly urge that this partnership be recognised in the organisational arrangements and remit of the new regional agency with a lead role for health and well-being. It is our view also that the title of this new agency should recognise and reflect the complementary perspectives and contributions of both medical and social models of health and well-being.
In responding to the detail of questions posed in the consultation questionnaire, we have premised our responses on the view that form follows function. As such, we are unsure whether the outworking of our response could mean that the distribution of staff across the proposed new structures might differ somewhat from the particular distribution suggested in the consultation document. However, we believe the total number of staff remaining after the completion of the reforms would remain in line with that envisaged in the consultation document.
Regional Health and Social Care Board (RHSCB)
- The core functions of the RHSCB should be commissioning, performance management and improvement and financial management.
- The RHSCB should be accountable to the Minister against a clear framework of objectives subject to the Minister’s approval.
- There should be minimum duplication between the role of the RHSCB, the Department, the RPHA and HSC Trusts.
- The Department should give due consideration to transferring responsibility for professional education and training and for workforce planning to the RHSCB.
- Due consideration should also be given to transferring to the regional board responsibility for capital planning and negotiation of Family Practitioner contracts.
- Trusts should report directly to the new RHSCB.
- The perspectives of the senior personnel accountable for core professional and business functions should be represented on the board of the RHSCB.
- The RHSCB must have a Director of Social Services to allow the Chief Executive of the RHSCB to be assured that appropriate social care services are commissioned for the safe discharge of statutory functions for children and vulnerable adults.
- The range of commissioning functions to be carried out should equate to the spectrum of commissioning activities carried out by existing Boards.
- Commissioning arrangements should:
- Deliver improved health and well-being / reduced inequalities
- Be locally focussed, regionally coherent and evidence-based
- Draw on the necessary range of multi-professional expertise
- Be organised efficiently and effectively through flexible teams
- Have access to all relevant information sources
- Make adequate provision to ensure specialist / vulnerable services are protected and developed
- LCGs should be fully involved in performance management and improvement.
- Commissioners should have Government and Departmental support to use appropriate incentives and sanctions with Providers (including tariffs) to achieve the maximum possible return on the investment of public funds.
- There must be a holistic approach to commissioning, embracing both services and public health and well-being dimensions.
- There should be the closest possible collaboration between the RHSCB and the Regional Public Health Agency (RPHA), enhanced by co-location of staff and appropriate designation of workload.
- Funding for health improvement initiatives should flow through the commissioning process from the RHSCB to the RPHA in most instances.
- Appropriate statutory functions carried out currently by Boards should transfer to the RHSCB in any circumstance where the action necessary to fulfil the statutory functions is wholly or mainly carried out by Trusts.
- Due consideration should be given to relocating to the RHSCB the Local Supervising Authority (LSA) role in respect of the Statutory Supervision of Midwives and to ensuring appropriate arrangements for incorporation of the LSA Responsible Officer position within the RHSCB.
- RHSCB should be accountable for the management of contracts for the provision of Family Practitioner Services (FPS), including the commissioning of National and Directed Enhanced Services with Local Enhanced Services through LCGs.
- Performance management, professional development and oversight of governance arrangements for Family Practitioner Services should also rest with the RHSCB.
- Transactional functions for FPS, such as payments and list management, should be based in the Central Services Organisation.
- FPS input to the Regional Public Health Agency should be provided on a sessional basis, using co-located staff.
Local Commissioning Group (LCGs)
- LCGs should have the lead role in engaging communities in identifying commissioning priorities and improving health and well-being.
- The majority of services should be commissioned locally, LCGs committing the necessary resources to allow identified specialist services to be secured on a regional basis.
- LCG staff should be locally based and co-located with those staff from the RPHA and CSO whose work has a direct bearing on commissioning and health improvement for local people, to ensure close collaborative working at grass roots level.
- In the immediate future LCG boundaries should preferably be co-terminus with those of the 5 HSC Trusts. In the medium term LCG boundaries should also reflect the reform of local government and, as far as possible, other elements of public service.
- As committees of the new RHSCB, LCGs should have their roles and responsibilities set out in schemes of delegation, including accountability from the LCG to the Board for statutory functions.
- The Chairs of LCGs should report to the Chief Executive of the RHSCB in line with the requirements of accountability for statutory functions and the role of accountable officers.
- The RHSCB should approve each LCG’s Annual Commissioning Plan and monitor its performance.
- Members of LCGs should be appointed on the basis of merit and competency and reflect an appropriate range of professional and social backgrounds and local identities.
- There should be 2 social care professionals on each LCG to reflect the range of adult and children’s issues.
- The RHSCB should ensure that appropriate senior support and expertise is available to LCGs along with the necessary support staff and range of commissioning skills in functionally viable units.
- The merit principle should underpin the selection process to LCGs in respect of local councillors in accordance with the Office of the Commissioner for Public Appointments NI Code of Practice.
Central Services Organisation
- The Central Services Organisation (CSO) should be a separate legal entity with the accountability arrangements as proposed with the exception that the commissioning and management of FPS should rest with the RHSCB and not with the CSO. We are also of the view that the research and development function should be housed within the CSO.
- We support the concept of a ‘hard charging’ regime.
Regional Public Health Agency
- The three domains of public health should be integrated and co-located to facilitate both local and regional working alongside staff from the other relevant organisations wherever possible.
- The designated role and responsibilities of the Director of Public Health are such that, in the structures proposed, statutory public health functions could only be discharged by the RPHA.
- The social care contribution to the public health agenda should be recognised and further developed through the work of the RPHA.
- There should be:
- adequate specialist staffing with appropriate training and qualifications and adequate support
- capacity for health intelligence, including links to the Central Services Organisation information resources and relevant resources in other organisations
- Strong public health input/presence in the five proposed local commissioning groups
- Ability to relate to the five Trusts and the proposed eleven councils
- Strong links with the DHSSPS in terms of policy and strategy development and with the All Ireland Public Health Observatory, the Cancer Registry and relevant Departments at QUB.
- Further consideration is required regarding how locally elected representation from eleven potential constituencies would work in practice on the Board of the RPHA.
- The commissioning of health improvement should be undertaken by the RHSCB in collaboration with the RPHA
- A central health protection unit within the RPHA should ensure an effective presence and mechanisms at local level regarding links to environmental health and 24 hour on-call rotas.
- Northern Ireland should maintain a formal link with the Health Protection Agency in regard to communicable disease control services.
- There should be formal contractual arrangements between the RPHA and the RHSCB for securing public health involvement in commissioning
- RPHA staff should be integral members of commissioning teams at LCG and RHSCB levels.
Relationships between Organisations / Sectors
- Trusts should have public health / health improvement specialist leadership embedded to ensure that health improvement / community development is not peripheral to their agenda.
- Legislation should identify appropriate organisations / sectors with whom local councils should consult when preparing community plans, including but not limited to the RPHA, RHSCB, and LCGs.
- If legislation is to be introduced to underpin collaborative working between the RHSCB and the RPHA, then the requirement should be for the regional board to take due regard of the advice of the RPHA rather than just to consult.
- The Director of Public Health, employed by the RPHA should serve as a non-executive director of the RHSCB and the Director of Social Services employed by the RHSCB should serve as a non-executive director of the RPHA.
- We are broadly supportive of the proposed merging of agencies into a common services organisation. However, the NI Guardian ad Litem Agency and the NI Social Care Council were established to sit outside the main “commissioning and provider organisations” so that they could have a professional “challenge function”. Their incorporation into a common service organisation would question this key role.
- In terms of the new Patient and Client Council we favour a single independent regional body with clear local identities and flexibility for managing its agenda and work : in essence a “hub and spokes” model.
- The new consumer body should have the right to attend and participate in meetings of the RHSCB and RPHA.
Q1. The Department is seeking your views on the functions, constitution and governance proposals for the new Regional Health and Social Care Board.
Response:
Functions of the Board
The Eastern Health and Social Services Board believes that the core purpose of the RHSCB will be to improve the health and well-being of the people of N.Ireland. We agree that the core functions of the RHSCB should be commissioning, performance management and improvement and financial management. We agree also that the range of commissioning functions to be carried out through the RHSCB/LCGs should equate to the spectrum of commissioning activities currently carried out by the existing Boards.
The Eastern Board is of the opinion that appropriate Statutory functions carried out currently by HSS Boards should transfer to the RHSCB in any circumstance where the action necessary to fulfil the Statutory functions is wholly or mainly carried out by Trusts. The majority of such functions relate to Social Care activity. We feel that more should have been said in the consultation document about the importance of the statutory Social Services functions in relation to children where there is a long history of attention. More should also have been said about commissioning services from a social care perspective with a view to improving well-being and independence of patients and clients as well as their health and focusing more Trust attention on protecting vulnerable people be they elderly or disabled or the victims of trauma or domestic violence.
Due consideration will also need to be given to relocating to the RHSCB the Local Supervising Authority (LSA) role in respect of the Statutory Supervision of Midwives and to ensuring appropriate arrangements for incorporation of the LSA Responsible Officer position within the RHSCB.
We consider that it is also essential that the RHSCB would be accountable for the management of contracts for the provision of Family Practitioner Services, including the commissioning of National and Directed Enhanced Services with Local Enhanced Services through LCGs. Performance management, professional development and oversight of governance arrangements for Family Practitioner Services would rest with the RHSCB.
In essence, our view is that:
- There are clear synergies in having most FPS staff together in one organisation.
- All professional and development staff should be in the RHSCB.
- Information Management staff working in FPS should also be in RHSCB particularly if other Information Management staff involved in commissioning are so located.
- Transactional functions such as payments and list management should be based in CSO.
- FPS input to RPHA could be provided on a sessional basis and using co-located staff.
The Board agrees that strong performance management and improvement should be a key function of the proposed Regional Board. We would add, however, that the focus should be on creating a culture of continuous improvement across the full spectrum of services that are commissioned. It is essential, therefore, that commissioners, both local and regional, should do their commissioning in a way that has performance management as one of its aspects. Commissioners should be fully involved in performance management and improvement so that this is not seen solely as a regionally driven centralised activity.
The Eastern Board endorses the proposed significant financial management role of the RHSCB. For commissioning to be effective it is essential that commissioners have Government and Departmental support to use appropriate incentives and sanctions with Providers (including tariff) to achieve the maximum possible return on the investment of public funds. Whilst we recognise the importance of ensuring the maintenance of Trust financial viability, we believe it is essential that ensuring responsible service development, reform and improvement is seen as the primary public interest.
In terms of commissioning, the approach must be holistic and embrace both services and public health and well-being dimensions. This will require close collaboration between the RHSCB and the RPHA. A clear understanding also needs to be developed regarding the range of functions encompassed by the term commissioning since the perception of the purpose and scope of commissioning very much affects how it will be organised. In our view the following principles should underpin our approach to commissioning in the particular circumstances of Northern Ireland:
Local Population focused but regionally coherent
Commissioning is about planning, procuring and performance monitoring services for ‘populations’ based on an understanding of their health and well-being needs, their expectations, the pattern and quality of the service they experience at present and the potential for service improvement and reform. The ‘populations’ relevant to any service can be local, sub-regional or regional – depending on the issue under consideration. In circumstances where needs, expectations and ability to provide effective interventions changes, Commissioners need to continuously re-negotiate priorities with local stakeholders and strike a balance between their wish to innovate and serve needs locally and the responsibility to contribute to regional service coherence where that is important to the population.
High added-value Commissioning expertise
The Purpose of Commissioning in the health and care context is: Improving health and well-being and reducing inequalities.
The Business of Commissioning involves:
- Assessing the health and well-being needs of groups, populations and communities of interest;
- Prioritising needs within available resources;
- Building the capacity of the population to improve their own health by partnership working on the determinants of health in local areas;
- Working with other key stakeholders in planning health and care services to meet current and emerging needs;
- Securing - through Service Level Agreements and Contracts, the delivery of efficient health and social services.
- Ensuring that services meet good standards for safe, quality care - with particular refer to Service Frameworks, where these are available;
- Using investment and performance management to develop and reform services.
Commissioners need a high level of local knowledge to allow them to work with and challenge where necessary, providers and other stakeholders. They need also to have expertise of a variety of kinds not often embodied in one individual so commissioning must be seen as a multi-professional function combining expertise from: social care; nursing; allied health professionals; public health; family practitioner services (dental, pharmacy, medical, optometrics); finance, information, contracting and service planning. Commissioning needs to be evidence based and, therefore, commissioners need to have predictable, regular sources of research / information / intelligence as a core support to their work. As a matter of principle, we believe that all relevant health and social services organisations should have access to the appropriate range of information sources, regardless of where in the system the information is collected and/or held.
Effective and efficient
Commissioner organisations need to cover a very broad agenda expertly but with constrained numbers of staff. Individuals, therefore, need to operate as members of dedicated Teams that are ‘light on their feet’ to be able to develop, maintain and mobilise their expertise. At the same time, the individuals who make up teams need to bring their expertise to a number of Teams for different purposes. This requires significant workload planning and flexibility. In order to commission effectively it is important that the design of the new system takes account of these considerations.
A key principle of the model for commissioning that we favour is subsidiarity i.e. services should be commissioned as locally as possible. For some services, however, commissioning is more appropriately organised at an ‘all Northern Ireland’ level. The regional mechanisms to support ‘all N.I.’ commissioning would, of course, need to ensure that local commissioners were fully engaged in the processes so that they could represent the interests of their local population and commit resources as necessary to region wide plans that were agreed. Examples of circumstances where regional or N.I. wide commissioning would be appropriate are:
Where services are characterised by financial risk through being small in scale, costly and either unpredictably distributed or highly clustered. Examples of such services are those for Haemophilia, Enzyme Deficiency Disorders and specialist Forensic Psychiatry;
Where certain services for adults or for children are of small scale and therefore vulnerable and where a fairly secure pattern of commissioning is required to ensure continued viability in service provision in Northern Ireland. Examples would include Genetic Services, Special Eating Disorder services and Specialist Child and Adolescent Mental Health services;
Where regional monopolies exist and where commissioning needs to be coordinated in order to maximise leverage. For example Plastic surgery, Neurology and Cardiac Surgery. These services need strong performance management to bring the contestability that otherwise might be brought by there being alternative providers.
Where services for Looked After children, for example Fostering, Adoption and Secure Accommodation, require a regional perspective to ensure that statutory functions are met consistently. The proposed model would allow local input and flexibility (and maximize local commissioning) so that vital links with other services, including primary care, are maintained;
Where Family Practitioner contracts are concerned, these would be best held regionally but managed by locally based staff, allowing local input which is vital to such provision whilst minimising conflicts of interest.
HSS Boards have, as an example of collaborative Regional Commissioning, the Regional Medical Services Consortium which they have operated for many years and which can act as a good model on which to build for balancing local and regional interests.
As already acknowledged, it is important that new commissioning arrangements are rooted in good local knowledge and expertise. For this to be effective, the Board strongly supports the view that the majority of RHSCB staff supporting local commissioning should, as far as is practically possible, be locally based. In the model proposed in the consultation document and in light of the principles underpinning commissioning described earlier, it would be essential that locally based RHSCB staff would be co-located with colleagues from the RPHA and CSO whose work has a direct bearing on commissioning and health improvement for local people.
In paragraph 7.6 of the consultation document it is stated that “the RPHA would be commissioned directly by the Minister or through the RHSCB, to provide public health programmes and initiatives at a regional and/or local level”. The Eastern Board would be concerned that this section needs to be clarified. We agree with paragraph 4.4.3 which states that “the proposed arrangements present a major opportunity to have commissioning that focuses on promoting health and wellbeing and not simply securing health and social care services”. In our view, for health improvement interventions to be effective, they must be responsive to the varying needs and characteristics of our diverse communities. Therefore, those needs must be identified at local commissioning level and effective interventions commissioned and implemented at that level. It will be entirely appropriate, of course, for the design of various health promotion initiatives to be undertaken centrally to meet key Ministerial objectives. However, successful implementation cannot be achieved on a regional standardised basis insensitive to local circumstances. Therefore, to support this approach it will be essential that the majority – and preferably all - funding for health improvement initiatives flows through the commissioning process i.e. from the RHSCB to the RPHA.
Constitution
The Board supports the application of the principles of good governance, with a focus on the quality of care for patients and clients, accountability, transparency, efficiency and effectiveness. This is essential in the context of a body responsible for the commissioning, performance and financial management of health and social care services to the value of over £3billion per annum.
The consultation paper proposes that the board of the RHSCB should comprise a Chair appointed by the Department, Non-Executive Directors appointed by the Department including the Chief Executive or a senior level Executive in the proposed RPHA (Section 7), a Chief Executive; and such other officers as may be prescribed having regard to the above principles of good governance. The Eastern Board agrees with these proposals.
The conduct of Board business would be framed in a best practice set of Standing Orders and Standing Financial Instructions.
In terms of executive director membership of the Board, it is essential that the perspectives of the senior personnel accountable for core professional and business functions of the Board are represented at the decision making table. By the same token, we believe it is important that Chairs of local LCGs report to the Chief Executive of the RHSCB so as to ensure clarity regarding lines of accountability for statutory functions and the role of accountable officers.
Governance
The Board endorses the proposal that the RHSCB would have a very clear management remit with both the power and the authority to act on behalf of the Minister in striving for significant improvements in efficiency and performance throughout the health and social care system to bring about improved services to patients, clients and carers.
The RHSCB should be accountable to the Minister against a clear framework of objectives which would be subject to the Minister’s approval with regular monitoring reports to show progress against these. It is imperative that there is also minimum duplication between the RHSCB and the Department, so that there would be the clearest possible accountability and governance. In particular, the Board endorses the proposal that the six HSC Trusts would report directly to the new RHSCB.
Within this context, it will be important to ensure, from a performance management perspective, that those statutory functions delegated by the RHSCB to Trusts under the HPSS (NI) Order 1994 are discharged appropriately, to agreed standards. These statutory functions include, for example, being the corporate parent of looked after children. This encompasses not just the provision of physical care, but includes an obligation towards all aspects of the needs of these children.
To allow the Chief Executive of the RHSCB to be assured that appropriate social care services are commissioned for the safe discharge of these statutory functions for children and vulnerable adults we believe the RHSCB must have a Director of Social Services.
Unlike the position for other professions, social work training (pre and post qualifying) is commissioned at Board level. In order to maintain and develop a skilled professional and competent social services workforce, fit for purpose, it is imperative that the commissioning of personal social services training resides within the professional domain in the RHSCB. Quality, safety and effectiveness are central to the government’s modernisation agenda and the commissioning of training makes a significant contribution to this objective and is integral to sound governance practice, risk management, workforce planning, service development and ensuring safe and accountable practice. The commissioning of training involves close partnership with the Northern Ireland Office and the Department of Education to ensure that regional strategic plans are supported by an appropriately qualified workforce.
Q2. The Department is seeking your views on the functions, constitution and governance proposals for the Local Commissioning Groups, including membership.
Response:
Functions
We endorse the Minister’s proposals that LCGs should have a holistic focus, addressing both health and wellbeing inequalities as well as securing health and social care services.
At the heart of the Minister’s proposals is a recognition that the needs of local populations differ and the pattern of current service provision varies from place to place. It is important, therefore, that the new commissioning arrangements are locally focused and are rooted in good local knowledge and expertise. By extension this will require budgets devolved to appropriately constituted Local Commissioning Groups with responsibility for addressing the needs of their local population while working within coherent regional policy and strategy frameworks, available resources and performance targets.
Whilst the majority of services should be commissioned locally, we believe that LCGs should work collaboratively to commission certain services, which, by virtue of their specialist nature, small scale or statutory accountability, should be commissioned regionally. This would involve LCGs agreeing commissioning priorities and committing the necessary resources to secure these services.
We would endorse the view that significant planning, purchasing and performance management responsibility would therefore be positioned with LCGs (paragraph 4.4.3). It is essential to ensure close collaborative working at grass roots level that staff are in the main locally based and co-located with those staff from the RPHA and CSO whose work has a direct bearing on commissioning and health improvement for local people
We agree that the process of commissioning should have “very strong links with local communities, with voluntary and community sector organisations and the engagement of communities in securing the health and well being of their people”. If local commissioning is to be truly meaningful it will be vital that LCGs engage in a meaningful way with all relevant stakeholders – service users, carers, community and voluntary groups, the wider public, and particularly ensuring that those who often have ‘no voice’ are listened to. It will therefore be essential that, whilst all organisations must engage with stakeholders, the RHSCB and its LCGs have the responsibility and are the overall lead for this. This will involve working closely with other organisations, Trusts, RPHA and other statutory organisations so that duplication is avoided and the potential outcome of any engagement maximised.
Constitution
Our preference would be for LCG boundaries to correspond to those of civic society as alignment with natural communities and their needs is of fundamental importance, including a focus on partnership with local government in respect of community planning.
We recognise the advantages of having 5 LCGs boundaries co-terminus with those of the 5 current provider organisations and would support such an arrangement as the best option at present. However, we recognise that when the new local government boundaries are determined, if these are not co-terminus with provider organisations, consideration may need to be given to the boundaries of provider organisations.
It will also be important in future arrangements that the boundaries of LCGs reflect, as far as possible, co-terminosity with other elements of public service that impact on health and wellbeing, including housing, education and police. This arrangement would still allow meaningful alignment with Trusts as individual LCG commissioning will always be across Trust boundaries in keeping with patient movement and care pathways.
In paragraph 4.4.3 (constitution of LCGs) it is stated that LCGs would operate “as committees of the new RHSCB who would determine the detail of the LCGs role and responsibilities”. We believe it would be constructive and in line with the emphasis that the consultation document places on local commissioning for the roles and responsibilities of LCGs to be set out in standing orders and schemes of delegation. Beyond this, the number of LCGs would be a matter for the RHSCB to determine having due regard to the final outcome of the review of the number of government local councils and the merits of further change in the number of LCGs.
Membership
The Board supports the Minister’s comments in the Consultation Paper that LCG Membership “would be constituted to have a good spread of expertise with a bias, in terms of numbers, favouring those with close (preferably daily) contact with the local population but they should also not be too cumbersome”. In respect of LCG Membership, it is important that this has broad-based professional involvement from a range of health and social care practitioners.
We would offer the following comments on the suggested model:
- The proposal to have 4 General Medical Practitioner members is welcomed. We would add that Family Practitioner members should not be permitted to also hold any posts that would lead to conflicts of interest.
- We regret however that Social Care professionals and Lay members have been reduced to one member each and would strongly recommend that there should be 2 social care professionals to reflect the range of expertise required in both adult and children’s services.
- With regard to dentists, nurses and optometrists we would stress the importance of maintaining a balance of available professional expertise across LCGs.
- We also note the very valuable contribution and perspectives of Lay Members in particular as they can bring an independent perspective to bear and reflect the views of relevant interests e.g. local maternity liaison groups.
- In relation to the Pharmacy representative, we are of the view that this should be a Community Pharmacist.
- The Chair of each LCG should be appointed on the basis of merit and competency.
- We welcome the continued involvement of Public Health, Social Care, Allied Health and Nursing members as they make an important contribution to LCGs by having a broad based knowledge of care needs, service provision models and performance.
- Public Health, Social Care, Allied Health and Nursing members should be deployed in commissioning roles and not service provision (otherwise this will create unhelpful conflicts of interest).
- We recognise the value of having Public Health, Social Care, Allied Health and Nursing members appointed on the basis of merit and competency to each of the LCGs rather than being nominated.
- We welcome the proposal to have elected local representatives as members of LCGs and would concur that such appointments should be consistent with the merit principle in accordance with the Office of the Commissioner for Public Appointments NI Code of Practice.
- It will be important that the governance arrangements for LCGs require regular attendance by all members to ensure effectiveness in carrying out their work.
- There is value in ensuring that members are drawn across a wide social background and geographical area throughout each LCG area.
- Reflecting the importance of local commissioning, the RHSCB should ensure that appropriate senior support and expertise is available to LCGs.
- The consultation document states that professional members should have expertise across all the programmes of care, but singles out mental health and learning disability as being particularly important. We feel that it is unhelpful to specify these as, whilst mental health and learning disability are current priorities, there may be different priorities in future years.
- It will be important that members of the new LCGs, including locally elected representatives, have early and continuing access to a rigorous commissioner development training programme.
Support to LCGs
The effectiveness of LCGs will be influenced significantly by the commissioning staff available to support them and in particular the need for close proximity to staff with skills in areas such as information, strategic planning, performance management, procurement, financial control, monitoring and regulation.
We believe that staff in the proposed RHSCB should wherever possible be locally based in a number of centres across Northern Ireland to facilitate close relationships with LCGs and in the interests of building local agendas into coherent regional approaches.
This raises a fundamental question: firstly how to get staff from the RHSCB, RPHA, CSO as well as other bodies – in particular environmental health and community development in local government – working effectively together, serving common objectives and using integrated systems wherever possible. We believe the Minister’s emphasis on close involvement with local government to be entirely correct and to offer great potential. To realise this potential we would propose the following model:
- The need for the RHSCB, RPHA and CSO to be based together in functionally viable units located across Northern Ireland and spanning all the main health improvement and protection, commissioning, service performance and common service functions.
- Only those functions at the most senior or most specialised level would be in a central location and there would be merit in examining the potential for such posts in the RHSCB, RPHA and CSO to be in the same single location. We believe this to be both an efficient as well as effective model for staff deployment as those staff who need day and daily proximity to the communities they serve would also have roles in contributing to work at a regional level, as proposed in the consultation document.
- A common vision and shared priorities and objectives along with clear lines of accountability will be required to enable all the proposed new organisations to work together effectively.
- In addition we would also propose that local government environmental health and community development staff, who make a significant contribution to health protection and health improvement should also be co-located with their colleagues from the regional Board and RPHA.
Governance
We would endorse the proposed role of the RHSCB as ultimately accountable for the outcomes of commissioning functions discharged by LCGs, including statutory responsibility to contain expenditure within allocated resources. We are of the view that the Chair of the LCG should be accountable to the Chief Executive of the RHSCB.
Furthermore, we support the proposals that the RHSCB would approve each LCG’s Annual Commissioning Plan and would be responsible for monitoring its performance. In our view, LCGs will be key to the continued development of services commissioned from Family Practitioners. It makes sense that contracts would be managed locally but held regionally to avoid conflicts or perceived conflicts of interest. We also support the proposal that LCGs would have delegated responsibility – through an Operating Framework or Scheme of Delegation - to commission services for the population they cover, including the development of proposals to ensure the active engagement of the range of primary care professionals and the wider community. Moreover the Operating Framework or Scheme of Delegation should make clear the accountability from the LCG to the Board for statutory functions and the role and powers of LCGs in holding others to account in terms of performance management, quality and standards and health improvement.
The reformed LCGs should be established as rapidly as possible and in tandem with the RHSCB. It is vital that the LCGs are in a position to commission effectively for the financial year 2009/10 onwards and therefore would require a minimum of lead- in time of 6 months prior to that (albeit in shadow form).
We believe that, in addition to the core commissioning functions already identified, the following will also be key roles for the new LCGs:
- work with Independent Practitioners, the Community and Providers to reshape and modernise care service delivery
- advance aspects of performance management & quality management e.g. working with Primary Care to challenge variations in referral practice and developing Local Enhanced Service Initiatives
- targeting and addressing inequality in health status of groups/communities or service provision (gaps)
Q3. The Department is seeking your views on the process for obtaining local government representation on the Boards of the Local Commissioning Groups.
Response:
We welcome moves to increase democratisation within the system and enable enhanced involvement of local government in improving the health and wellbeing of local communities. However the partnership with local government needs to be much more integrated with the functions of local government if the optimal impacts on public health are to be realised.
We agree that the merit principle should underpin the selection process to LCGs in accordance with the Office of the Commissioner for Public Appointments NI Code of Practice. It will be important to ensure that all members understand their roles and responsibilities and that conflicts of interest are avoided.
We believe that due regard should be given to the need for local elected representatives appointed to the LCGs to be geographically representative and to have a knowledge of health and social care.
In addition, recognising the challenges for elected representatives in balancing their many public and personal commitments (some may also be MLAs or MPs), it will be essential to ensure continuity and stability of membership (within their period of election). As with all members, they should be committed to their role in the LCG.
Q4. The Department is seeking your views on the functions, staffing and governance proposals for DHSSPS.
Response:
In general, we agree with the responsibilities for the Department outlined in the consultation paper and would stress that the Department needs to employ sufficient staff from all relevant professions to provide advice to the Minister and actively be involved in the formulation of policy, ensuring that it is both evidence-based and achievable by the HSC. We believe that the roles and functions of the Department should be clearly focussed to avoid potential for role confusion and uncertainties about accountability. In particular, we are of the view that the Department should give due consideration to transferring to the RHSCB responsibility for professional education and training and for workforce planning. It should also be the case that responsibility for capital planning would be transferred to the regional board, along with responsibility for negotiation of Family Practitioner contracts, in line with practice elsewhere.
Q5. The Department is seeking your views on the additional functions, staffing and governance proposals for the common services organisation.
Response:
The Board would be supportive of the proposal to have a shared services organisation. The Board would also support the determination made following consultation in September 2007 with regard to the business of the organisation. We would agree that this should include the common business functions of Human Resources, Finance, Estate Management and Maintenance, Information Technology, Procurement and CSA Legal Services. Information Management for the commissioning process should rest with the commissioning organisation. This should include information analysis to support contract management of Family Practitioner Services (FPS) by the Board.
With regard to the additional services proposed for the Common Services Organisation (CSO), the Board would be supportive except that, as noted above, the commissioning and management of FPS should rest with the Board. We are also of the view that the research and development function for HSS should be based in the CSO as opposed to being located within the Department.
The Board agrees that the CSO should be a separate legal entity with the accountability arrangements as proposed. We would also support the concept of a ‘hard charging’ regime.
In relation to complaints handling, an earlier DHSSPS consultation on Complaints recommended the removal of the Independent Review stage from the HSC organisations with direct referral following local resolution to the NI Ombudsman. We are of the view that, albeit not featured in the consultation paper, there exists the potential for a new Common Services organisation, on behalf of the Regional Board, to effectively provide an independent HSC wide second stage complaints handling process. It is regrettable that the opportunity for the proposed CSO to handle this work on behalf of HSC organisations appears to have been missed.
Q6. The Department is seeking your views on the proposal to create a Regional Public Health Agency and the functions it would undertake.
Response:
We strongly endorse the fundamental principle of putting the public health agenda at the heart of the Health and Social Care system. The Regional Public Health Agency should be resourced to ensure that it has the capability to deliver on the challenging agenda. It is important to emphasise in this regard that statutory functions relating to public health could only properly be undertaken with an appropriately qualified and adequately staffed public health workforce accountable through a Director of Public Health (with all the roles and responsibilities which go with this designation across the UK). In the structures as proposed, statutory public health functions could only be discharged by the Regional Public Health Agency (RPHA).
The functions of Public Health are clearly the three domains as defined by the Faculty of Public Health delivered by teams of multidisciplinary appropriately trained public health staff working with adequate support. We recognise the benefits of public health working within a critical mass. The critical mass is essential for training future generations of the multidisciplinary workforce and for continuing professional development.
It is also important that the 3 domains are integrated and where possible co-located for both local and regional working. Co-location must include staff from the other relevant organisations.
The RPHA must be equipped to deliver on the public health functions of health improvement, health protection and service development both locally and regionally with appropriate capacity for health intelligence, evidence based practice, population needs assessment, strategic planning, leadership, community development, advocacy and research.
The elements envisaged within public health and linkages proposed represent an increase in expectation of the role and functions compared with current functions e.g. input to local government community planning. To ensure that it is possible to deliver on the agenda the public health workforce must have adequate specialist staffing (with appropriate training and qualifications) and adequate support (also relevant where staff are out-posted).
The establishment of a Regional Public Health Agency covering all domains of Public Health has the potential to be the platform to deliver on the agenda however it cannot function solely as a regional central entity. Such an agency must have the ability to work at both a regional and local level in all three domains. In effect, this means there must be a strong public health input/presence in the five proposed local commissioning groups, an ability to relate to the five Trusts and the proposed eleven councils in the context of community planning and new environmental health structures, to work with the regional commissioning agenda and to deliver on the health improvement agenda. The RPHA would also have strong links with the DHSSPS in policy and strategy development.
The working environment has an added element of complexity when staff employed by one organisation would be expected to spend an agreed amount of their working time within other organisations. Clear rules of engagement and managerial and professional accountability would be required. Particular attention would be required in regard to the arrangement for those staff who could be employees of the RPHA and LCG Board members.
RPHA Board
The document does not clearly define the Board structure of the Agency. It is suggested that the Board of the RPHA would have input from locally elected representatives. Given that this is a regional agency as is the Regional Health and Social Care Board where local representatives are not to be Board members, further consideration is required regarding how locally elected representation from eleven potential constituencies would work in practice on the Board of the RPHA.
In order for an RPHA to be an authoritative source of information on the health of the public it would have to have a strong information base and information specialists in support. It would be important to consider how the All Ireland Public Health Observatory should be linked to the agency. There would also have to be very strong links to the Northern Ireland Cancer Registry and the recently created Centre of Excellence awarded to the QUB Department of Epidemiology and Public Health and the Institute of Public Health. Further consideration should be given to developing the potential for ‘all Ireland’ collaborative public health working.
Management information in health protection, surveillance and hospital acquired infection should be integral to the RPHA. There should also be links to relevant information from other sources such as education, justice, social development and voluntary organisations.
As indicated earlier there is also the need to have full access to input from the information resource in the CSO.
Health Improvement
The commissioning of health improvement should be undertaken by the RHSCB in collaboration with the RPHA. The RHPA should also provide a range of health improvement functions and should be adequately resourced to undertake all these functions. The organisation should have the flexibility to respond to urgent issues when they arise.
The RPHA would be the organisation through which significant regional and local inter-agency working will take place. It is important that this work continues to be informed by an ethos that is user and carer focused. The continuation of health improvement collaborative work such as Healthy Cities, HAZ and Investing for Health should be maintained and supported through the RHPA (see also response to Question 7).
Social services staff play a central role in the promotion of well-being and should occupy a significant role in the work of the RPHA. The social care contribution to the public health agenda should be recognised and further developed through the work of the RPHA. We would wish to see a strong social services presence in the RPHA and would recommend a change of the proposed organisation’s title to reflect those issues of wellbeing that are not public health.
We also believe that, to promote close working relationships between RHSCB and RPHA, staff should be co-located. Specific attachments of senior social services staff from the RHSCB would also have potential benefits:
- Assist the RPHA in promoting health and well-being by ensuring that social services staff are actively involved in its work.
- Assist the RPHA to address the public health implications of child protection and safeguarding issues.
- Promote continuity and build on existing arrangements where social services staff are currently involved in successful health and well-being improvement programmes, community development and emergency planning.
- Ensure that the governance issues relating to the employment of social workers and social care staff are fully addressed.
There would in our view also be merit in having a debate as to the advantages and disadvantages of locating the Safeguarding Board for NI in the RPHA, whilst the commissioning responsibility would continue to rest with the RHBSC.
Health Protection
It is recognised that there is considerable strength in the creation of a Health Protection Unit in RPHA which should cover communicable disease surveillance, health care associated infection surveillance, responding to health protection incidents whether communicable disease related or of an environmental nature and emergency planning.
There are inherent risks in the development of a central unit without effective presence and mechanisms at local level and these are:
1) Loss of strong local links to local environmental health. These linkages will be important with the emergence of changing local council structures and their impact on environmental health structures. Safeguards must be in place to continue to secure strong local knowledge and more importantly working relationships.
2) The provision of a 24 hour on-call rota for health protection must be retained. There is currently 24 hour on call provision in a number of tiers (4). The second on-call, currently at each of the 4 Boards, provides the dual function of consultant cover for the first on-call (usually a trainee in Public Health) and knowledge of the local system. Movement to a Northern Ireland wide rota provided by a central unit would require careful consideration of how to maintain the existing strong local knowledge.
Within the proposed new arrangements all CCDC staff could be employed by the RPHA (the staff of CDSC NI are currently employed by the health Protection Agency). It would be essential that Northern Ireland maintains a formal link with the Health Protection Agency which could be secured via a robust Service Level Agreement.
Public Health, Commissioning and Policy Development
We fully support the importance of the public health role in the commissioning domain. We would contend that strong commissioning for consistent evidence-based practice, advancing patient safety and outcomes, service redesign and service improvement requires public health to be an integral component of commissioning and not an “arms length” advisory support role.
To ensure embedded public health in commissioning (and not public health advice as an option) there will be a requirement to have formal contractual arrangements between the RPHA and the RHSCB. Public Health staff will be both members of LCGs and be directly involved in the work to support the LCGs and the RHSCB in their roles as local / regional commissioner. Where public health staff are spending a substantial part of their working life in an out-posted environment arrangements should be in place to ensure they are adequately supported and that there is clarity of roles and responsibility. Such staff should be professionally accountable to the regional director of public health and their job plans should secure adequate time for professional development and CPD. Any difficulties arising from the capacity agreed or any necessary change will need to be agreed at a senior level between the two organisations in order that individuals are not placed in an invidious position between the two.
Q7. The Department is seeking your views on the proposal to incorporate Health and Social Care Trust specialist health improvement functions into the Regional Public Health Agency.
Response:
The removal of specialist health improvement staff from the Trust may reduce the ability of the Trust to deliver on the health improvement agenda. Trusts need to have public health/health improvement specialist leadership embedded within its services so that health improvement including community development is not peripheral to the trust agenda.
It would be important to develop strong links between the RPHA and Trusts and for staff to be based locally. Fully coordinated health improvement programmes should be secured via the commissioning process, including the sub-commissioning of appropriate services from or through Trusts.
Q8. The Department is seeking your views on the proposal that, in the future, local government could be required, through legislation, to consult with the Regional Public Health Agency when developing its community plans.
Response
We would support strong links, supported by legislation, to ensure that, in the pursuit of health and wellbeing, local government and health and social care organisations are working collaboratively to a common agenda and are fully consulting each other on relevant matters.
We would expect legislation to identify a number of organisations, agencies or sectors with whom local councils will be expected to consult when preparing community plans. The RPHA would be one of those organisations. We would expect also that the RHSCB, and especially LCGs, would be actively involved in community planning.
Q9. The Department is seeking your views on the proposal that the Regional Health & Social Care Board and its Local Commissioning Groups would be required, through legislation, to seek advice from the Regional Public Health Agency when developing their commissioning plans.
Response:
To ensure that the RHSCB can deliver to commissioning for improved health and wellbeing requires public health needs to be embedded in the commissioning process. Legislation to seek advice will not in itself deliver this. Moreover, given that the RHSCB and the RPHA will both be part of the close family of HSC organisations, probably sharing staff and board members, and both being accountable to the Department, it should be axiomatic that they will consult one another without this having to be enshrined in legislation. However, if the relationship is to be underpinned by legislation, then this should require the RHSCB to take due regard of the advice of the RPHA rather than just to consult.
We would be concerned unless the working arrangements between the RHSCB and the RPHA are robustly established early on in the change process that the Board may seek alternative ways of securing public health advice immediately undermining the prime function of the Agency. This risk would be mitigated by the early appointment of the Regional Director of Public Health.
Q10. The Department is seeking your views on the proposal to appoint the Chief Executive or a senior Executive of the Regional Public Health Agency as a non-Executive of the Board of the Regional Health and Social Care Board.
Response:
The document has already referred to a function of the Regional Health and Social Care Board as commissioning from Trusts and other organisations to improve health and wellbeing of the population. This must be undertaken cooperatively with the RPHA.
Careful consideration is required to clarify not just the role of the respective organisations (each with a ‘Board’) but how they interconnect on an ongoing basis to effect sustained improvement in health and well being.
The RHSCB as a commissioner of health and social care must have appropriate professional leadership embedded at executive level. The position of a senior executive of the RPHA as a non-executive of the Board would be important as the formal link, whilst recognising that this individual would then be a member of two Boards which may present conflict of interest and difficult governance issues. This individual should be the Regional Director of Public Health who should have the ‘right to be heard’ enshrined. By the same token, it will be important to ensure that the RHSCB Director of Social Services plays an equivalent role in terms of the Board of the RPHA.
Q11. The Department is seeking your views on the proposal of how to make the work of the Regional Public Health Agency fully multi-professional.
Response:
The RPHA should be multi-professional and multidisciplinary. It should also be able to deliver across the range of programmes of care.
There must be Public Health leadership, a Regional Director of Public Health supporting multidisciplinary public health training and continued professional development. The RPHA should also be able to have formal links with the primary care function. The ability to have a public health input to Directed Enhanced Services should be developed.
The Board’s comments in response to Question 6 regarding social services input to the RPHA are also relevant. Such input may be best achieved by some social services staff, employed by the RHSCB, having agreed contractual commitments to the RPHA. It might be desirable for a senior social services officer to have responsibility for leading this work, in which case they would be contracted for the majority of their time to work in the RPHA.
Q12. The Department is seeking your views on the proposals for the Agencies referred to in Section 8.
Response:
In keeping with the move for a streamlining of Health and Social Care organisations and associated systems and processes we are broadly supportive of the merging of agencies into a common service organisation. It should be noted, however, that the NI Guardian ad Litem Agency and the NI Social Care Council were established to sit outside the main “commissioning and provider organisations” so that they could have a professional “challenge function”. Their incorporation into a common service organisation would question this key role.
They require to be considered alongside the Regulation and Quality Improvement Authority (RQIA), which has a distinct role “outside the Health and Social Care commissioning and provider organisations”. The previous RPA proposal that the NI Regional Medical Physics Agency becomes part of the Belfast HSC Trust is supported. In terms of the proposal to include the functions of the Mental Health Commission within the RQIA, the majority view of the Board is that we are supportive of the proposal. There is not however consensus in this regard, one of the Board’s non-executive directors being strongly in favour of the Mental Health Commission retaining its current status.
We would support the view that the functions currently undertaken by CSA should be incorporated appropriately within the proposed new CSO.
The functions of Health Estates should be reviewed in light of the view expressed above that the appropriate place for capital planning should be within the Regional Board as a core element of commissioning.
Q13. The Department is seeking your views on the proposals for the two options, set out in Section 9, to replace the HSS Councils.
Response:
The new consumer body must be able to influence the new RHSCB and RPHA. It should have both a local population focus (as advocates on behalf of the local population) and also have a regionally coherent influence on the commissioning and the public Health and wellbeing agendas. Its potential to do this would be reduced with an Option 2 model. We would therefore be recommending a single independent regional body with clear local identities and flexibility for managing its agenda and work through committees, groups and dispersed staff. It will be important that in the shaping of the service in future the consumer body’s voice is effectively heard at both regional and local levels – in practice a new organisation which has both a “hub and spokes” in representing patients’ and clients’ interests.
Q14. The Department is seeking your views on the constitution of the new organisation(s) under each of the proposed options, set out in Section 9, to replace the HSS Councils.
Response:
We would be generally supportive of the proposal set out in paragraph 9.6 of the consultation document. However, as local Council representatives are to be members of the newly established Local Commissioning Group (LCG) it may be appropriate to review the input from this Group to the new consumer body and increase membership from the voluntary lay and carers sectors. Furthermore it is suggested that lay representatives on LCGs should come from the replacement consumer body / Health and Social Service Council and should not be a locally elected Councillor. It would be inappropriate for common membership of LCGs and the replacement organisations for Health and Social Services Councils.
It will also be important in influencing decision-making and ensuring that a strong consumer voice is heard. The new consumer body should have the right to attend and participate in meetings of the proposed Regional Health and Social Care Board and the Board of the new Regional Public Health Agency.
Q15. The Department is seeking your views on the human rights implications of the proposals for Health and Social Care reform and any issues you think relevant.
Response:
The main consultation document makes reference to appropriate statutory functions currently carried out by the current Boards becoming functions of the Regional Board. It is important in this regard that the regional Board establishes and maintains appropriate mechanisms to ensure that its statutory equality and human rights duties as set out by Section 75 of the NI Act and the Human Rights Act 1998 are discharged effectively.
Q16. Can you identify any additional relevant evidence or information which the Department should have considered in assessing the equality impacts of these proposals?
Response:
The EQIA undertaken by the Department is rightly presented in the context of the seven necessary steps for such a process. However, the detail of the data and information presented and the level of data analysis undertaken in the consultation document appears more akin to an initial screening exercise than an EQIA.
Limited quantitative information is considered for some of the groups and is considered only in the context of six of the section 75 groups. Other sources of information, for example from OFMDFM (2006), could have been used to estimate the numbers of people who are gay, lesbian or bisexual estimated at 10% or Department of Health and Social Services figures (DHSSPS 2000) which estimates that 34% of the working population have caring responsibilities.
There also appears to have been no attempt within the EQIA to consider qualitative information collated through pro active consultation and engagement with staff or section 75 groups using a variety of methods. It may have been useful to consider other sources of information to inform the EQIA where quantitative information is limited. As reported in the Guidance on EQIAs produced by the Equality Commission 2004 “ it is unacceptable for an EQIA to merely record that no data is available”. Where local data is not available the advice is to consider comparative data from elsewhere. Other EQIAs from other organisations often provide useful material such is the EQIA undertaken by the Inland Revenue which examined reorganisation.
Reference is made to the Shared services EQIA (2007) and the Human Resources Framework EQIA (2006) as sources of evidence to be used. Both of these documents were high level EQIAs. Feedback given from a range of sources highlighted that these previous exercises were also limited in the information, data and analysis they contained. The expectation would therefore have been that such feedback would have positively influenced the current EQIA exercise more than seems to have been the case. It is also unclear if and how the ministerial visits and engagement with staff have been used to inform the EQIA process.
Q17. Can you identify any other potential adverse impacts, with supporting evidence, which might occur as a result of these proposals being implemented?
As acknowledged throughout the EQIA, the proposals will inevitably have a material impact on administrative and managerial staff in Boards, Agencies, Trusts and the Department. The focus on staff within the EQIA is therefore appropriate and welcome.
One of the difficulties is that the EQIA concentrates on things that will “potentially” happen in respect of location, recruitment and redundancies as decisions have yet to be made on the number of staff who will have to relocate or the number of post reductions that would have to be delivered. Given the complexity and differences across the organisations affected however the impact of the proposals could vary significantly between organisations.
For example, the proposals envisage a reduction in posts within Boards from the current total of approximately 900 staff. At the same time, the estimates number in the new Regional Board is put at around 400. These comparative figures may have a disproportionate adverse impact on current employees of Boards. These comparative figures stand in contrast to other comparative figures featured in the current proposals. In particular, the size of the proposed Common Services Organisation at over 2000 staff, appears less likely to have an adverse impact on current employees of other organisations, for example, when seen in relation to the current size of the Central Services Agency at approximately 600 staff. In addition, it is possible that there may be further differential impacts on current staff numbers as a result of the establishment of a Regional Public Health Agency.
Q18. Can you suggest any other mitigating measures to eliminate or minimise any potential adverse impact on the staff concerned?
Response
The mitigating measures suggested are quite general.
Q19. Have the needs of the Section 75 categories of people been fully considered in this EQIA? If not, please provide details and supporting evidence.
Response
In a number of these groups it is suggested that no evidence exists to indicate differential or adverse impacts. Without the collation of additional data for a number of these groups and analysis of this data to inform the EQIA, it is difficult to see how such conclusions can be reached with confidence. In addition, little consideration is given within the EQIA to the need for monitoring data which is a key element of the EQIA process.
Whilst the EQIA rightly acknowledges the potential impacts on staff groups in affected organisations little attention is given to other affected groups, including Section 75 Groups and service users.
The expressed objective of the proposals are to “improve health and social care services and thereby the well being of the people in N.Ireland.” However, there is insufficient attention in the EQIA to consideration of the impacts on service users and ways in which to ensure adequate public involvement in consideration of critical issues, including what services should / should not be commissioned and which services are best commissioned locally versus regionally.
Q20. Do the proposals afford an opportunity to promote equality of opportunity and/or good relations?
Response:
In this regard, it will be important to ensure that equality and human rights issues receive appropriate attention in the context of preparatory work being undertaken by the work streams referred to in the main consultation document and throughout the period of transition. It will also be important to ensure that democratically elected local representatives participating in the new arrangements are encouraged to champion the views of all Section 75 groups.
General Comments
Response:
Page 15 of the main consultation document lists a number of cardinal principles in terms of the constitution of the proposed Regional Board. The key principle of equality should be added to the list.
Belfast City Council
This response to the Health and Social Care (Reform) Bill is written in the context of Belfast City Council’s recent comprehensive response to the consultation on proposals for health and social care reform. While the Council recognises that those proposals go beyond the issues which need to be enshrined in legislation, we would ask that our wider comments on the proposals be considered in the implementation of the health and social care reforms.
The Council welcomes the Health and Social Care (Reform) Bill and, in particular, is supportive of the creation of the Regional Agency for Public Health and Social Well-being. There are a number of matters within the Bill which we believe require further consideration to ensure that the opportunity is maximised to put in place legislation which will improve health and well-being.
The Council is concerned that increased democratic accountability could be limited in that elected representatives will not be on the Regional Health and Social Care Board.
Section 8 includes the requirement for the Board to consult the Regional Agency for Public Health and Social Well-being (RAPHSW) in drawing up the commissioning plan. We consider that, in addition to this, integration would be improved by the inclusion of the chief officer or Chair of the RAPHSW as a member of the Board.
Section 13 describes the proposed functions of the RAPHSW, including the need to co-operate with other bodies which exercise functions relating to health improvement or health protection. The Council believes that this should be more clearly articulated in relation to working with local government and would ask for the inclusion of a reference to the need for two way formal statutory consultation between local government and the Regional Agency and local commissioning groups, when developing commissioning plans and community plans. Given the significance of the local government role in the delivery of public health functions we would ask for a requirement in the legislation for the Agency to work in support of local government. The Council considers that the requirement for the RAPHSW to provide the Department, the Regional Board and Local Commissioning Groups with such information, advice and assistance as they may reasonably require in connection with the exercise of their functions, should be extended to include local councils in the exercise of functions relating to health improvement and health protection.
At 7.4 of the earlier consultation, the expectation of the Agency having both a regional and a strong local presence is stated. In the Council’s response it was suggested that the RAPHSW should have locally based inter-disciplinary teams for health improvement that could work along side the Local Commissioning Groups to develop local health improvement plans that balance regional priorities with local need. It is not clear, from the draft Bill, how the inter disciplinary or strong local presence of the Agency will be achieved.
The Council considers that the Local Commissioning Groups should be aligned with the new local government structures to facilitate effective representation mechanisms and allow joint working on a regular basis.”
Southern Area Children and
Young People’s Committee
1. Introduction.
The Southern Area Children and Young People’s Committee (SACYPC) is the multi-agency and multi-sectoral partnership which oversees the Children’s Services Planning process in the Southern Health and Social Services Board area.
Children’s Services Planning, mandated by the Children’s Services Planning Order 1998, and led by each Health and Social Services Board, draws together statutory, voluntary and community organisations to carry out joint strategic planning to address the rights and needs of vulnerable children and young people.
The overall aim of the Southern Area Children’s Services Planning process is to enable vulnerable children and young people to reach their full potential and be socially included members of the community, as children and adults. The process has now been adapted to ensure that its planning is driven by the need to contribute towards improvement in children’s outcomes, as set out in the OFMDFM Ten Year Strategy ‘ Our Children and Young People: Our Pledge’.
Each Children and Young People’s Committee (CYPC) carries out its planning through the processes below to achieve the above aim, as follows;-
- An outcomes approach to addressing the rights and needs of children and young people
- Seeing children and young people in the round
- Providing support to families
- Setting up locality inter-agency processes to improve outcomes for children as articulated by their communities as well as local agencies
- Incorporating children into the planning process so that their view are heard and listened to.
Each CYPC leads a number of planning or working groups, which plan for specific groups of children and young people who are likely to suffer social exclusion.
2. Response to the Health and Social Care (Reform) Bill.
The Southern Area Children and Young People’s Committee (SACYPC) welcomes this opportunity to respond to the Committee’s consultation on the Bill. The SACYPC also welcomes the statement made by the Minister to the effect that Children’s Services Planning will transfer from the HSS Boards to the new Regional Health and Social Care Board. We trust that the transfer of statutory responsibility for Children’s Services Planning is dealt with through Section 8: Functions of the Regional Board and Section 24: Transfer of Functions of Health and Social Services Boards.
The current statutory responsibility for Children’s Services Planning requires the four Health and Social Services Boards to produce Children’s Services Plans under the Children (NI) Order (Amendment) (Children’s Services Planning) Order (Northern Ireland) 1998.
The SACYPC believes that the current reform presents a critical opportunity to improve these arrangements and to create a process through which accountability can be discharged effectively, which cannot be achieved by any single agency in isolation.
It is also our view that action must be taken to ensure that adequate provisions are built into the legislation to provide the required accountability for the delivery of statutory responsibility for planning and commissioning of children’s services.
We suggest that the four Area Children and Young People’s Committees proposals for ‘A Joint Planning and Commissioning Framework to Improve Outcomes for Children and Young People’[1](attached at Appendix A) should be taken into account in the final draft of the Bill. These proposals provide for the expansion and further development of statutory Children’s Services Planning. We suggest that these proposals fully address the deficiencies of agencies currently planning and commissioning services separately, and should be taken forward as the way ahead for the future planning and commissioning of children and young people’s services.
We have appended these proposals to this response. The SACYPC would strongly advocate that these proposals are taken forward into account in the final version of the Bill, thereby ensuring a positive way ahead for the future planning and commissioning of children and young people’s services.
Children’s Rights Framework
The Committee recommends that statutory provision for Children’s Services Planning must be firmly grounded in the children’s rights framework which the Department of Health, Social Services and Public Safety signed up to through the cross government 10 Year Children and Young People’s Strategy. The legislation should integrate the over-arching guiding principles of the United Nations Convention on the Rights of the Child (UNCRC) and inform and guide the Department’s delivery of the strategic outcomes of the 10 Year Strategy.
Ultimately, reflecting on the Minister’s guiding principles for reform, statutory Children’s Services Planning must be child-centred and responsive to the rights and needs of all children and young people, promoting their best interests (UNCRC Article 3) in a non-discriminatory manner (UNCRC article 2). Fundamentally and again reflecting the Minister’s guiding principles for reform, children and young people must be given the opportunity to be heard and have their views given due weight and consideration (UNCRC article 12) at all levels in the planning and commissioning of children’s services.
Currently Children’s Services Planning does enable the involvement and active participation of children and young people at local level, however under the new arrangements for Children’s Services Planning in our proposals, participation of children and young people should be a key consideration at all levels, from government through regional to local level.
In this regard the SACYPC would highlight the role and remit of The Participation Network which is supported by OFMDFM[2]. The Participation Network works with Government departments and statutory agencies in Northern Ireland to develop their capacity to fulfil their duties to effectively engage, and involve children and young people in decision making. We have found it useful in increasing participation and believe that this key asset be fully utilised by Government as it takes forward all of the RPA reforms.
Statutory Duty for Integrated Planning and Commissioning.
Our view is that expanded and enhanced provision for Children’s Services Planning within the new arrangements for health and social care must be underpinned by a statutory duty to plan and commissioning children’s services across agency.
We have recognised the absence of this statutory duty as a limitation within the current Children’s Services Planning process where, despite much good practice in multi-agency planning at locality level, the process has been reliant on goodwill in the absence of a requirement for agencies to co-operate and draw up joint plans.
We therefore propose that expanded and enhanced provision for Children’s Services Planning within the new arrangements for health and social care should be underpinned by a statutory duty to co-operate to deliver the Ten Year Children and Young People’s Strategy. The statutory duty should be initiated at Ministerial level underpinning the functioning of the Ministerial Sub-Committee on Children and Young People, and should operate at departmental, regional and local levels facilitating and enabling the joint planning and commissioning of services for children to meet the outcomes of the Ten Year Strategy.
Role of the Voluntary and Community Sector
The SACYPC is concerned at the limited recognition of the role of the voluntary and community sector both as a provider of services and as an advocate for communities.
The SACYPC recommends that the role of the children’s voluntary and community sector is explicitly recognised within the statutory duty to plan and commission services together, thereby ensuring the sector’s existing central role is maintained and protected within future arrangements for Children’s Services Planning. We would also recommend that there is recognition of the voluntary and community sector as a key partner in the initiation, maintenance and facilitation of the planning process. In other jurisdictions similar recognition of ‘other persons or bodies’ who ‘exercise functions or are engaged in activities in relation to children’ has been included in legislation.[3]
Consideration of the Same Issue by the Committee of the Office of the First Minister and Deputy First Minister.
We would further suggest that the Committee have regard to Final Report on the Committee of the Office of the First Minister and Deputy First Minister’s Inquiry into Child Poverty in Northern Ireland. This Committee commissioned comparative research on the legislation underpinning Children’s Services Planning in Northern Ireland and compared this with approaches in other countries. This Committee recommended that:-
‘OFMDFM and relevant departments and agencies, including, in particular, the Department of Health, Social Services and Public Safety and the Department of Education, review and update legislation underpinning Children’s Services Planning with a view to:
- Extending the duty to develop children and young people’s plans to at least include the Regional Health and Education Authorities;
- Linking the Children’s Services Plans more directly with the outcomes of the Children’s Strategy, whilst retaining specific recognition in the legislation for children in need;
- Strengthen the legislation, or statutory guidance, so that relevant organisations are required to co-operate, rather than participate, in Children’s Services Planning and delivery.’
The above recommendations are completely consistent with the proposals of the four Children and Young People’s Committees proposals, which are attached at Appendix A.
Appendix A
Implementing ‘Our Children and Young People – Our Pledge’:
A Joint Planning and Commissioning Framework to Improve Outcomes for Children and Young People.
February 2007
(Diagram updated March 2008)
Implementing ‘Our Children and Young People – Our Pledge’:
A Joint Planning and Commissioning Framework to improve Outcomes for Children and Young People.
Key Messages.
1. The paper proposes joint planning arrangements for the implementation of Our Children and Young People Our Pledge: a Strategy for Children and Young People in Northern Ireland.
2. The proposals are aimed at
a. Replacing the existing system for inter-agency planning and commissioning of services for children and young people, and
b. Addressing the deficiencies within the present system.
3. There can be no straight read-across, due to differences in how services are delivered, but the proposals mirror Every Child Matters arrangements in England and the integrated children’s services approach being adopted in Scotland. In Northern Ireland it is essential that there is a strategic partnership at regional level as the key mechanism for achieving integrated services for children and young people.
4. The proposals would set in place statutory duties for co-ordinated planning for all children, without detracting from individual Department and Agency accountability arrangements.
3. Introduction
Thank you for inviting us to share with you our proposals for a joint planning and commissioning framework to improve the outcomes for children and young people contained within Our Children and Young People: Our Pledge’.
4. Current Arrangements
We represent the four Children and Young People’s Committees (CYPCs), the multi-agency and multi-sectoral partnerships which oversee the Children’s Services Planning process. This process was set up in 1998 and the Children and Young People’s Committees have evolved into strong multi-sectoral partnerships, drawing together Statutory, Voluntary, Community and Black and Minority Ethnic organisations to carry out joint strategic planning to address the rights and needs of vulnerable children and young people. Our third three-year multi-agency Children’s Services Plans were based on common themes agreed across all four Committees, and the Committees have now agreed that the next Children’s Services Plan will address planning at a Northern Ireland level as well as local and locality levels.
Our learning process, through carrying out joint planning, has led us in the same direction as Every Child Matters and the Children Act 2004 in England, and similar changes in Scotland and Wales.
We have been able to set up some innovative jointly led and commissioned services. We have provided much needed learning and practice regarding joint planning, especially at locality level. However, despite our efforts, most mainstream services for children and young people still remain firmly in their separate silos of ‘health’, ‘social services’ ‘education’ etc. The 3 major deficits in the current process are:-
1. Though there is a statutory duty for Health and Social Services Boards to lead the process, there has not been a duty to co-operate for other agencies, so the process relies on goodwill.
2. The requirement for co-ordinated planning has not operated at Government level.
3. The Children’s Services Planning process has addressed vulnerable children in isolation from planning for all children. It has been difficult to influence universal services to better support vulnerable children and therefore it has been difficult to promote preventative strategies.
In formulating our proposals for improving the better integration of services for children, we have welcomed two key Governmental drivers for change in Northern Ireland – the Strategy for Children and Young People and the Review of Public Administration proposals.
We had learnt, as had been learnt in other parts of the UK – that planning for vulnerable children and young people cannot be successful if it is not connected to planning for universal services. We developed the Northern Ireland Family Support Model – based on the work of Pauline Hardiker –which provides a framework for analysis of services from prevention and early intervention through to specialist services. This is completely in keeping with the thinking of Every Child Matters.
‘Our Children and Young People: Our Pledge : the Strategy for Children and Young People in Northern Ireland’ is the core part of the solution as it has introduced the central driver of universally accepted outcomes for all children and young people. This has not only introduced a common language but also introduces the need for all services for children to be able to demonstrate their contribution to achieving these outcomes.
The Review of Public Administration could be the second building block. The RPA could, if managed effectively, allow services for children and young people to be planned and commissioned to achieve the outcomes set out in the strategy. The RPA presents the chance to do, in Northern Ireland, what the Children Act 2004 is doing in England – to make services for children and young people fit around the child, as opposed to the child and family trying to fit themselves to disparate and disconnected services – with statutory duties for integrated planning and clear accountability for such joint work between government and local agencies.
Joint Planning and Commissioning of Children’s Services, Post RPA
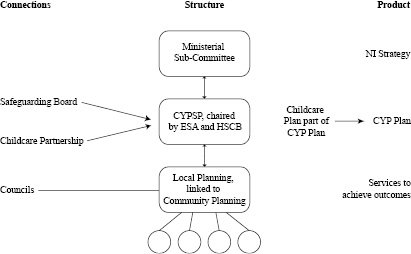
3. Proposals.
3a. Government Level
We would now like to offer our understanding of what has been set out within the Strategy for arrangements at Government level and our vision of how regional and local planning and commissioning could provide the implementation process for the Strategy. Clearly, at Government level, the Ministerial Sub Committee on Children and Young People will be leading the overarching Strategy for Children and Young People. Our view is that the Committee should put in place requirements on all Departments of Government to work towards the Strategy outcomes, which the Committee should monitor through a performance management framework which measures Departments’ contribution to the delivery of such jointly agreed outcomes.
At Ministerial and Departmental level we think that the process should ensure a consistent policy direction across Departments, based around each Department’s contribution to achieving the outcomes. Key service priorities, e.g. the educational needs of Looked After Children, or the reduction in teenage pregnancies should be ‘joint governmental priorities’ within the Strategy as well as being included in all the relevant Departmental priorities. Performance measures should also be consistent and linked to the high level outcomes.
Accountability for individual Departmental policies clearly remain with the relevant Ministers and Departments concerned but there should be the additional line of accountability to the Ministerial Sub-Committee to ensure consistency across Departments in setting the Governmental priorities, targets and performance measures.
3b. Regional Level
At the next level we believe that there should be a regional Children and Young People’s Strategic Partnership. Its purpose would be to implement the Strategy by putting in place a Children and Young People’s Plan. This would be a single, strategic, overarching plan on how all agencies will work together towards achieving the outcomes for all children and young people. It would support more integrated and effective services to secure the outcomes set out in the Strategy.
The Plan would provide a common overall direction for the development of all services to children, across agencies and sectors, to improve the high level outcomes for children. In addition it would set out specific plans for groups of children who are achieving poor outcomes, and would address the joint governmental priorities set out in the Strategy.
This body should be led jointly by the Education Skills Authority and the proposed regional Health and Social Care Board. Its members should either be CEO’s or CEO direct appointees, and should represent Health and Social Services, Education (including after school age learning), Statutory agencies concerned with Youth Justice, Housing, Social Security etc, as well as the Community and Voluntary (including Black and Minority Ethnic) sectors.
There should be a statutory requirement on all agencies to take responsibility for such integrated planning, through a single Children and Young People’s Plan, as there is in England for such Plans.[4] This Plan would cover all services for children and young people, from universal to specialist, and include Early Years, services associated with Education and Schools, Safeguarding, Youth Justice, Social Services for Children in Need and all services for disabled children and young people.
The Children and Young People’s Plan will need to link to the separate plans which the partner agencies will continue to draw up to cover the full range of services and statutory duties for which they are responsible, and single agency plans would reflect the priorities and actions agreed through the Children and Young People’s Plan which link to the Strategy outcomes.
The Children and Young People’s Plan could therefore replace a large number of existing plans. In England such Children and Young People’s Plans have replaced 7 statutory plans and 12 non-statutory plans, and link to many more.[5]
The inclusion of both universal and specialist services in a Children and Young People’s Plan is an extension of the current Children’s Services Plans – these currently only cover vulnerable children and children in need.
We feel this shift is essential, for two reasons:-
Firstly, the outcomes approach, as set out in the Strategy, emphasises inclusion and the need to ensure that those children who are most vulnerable have the same opportunities as other children.
Secondly, early intervention and prevention requires a refocusing of universal services to respond more effectively to those children who are struggling to achieve reasonable outcomes.
So, all services to children, both universal and specialist, should be planned in a coherent ‘joined up’ manner.
In order to ensure this appropriate linkage between universal and specialist services, the Strategic Partnership will need to be integrated with other key fora such as the regional Safeguarding Board for Northern Ireland. Whilst such fora will have responsibilities in their own right it is essential that these are set out in such a way as to ensure synergy with the work of the Strategic Partnership. In addition, it is essential that these fora relate to the same body, in order to avoid conflicting requirements.
Taking the need for safeguarding children as an example, the role of the Northern Ireland Safeguarding Boards is not to plan services for all six outcomes – but to ensure that the safety aspects relating to all six outcomes are being delivered through the wider planning process of the Children and Young People’s Plan.
Prevention and early intervention in relation to safeguarding is provided through services such as early years, parenting programmes, primary healthcare, educational support services and local community support services. The joint planning and development of these services would be carried out through Children and Young People’s Planning.
Why should the partnership be regional?
Children and Young People’s Strategic Partnerships in England are led by Local Authorities. We considered whether this process should be driven at the local council level here in Northern Ireland. There are a number of critical reasons why we think this is not possible, as follows;-
Co-terminosity has not been achieved by the RPA process. Heath and Social Services are delivered through 5 Trusts, which are not co-terminous with the suggested council areas.
District councils in Northern Ireland do not have responsibility for education, children’s health or social services. Therefore, there cannot be a direct read-across from other UK arrangements for the integrated planning of services for children and young people. In particular, financial and statutory responsibility for services for children is not vested in a single body such as a Local Authority.
Agencies who are organised regionally, including PSNI, PBNI, Youth Justice Agency, NI Housing Executive and Social Security Agency, have been telling us that relating to 4 CYPCs is difficult and that one planning process, informed by local needs assessment, is what is required. A number of regional childcare voluntary agencies have been saying the same.
There will be a regional Safeguarding Board to replace the four existing Area Child Protection Committees, which are currently led by Health and Social Services Boards. It follows from this that the process of developing a Children and Young People’s Plan in the Northern Ireland context should be at regional level.
Developments in England and Scotland are moving towards the pooling of budgets to improve the integration of services for children and young people. Experience nationally and internationally suggests that this is ultimately required. It is unlikely that budgets for services for children will be devolved to local (council area) level. Therefore the co-ordination of planning and commissioning needs to be carried out at the level at which major decisions about budgets are made.
For all these reasons we suggest that the Children and Young People’s Strategic Partnership should sit at regional level. In addition, we recommend that this body is jointly chaired by the Education and Skills Authority and the proposed regional Health and Social Care Board. Given that the equivalent bodies in England are chaired through Children’s Trusts or Children’s Departments, both of which combine education and children’s social services, we think that this joint chairing arrangement suits the arrangement of agencies within Northern Ireland.
3c.Local Level
At local level, the RPA has set in place the requirement for the co-ordination of planning and delivery of services through the concept of community planning, led by local councils. However, councils will not currently assume responsibility for children’s Health, Social Services, or Education services. This differs from the Scottish model, which has been used in the RPA consultation document as the model for the proposals in community planning.
It is our view that the co-ordinated planning of children’s services, as part of community planning, would struggle for effectiveness at this time when being led by agencies with little responsibility for children’s services. It is also crucial that the local processes for assessment of need and delivery of services link into the Regional Children and Young People’s Strategic Partnership. Therefore it is our view that it would be most appropriate that the local level of planning for children’s services should be a multi-agency process which operationalises the regional Children and Young People’s Plan to meet locally assessed need. This two level process (regional and local) could then result in the chapter on planning for children in the local Community Plan. It is important that delivery resulting from such planning at local and regional levels is equitable and needs led.
This approach would mirror that taken in England to link the Children and Young People’s Plan and Local Area Agreements (the equivalent of community planning in England). The Guidance on Local Area Agreements[6] states that the Children and Young People’s part of each Local Area Agreement should reflect the Every Child Matters outcomes and the Children and Young People’s Plan.
4. Summary.
We have given a brief outline of an approach that we think could be taken to integrate the planning of services for children and young people to implement the Strategy.
Whilst the proposals have been developed from our experience of existing multi-agency structures, their success will require a number of key changes.
Legal requirements.
In addition to the structures and processes outlined above, it is our view is that there should be a legal requirement for a regional Children and Young People’s Plan – with legal requirements on all participating agencies to plan together the services needed to achieve jointly agreed outcomes for children, and for the plans of individual agencies to reflect that Plan. This would radically improve on current arrangements.
Therefore, in detail, there should be:
A joint duty on the both the Education and Skills Authority and the proposed regional Health and Social Care Board to initiate, maintain and facilitate a planning process, recorded in Children and Young People’s Plans.
A duty on named key public bodies to participate in the creation and implementation of the Children and Young People’s Plan.
A duty on Northern Ireland or Direct Rule Ministers to promote and encourage Children and Young People’s Planning as the key over-arching framework to improve the planning and provision of services for children and young people.
It needs the participation of children and young people at all levels
We are enabling involvement and active participation of children and young people at local level through Children’s Services Planning processes. It is our view that this must remain a central consideration in taking forward the wider RPA reforms, and must mirror the mechanisms in place between the Government, Regional and local levels, with children and young people participating at all levels, recognising that already existing mechanisms for the participation of children should not be duplicated.
Outcomes promoting rights and needs.
We have incorporated the promotion of children’s rights through the Children’s Services Planning process. Flowing from the rights outcome within the Strategy, we think that the Children and Young People’s Plan should incorporate the promotion of children’s rights throughout its planning and performance management frameworks.
With Democratic Accountability at all Levels
We think that the Children and Young People’s Strategic Partnership should include representation across the Statutory, Voluntary, Community and Black and Minority Ethnic sectors, with participation of children and young people. Democratic accountability should be led out through the Ministerial Sub-Committee, and mirrored at regional and local levels as appropriate. We believe that all organisations should address these requirements as they restructure following RPA.
This must be adequately resourced -
This process must be adequately resourced. The planning structures need to include planning, financial and professional expertise. In addition, best practice in the participation of children and young people demonstrates that resources are required for participation to be effective.
[1] CYPCs, ‘A Joint Planning and Commissioning Framework to Improve Outcomes for Children and Young People’, p.4
[2]2 http://www.ci-ni.org/theparticipationnetwork/
[3] Children Act 2004 http://www.opsi.gov.uk/acts/acts2004/ukpga_20040031_en_3#pt2-pb1-l1g10
[4] Statutory Guidance on Children and Young People’s Plans for England due out in February 2007. Currently non-statutory guidance is in place.
[5] p.6 Guidance on Children and Young People’s Plan, London,2005.
[6] Local Area Agreements Guidance. Office of the Deputy Prime Minister, London, June 2005.
Mental Health Commission
I refer to your recent correspondence seeking comment from the Mental Health Commission on the Health and Social Care Reform Bill.
The Commission would make several general comments.
One of the major strengths of the HPSS within Northern Ireland is its integrated structure which has been the case at senior levels within the Boards for more than 35 years and is now reflected within the Trust management and operational delivery structures. The proposal to now create two separate bodies (i.e. a Regional Public Health Agency and a Regional Commissioning Board) has significant potential to disrupt this integration. We can see no good reason why this proposal for separation is being made. If separate divisions are necessary to ensure that different interests are served, then so be it but this can surely be achieved while maintaining staff within a single corporate entity, single senior management leadership and single point accountability. This approach would obviate the need for legislation to underpin what is the current reality of multidisciplinary working within commissioning bodies. It is this approach that we believe has led to very significant reform and modernisation, and progressive achievement, particularly over the last ten years in mental health and learning disability services.
The proposal to move from seven LCGs to five is welcomed as it will allow for synchronicity and co-terminosity with HPSS Trusts while still accommodating close links with local councils. However, we can see real frustration amongst General Practitioners who are not convinced that significant commissioning autonomy will be devolved to a local level. Unless they and their primary care colleagues are intrinsically involved in this process, we risk losing the benefits that have been obtained in recent years, for example in the further development of home treatment, the stepped care model and primary care fronting service delivery in areas such as
Child and Adolescent Mental health services and services for people with an eating disorder.
At the same time, we wish to see a strong regional commissioning focus for those aspects of planning, commissioning and performance management that need to be led on a regional basis. We would welcome the development of a single body responsible for commissioning services that we could engage with on a regular basis and draw attention to some of the major weaknesses that we identify regularly.
We would strongly advocate that professional leadership is embodied within the organisation responsible for strategic planning, commissioning, financial and performance management. We are convinced that the world class commissioning being sought is best achieved through the bringing together of technical corporate skills along with professional expertise and experience.
The problems associated with the split between the Regional Board and the RAPHSW are now exacerbated because of the Bill’s proposals to place elected representatives on the Board of the RAPHSW rather than the Board of the Regional Board i.e. the Councillors will also be at arms length from commissioning decisions.
Article 4 allows the Department to take decisions without consultation and this represents too much power with no accountability (a similar provision exists for the Regional Board but this at least is subject to Departmental approval.)
It remains to be seen what the effect of Article 8(3) will be. What if the regional board consults RAPHSW, has due regard to their advice and does the complete opposite? Will RAPHSW attempt to exercise control over the Regional Board through the Department? The only real solution will be for there to be such close working between officers of the two bodies that the “join” will be almost invisible.
Schedule 2, Article 7(3) is wrongly drafted and unless corrected, would result in a situation in which RAPHSW committees would have to comprise exclusively of Regional Board members – it is simply a cut and paste error from the previous section – the words “Regional Board” should be replaced by “RAPHSW Board”.
Western Health and
Social Services Board
Thank you for the opportunity to submit comments on the Health and Social Care (Reform) Bill.
We fully accept that there is a need to reform and streamline the health and personal social services organisational arrangements in Northern Ireland. Generally, we welcome the proposal set out in the consultation document which was issued by the Minister for Health and Personal Social Services and Public Safety on 18 February 2008. We enclose a copy of the Board’s response to that consultation document for ease of reference.
We are of the view that the provisions of the Health and Social Care (Reform) Bill reflects the proposals set out in the consultation paper and would provide the basis for ensuring that there is appropriate legislative arrangements in place to support the reform of the health and social care system.
There is a need to ensure that in designing the system for the future, it is fit for purpose, is coherent and delivers high quality outcomes, and that the organisational arrangements are efficient and effective.
We would make the following specific points in relation to the Health and Social Care (Reform) Bill:
- Page 5, Regulation 7(1), page 9 , Regulation 14(1) and page 10, Regulation 16(1) – In these provisions of the Bill it is stated that each of the RHSCB, RAPHSW, RSSO and PCC shall be corporate bodies. These corporate bodies must form part of an integrated system.
- Consequently, there needs to be clear lines of governance and accountability within and between the constituent parts of the reformed health and social care system.
- We contend that it would be important that there is a clear line of accountability through which the Minister would be responsible to the Assembly, the Department responsible to the Minister, and the RAPHSW, the RHSCB and the RSSO responsible to DHSSPS. We would stress the importance of the Trusts being responsible for all performance issues (including financial performance) to the RHSCB. We would contend that this line of accountability needs to be clearly stated in the Reform Bill.
- Clarity of roles and responsibilities would be essential in order to have a health and social care system which is cohesive. Consequently, there is a need for clarity between the commissioning responsibilities of the RHSCB and the RAPHSW. The primacy for commissioning should be the RHSCB. Due regard needs to be given to the views and expertise of those working in the RAPHSW. Reference is made to the respective roles and responsibilities of the new constituent parts of the reformed health and social care system. However, we would hold the view that greater clarity is needed in terms of which part of the system has primacy for commissioning.
- The RHSCB and the RAPHSW will have discreet but complimentary roles in terms of a range of functions, including needs assessment, priority setting and developing a commissioning framework for delivering on targets set out within the Programme for Government and Priorities for Action. There needs to be clarity in the legislative framework in terms of who holds responsibility for issues such as the commissioning plan, the financial allocations etc. The RHSCB must have primacy in terms of the commissioning plan and the allocation of resources within policy frameworks established by DHSSPS.
- We support the proposal that there needs to be political representation on the Local Commissioning Groups, and that that representation should be obtained from local councillors. We would contend however, that there is a need for clarity in terms of:
- The avoidance of dual mandates;
- The number of Councillors required on the LCGs to take account of the number of Councils that will exist post RPA; and
- The need to ensure there is no duplication of roles and responsibilities for Councillors in terms of (for example) membership of the LCGs and the PCC.
Q1 The Department is seeking your views on the functions, constitution and governance proposals for the new Regional Health and Social Care Board.
Response:
It is imperative that there is clarity of roles, responsibilities and governance arrangements throughout the new HSC system.
In that context, we would offer the following views:
- We are of the view that the functions described in para 4.4 of the consultation paper are appropriate for the Regional Health and Social Care Board. We are also of the view that core Family Practitioner Services (including professional and development staff) should be part of the RHSCB. This is developed in more detail in our response to Question 5.
- It is vitally important to have clarity about what is commissioned at regional and local level. We have developed this further in our response to Question 2. Our view in terms of regional commissioning is that there should be one policy, one strategic framework and progressively, one service framework for each programme of care or major area of work. Within that context, the Regional Board should commission those services which are clearly Northern Ireland wide and generally described as low volume, high cost areas. The default position must be that as much commissioning as possible should be done at LCG level.
- The RHSCB should take on responsibility for commissioning high cost low volume services, including commissioning of specialist medicines. This would give the opportunity to establish a Northern Ireland Drug and Therapeutic Committee. This, in turn, would require someone with Pharmaceutical expertise to lead on procurement arrangements within the CSO. The Lead within the RHSCB could also provide input to the RPHA and the CSO.
- In terms of constitution of the Regional Board we support, in general terms, the proposals set out in para 4.3 (page 15) of the consultation document. We make the following additional points:
- We note the proposal that the Chief Executive or a senior level Executive in the proposed RPHA would be a Non Executive Director on the RHSCB. There is merit in this, given the importance of maintaining strong connections between the public health agenda and the commissioning agenda. Whilst the representative of the CSO would not be a member of the RHSCB, we recommend that a Senior Executive of the CSO would attend RHSCB meetings as appropriate.
- With regard to the other Non Executive Director positions on the RHSCB, it is important that the Chairs of the LCGs are Non Executive Directors of the RHSCB. This offers a forum for ensuring coherency and consistency in terms of commissioning at regional and local levels across Northern Ireland.
- We support the view that the Regional Board should also include “such other officers as may be prescribed, having regard to principles of good governance”. In that regard, we contend that the Executive Directors of the RHSCB should also be on the Board of that organisation.
- We also hold the view that the Board of the RHSCB should also include individuals who hold a portfolio for Medical, Nursing and Social Services. Given the scale of Family Practitioner Services functions and budgets we are of the view that there is a need for a lead person at RHSCB for FPS issues, including contract negotiations and management.
- The Board should also include lay representation appointed through the public appointments system, but lay people should not include politicians or local Councillors
- Consideration should also be given to including at least one representative from the Public Service Commission on the Board
Clearly, there is a balance to be struck between ensuring that all key stakeholders are represented on the Board whilst, at the same time, keeping the Board membership to manageable numbers.
- We support the governance arrangements for the RHSCB as outlined in paras 4.6, 4.7 and 4.8 (pages 21 and 22) of the consultation document. In particular, we support the view that there needs to be clarity of roles, functions and responsibilities between the DHSSPS and the RHSCB. We also support the view that the six Health and Social Care Trusts would report directly to the new RHSCB regarding commissioning issues.
Q2 The Department is seeking your views on the functions, constitution and governance proposals for the Local Commissioning Groups, including membership.
Response:
As stated earlier, it is very important at the outset to put in place arrangements that ensure LCGs commission most services, especially those which relate to primary and community care. LCGs must also have a pivotal role in ensuring that services across the HSC and the wider mixed economy of care are reformed and realigned in the context of the strategic and service frameworks set by the RHSCB.
All budgets should be devolved to LCGs on a weighted capitation basis. LCGs should then, within the Board of the RHSCB, agree the proportion of funding which should be devoted to the regional commissioning agenda.
The functions of the LCGs would then flow from that extensive commissioning agenda, and would involve needs assessment, planning, service specification and working with the Service Delivery Unit within the RHSCB structure to ensure that Trusts and other providers deliver on the targets and outcomes.
We will deal specifically with staffing issues later in this submission. However, at the outset we would point out that in order for each LCG to do its work effectively, it will require a strong local presence of staff with technical skills in areas such as: information; strategic planning; performance management; procurement; financial controls; monitoring and regulation. We concur with the view outlined in the paper that these staff will also have a role in contributing to work at regional level. It will also be vitally important to ensure that staff out-posted to support LCGs, staff from the RPHA and the CSO must be co-located in order to ensure complementarity of roles and to ensure maximum synergy.
We support the proposal that there should be five LCGs and these should be co-terminous with HSC Trusts. However, we note the most recent proposal that there will be now 11 Local Councils in Northern Ireland. Further thought will be needed in terms of how the LCGs will link with the appropriate Councils under the auspices of community planning arrangements.
We support the view that LCGs will be Committees of the RHSCB. We also support the view that the RHSCB will have a Scheme of Delegation and a clear operational framework within which LCGs operate. The system cohesion would be assured if the Chairs of the LCGs are members of the Board of the RHSCB.
In general terms, we support the model of membership set out in pages 19 and 20 of the consultation document. We make the following specific points:
Further thought will need to be given to the number of elected local representatives and how they would be drawn from the 11 local Councils to achieve a balance in geography and political constituencies.
There needs to be strong lay representation on LCGs. Involvement of local government on LCGs should not preclude engagement with users, carers and communities.
It will also be important to think through the dynamics arising out of the role and responsibilities of the local elected representatives, particularly the potential conflict of roles in terms of local representatives sitting on Councils, community planning fora, LCGs and other public agencies within the HSC, the HSS Council and the wider public service. Councillors may also be MPs/MLAs and sit on Committees of the Assembly. The issue of dual mandate will need to be addressed in terms of governance arrangements within the new HSC arrangements.
We would contend that the Chairpersons of LCGs should not be drawn from the local elected representatives.
Given the size of the budgets which will be devolved to LCGs, it would be necessary to include a Senior Finance Officer as a member of the LCG to ensure that financial management and budgetary control issues are to the forefront of the work of LCGs.
There should also be a general dental practitioner on each LCG, given the importance that needs to be placed on oral health.
We conclude that the work of the LCG and the geographical area to be covered requires a Commissioning Officer from the RHSCB located locally and dedicated to each of the five LCGs.
Q3 The Department is seeking your views on the process for obtaining local government representation on the Boards of the Local Commissioning Groups.
Response:
As indicated in our response to Question 2 regarding LCGs, this is a vitally important issue.
The balance that is required to ensure that geographical areas and political constituencies are adequately represented on LCGs.
There needs to be clarity in terms of:
- the avoidance of dual mandates;
- the numbers required to take account of the latest proposal to have 11 local Councillors; and
- the need to ensure that there is no duplication of roles and responsibilities for local Councils in terms of (for example) membership of the LCGs and the HSS Council.
Q4 The Department is seeking your views on the functions, staffing and governance proposals for DHSSPS
Response:
The comprehensive list of functions as set out on pages 23 and 24 of the consultation document accurately reflects the central role which DHSSPS must continue to play in the reconstituted HSC system.
We support the proposal to streamline the number of staff in DHSSPS. Further clarification is needed in terms of the number, roles and functions of staff who will transfer to other parts of the reconstituted HSC system. In particular, we are of the view that the information analysis function referred to in para 5.10 of the document should transfer to the CSO.
Clarity is needed in terms of where the HR function lies. Our view is that it is inextricably linked to workforce and commissioning issues, and should, therefore, be located in the RHSCB.
We are supportive of the governance arrangements as set out in the consultation document, with the proviso that an overall governance framework is developed, clearly delineating roles and responsibilities of each part of the new HSC system, based on the principle that there are clear lines of reporting and accountability, and that there is no potential for confusion as to where in the system accountability for core issues clearly rests.
In summary, we hold the view that the core spine of governance and accountability arrangements would be as follows:
The Minister would report to the Executive and the Assembly
- DHSSPS would set the policy legislative and overall financial arrangements for the HSC system
- DHSSPS officials would advise the Minister and the Permanent Secretary would hold the Chief Executive of the RHSCB, the RPHA and the CSO to account.
- The RHSCB would hold the Chief Executives of the six Trusts to account for performance and relevant statutory functions.
Q5 The Department is seeking your views on the additional functions, staffing and governance proposals for the common services organisation.
Response:
We support the proposal to have a Common Services Organisation to provide a range of functions on behalf of the wider HSC system.
We are generally supportive of the range of functions (including additional functions) as set out in para 6.6 and 6.7, on pages 29 and 30 of the consultation document.
The CSO must be seen as an integral part of the wider HSC system, and its staff employed in the CSO would continue to hold HPSS terms and conditions of service.
We make the following specific comments:
- The question has arisen as to where Family Practitioner Services should be located in the new HSC system.
- We have considered a number of options, including locating all FPS functions in either the RHSCB or the CSO, or allocating various functions to the RHSCB, RPHA and the CSO. FPS functions currently carried out by Boards involve a commissioning role and what could be described as “transactional roles” (for example payments to practitioners, probity, management of lists). There are synergies to be gained from keeping FPS staff and functions together. Our view is that the numbers of staff envisaged for the RHSCB should not constrain the future location of FPS functions and staff. We are of the view that all professional and development staff in FPS should be included in the RHSCB, and that staff from the CSA and staff from Boards who currently carry out transactional roles in respect of FPS should be an integral part of the CSO. The RPHA could obtain appropriate advice and inputs from FPS professional staff as and when required. System cohesion would be obtained by having representatives from the CSO and RPHA attending meetings of the RHSCB. The spinal cord of the new HSC system should be the commissioning functions carried out by the RHSCB.
- The question arises as to where the bases for the CSO would be located. We deal with this in more detail in response to question 20. However, it is important within the context of the debate on the CSO, to ensure that we build on the existing skill base such as the work previously carried out by Westcare Business Services (WBS). WBS was established in 1992 to provide common services to the Board and former Trusts in the Western area. WBS provided a broad range of services including Finance, Litigation, ICT, Human Resources, Occupational Health, Management Organisation Development, Social Services Training, Internal Audit, Health Promotion, Estates Services/Facilities Management. The WBS model provided synergy, avoided duplication of effort and provided cost effective outcomes for the client. WBS not only showed the potential for an effective CSO type model but also illustrates the availability of a suitably qualified pool of staff capable of providing CSO functions for Northern Ireland.
- Maximum use of technology should be made to ensure that jobs (including those at senior level) can be dispersed across Northern Ireland.
- In addition care is needed to ensure the proposal to have two main (multi-functional) centres within the CSO – as recommended in the separate consultation paper on Shared Services – is put in place.
- We hold the view that the CSO should be a separate legal entity with a Board structure and clear governance arrangements fulfilling all the functions set out in the consultation document.
Q6 The Department is seeking your views on the proposal to create a Regional Public Health Agency and the functions it would undertake.
Response:
Different views have been expressed by Board staff in terms of the roles, remit and governance arrangements of the Regional Public Health Agency.
More clarity is needed in terms of the roles and functions of the Agency and its interfaces with the RHSCB and CSO.
The RPHA would provide a central role in terms of public health and protection in its widest sense.
The specific points we make in relation to RPHA are:
- The role and remit of the RPHA must be to look at the wider aspects of public health including public health medicine
- The core functions of RPHA would be Public Health covering Health Improvement, Health Protection/Emergency Planning, Screening and Public Health Intelligence
- The RPHA should not directly commission services but provide relevant expertise and advice and the RHSCB would be required by legislation to give due regard to that advice
- The lines of accountability between the DHSSPS, RHSCB, RPHA must be clear and unambiguous
- In addition the RPHA must have a Director of Public Health
- The RPHA would include Public Health Medicine staff, Investing for Health, Community Development and Emergency Planning staff. It would not include specialist Health Promotion staff, HAZ, Health Visitors or other “front line” staff based in Trusts.
In order for the RPHA to function effectively, it will be necessary to;
- specify in legislation that the RHSCB must pay due regard to the expert advice from the RPHA
- put in place clear organisational arrangements to secure input from staff in the RPHA to the work of the RHSCB at regional and LCG levels
- support co-location arrangements to ensure effective integration of staff from RPHA, RHSCB and CSO at operational level
- There needs to be clear lines of communication between the RPHA and any other agencies remaining post RPA such as NPSA
- The RPHA should build upon the connections which have already been established UK wide and all-Ireland wide
Q7 The Department is seeking your views on the proposal to incorporate Health and Social Care Trust specialist health improvement functions into the Regional Public Health Agency.
Response:
As stated in our response to Question 6, the RPHA should not incorporate specialist Health Improvement staff from Trusts or HAZ staff.
Q8 The Department is seeking your views on the proposal that, in the future, local government could be required, through legislation, to consult with the Regional Public Health Agency when developing its community plans.
Response:
We strongly support the concept of community planning. We also strongly support the specific proposal that, in future, local government would have included in its legislation a requirement for ‘power of wellbeing’. This legislation would be useful but, by itself, would not ensure integrated working. Therefore, HSC structures which are put in place, must be coherent, and understood by multiple stakeholders so that strong partnership and inter-sectoral working continues to be supported.
Q9 The Department is seeking your views on the proposal that the Regional Health & Social Care Board and its Local Commissioning Groups would be required, through legislation, to seek advice from the Regional Public Health Agency when developing their commissioning plans.
Response:
We are supportive of this proposal. Again, legislation would not, by itself, ensure that there is integrated working. The key to successful connections between Public Health and the wider HSC system is to ensure that functions are co-located at a local level and that there is a interchange on a daily basis between those who work for the RPHA, the RHSCB and the CSO in order to support the pivotal role that LCGs will play in assessing needs and commissioning services efficiently and effectively to meet those needs.
Q10 The Department is seeking your views on the proposal to appoint the Chief Executive or a senior Executive of the Regional Public Health Agency as a non-Executive of the Board of the Regional Health and Social Care Board.
Response:
We are of the view that in order to ensure integrated working between the RHSCB and RPHA, the Chief Executive or Senior Executive of the RPHA should attend meetings of the RHSCB, but should not be a non-Executive Director of the RHSCB.
Q11 The Department is seeking your views on the proposal of how to make the work of the Regional Public Health Agency fully multi-professional.
Response:
We would contend that the RPHA does not need to have multiple professionals within its organisation, but could instead source professional advice from the RHSCB and the CSO. The integration of strategy and policy would take place at the RHSCB, integrated working would take place at an operational level through co-location of functions and staff to support the working of LCGs.
Q12 The Department is seeking your views on the proposals for the Agencies referred to in Section 8.
Response:
In line with the drive for streamlining the HSC and allied systems, we hold the view that all the agencies mentioned in para 8.1 should be brought together and housed within a separate section as part of the CSO, thereby reducing the number of Boards and streamlining support arrangements for those agencies.
In terms of the agencies mentioned in paras 8.2, we support the view that RQIA should remain as a separate organisation, and also support the proposal that its role and remit needs to be reviewed within the new governance framework for the reconstituted HSC system. RQIA should, we feel, include in future the functions of the Mental Health Commission.
We support the view that the Medical Physics Agency should become part of the Belfast Trust.
We support the view that the functions currently undertaken by the CSA should be incorporated within the proposed CSO.
In relation to Health Estates we are of the view that it should be included within the RHSCB because it is essential to make more explicit the link between commissioning of services and plans for the future built environment in which services will be delivered. Capital development must be lead by the commissioning agenda.
Q13 The Department is seeking your views on the proposals for the two options, set out in Section 9, to replace the HSS Councils.
Response:
We support Option 2 of the proposal as it offers a strong base for local influence and challenge to the HSC system. We support the view that the five HSS Council offices should be required by legislation to work together collegiately and with an annual programme of meetings. This could be done through the five Chairs and Chief Officers of the HSS Council Offices coming together in a unified forum.
Q14 The Department is seeking your views on the constitution of the new organisation(s) under each of the proposed options, set out in Section 9, to replace the HSS Councils.
Response:
We are generally supportive of the proposals set out in para 9.6 (page 41) of the consultation document. We are of the view that the size and composition of the HSS Councils should take account of the need for nominees from the new local authorities. We also believe that organisations from the community sector should have a strong representation on the HSS Councils.
As we indicated in our response to earlier questions, thought needs to be given to how political representation on the HSS Councils would work in the context of political inputs to other parts of the reconstituted HSC, including LCGs and the RPHA.
We fully support the view that the merit principle will continue to underpin the selection process of Board members on the HSS Council.
Q15 The Department is seeking your views on the human rights implications of the proposals for Health and Social Care reform and any issues you think relevant.
Response:
In our view there are three aspects of human rights to consider. The first is the human rights of service users and carers. In this regard, we are of the view that the human rights of service users and carers would not be adversely affected because of the proposed restructuring of health and social care, provided that resources are allocated fairly and that local populations have a strong voice through strong local commissioning arrangements.
The second aspect is to ensure that the rights of social groups (especially those who are marginalized and ethnic groups) are safeguarded.
The third dimension of human rights relates to staff. These will, again, not be adversely affected provided that the principles set out by the Public Service Commission are consistently and transparently applied.
Q16 Can you identify any additional relevance evidence or information which the Department should have considered in assessing the equality impacts of these proposals?
Response:
We are of the view that there are no other issues which the Department needs to consider over and above those set out in the consultation document.
Q17 Can you identify any other potential adverse impacts, with supporting evidence, which might occur as a result of these proposals being implemented?
Response:
This question has a direct connection with question 20 and we develop our issues more fully in response to question 20, however, the issue of location of services is central to the issue of equality when implementing the proposed changes to the HSC structure.
At a general level, we would highlight the following issues:
- The greater majority of jobs in the Western area are in the public sector
- There is high deprivation in the Western area. The five District Councils in the Western area are in the top 11 of the most deprived Councils in Northern Ireland, and Derry and Strabane have particularly high levels of deprivation as measured against social and economic indices.
- A high percentage of female employees (including those married with children) in the Western area are employed in jobs which will be directly affected by the restructuring of the HSC. The issues of work life balance need to be considered in terms of any changes to travel times and career opportunities
- There are concerns (as evidenced by the decision relating to jobs in the Service Delivery Unit) that senior positions in the HSC will flow out of the Western area under the proposed restructuring
- There are concerns and evidence from elsewhere in the UK that reorganisation leads to further centralisation. We emphasise the need to avoid what we term ‘gravitational pull’ towards the centre. We also contend that it is very important not to consider the location of bases in the health and social services sector in isolation from the location of other RPA affected organisations
We need to see clear evidence of living out the aspirations as set out in the document entitled ‘Report on Workplace 2010 and Public Sector Jobs Location’ in dispersing public sector jobs across NI, having particular regard to population base, potential recruitment pools and socio economic deprivation. The framework for the public sector jobs in Northern Ireland needs to be equality proofed and care is needed that temporary arrangements put in place do not become permanent solutions by default.
Q18 Can you suggest any other mitigating measures to eliminate or minimise any potential adverse impact on the staff concerned?
Response:
The mitigating circumstances are:
- Ensuring that the service framework for public service jobs fulfil the aspiration of dispersing jobs, including senior jobs across Northern Ireland in general and the West in particular
- Ensuring that individuals’ personal circumstances are actively and sympathetically taken into account in the selection and recruitment process for jobs and the retention of jobs. In this regard, the principles set out by the Public Service Commission need to be implemented in full.
- Embracing the concept of flexible working
- Embracing the concept of fully utilising technology to allow ‘virtual organisations’ and networks to be facilitated
- Exploiting the facilities of teleconferencing and video links to enable remote working to become a reality
- Making use of existing buildings within technology assisted organisational arrangements
Q19 Have the needs of the Section 75 categories of people been fully considered in this EQIA? If not, please provide details and supporting evidence.
Response:
There is evidence in the consultation document of awareness of the potential impact on Section 75 categories, however much more work is required to demonstrate that the impact of the proposals on each category within each major geographical area in Northern Ireland has been quantified.
Q20 Do the proposals afford an opportunity to promote equality of opportunity and/or good relations?
Response:
Again, we have considered this from two dimensions.
Equality of opportunity and good relations from the service user dimension will be developed if the proposals deliver the following outcomes:
- Strong local commissioning arrangements through well supported LCGs
- Checks and balances to ensure that resources are fairly distributed and increasingly targeted on areas of greatest need.
- Ensuring that the internal reorganisation of the HSC does not in any way undermine strong partnership working and stakeholder involvement through networking with local community groups and through properly supported community planning arrangements
- There are clear lines of communication and accountability at local and regional level
- In terms of staffing, equality of opportunity needs to be demonstrated through:
- building on existing skill bases;
- avoiding over-centralisation of functions and jobs, including senior jobs;
- fully utilising and exploiting modern technology to support a dispersed organisation; and
- taking into account the Guiding Principles set out by the Public Service Commission.
General Comments
Response:
We fully accept that there is a need to reform and streamline the health and personal social services in Northern Ireland.
Generally, we welcome the proposals set out in the consultation document, subject to the points we have made in response to the questions set out above.
There is a need to ensure that in designing the system for the future, it is fit for purpose, is coherent and is understood by those who use it and those who work in it.
We need to avoid the pull towards centralisation, because there is no need to do so, given the breadth and depth of skilled staff in the system currently.
It is very important to have strong commissioning at regional and local levels. In order to achieve this, it will be important to have a clarity about roles and responsibilities between the RHSCB and the RPHA. The primacy must rest with the RHSCB, and the RHSCB must have adequate staffing resources regionally and locally to ensure that there are effective commissioning arrangements in place to deliver on the reform, modernisation and redesign of services.
We would emphasise the following from the perspective of the Western area:
- LCGs must have a strong local voice and presence. They must be empowered and supported to carry out a central, meaningful commissioning role
- Local partnerships across the mixed economy of care and with other statutory agencies, are maintained and transferred into the new arrangements, especially community planning
- Resources are increasingly targeted on areas and issues of greatest need
- Governance arrangements are clear and channels of communication are effective and lines of accountability are unambiguous
- The system which is put in place is unified in a way which ensures that appropriate functions and staff to fulfil those functions are located in a way in which integrates, rather than separates.
- Integration of parts of the system is best effected through arrangements such as putting people from different parts of the one organisation on the Board of the RHSCB
- That staff reductions can be achieved and unnecessary bureaucracy can be reduced without unnecessary centralisation of functions and jobs
In the round, the proposals will be able to deliver the intended outcomes, provided there is now a period of careful planning and design to ensure that the Minister’s aspirations for the system are actually delivered.
RQIA
Further to your letter dated 4 July 2008, inviting a written submission on the Health and Social Care (Reform) Bill, I am pleased to provide a response from the Regulation and Quality Improvement Authority (RQIA).
The RQIA welcomes the opportunity to provide the Health Committee with comment on the Health and Social Care (Reform) Bill.
The RQIA recognises that the proposals seek to ensure clarity of function for all organisations under the new structures. This will be essential for improved performance and good governance. The public and staff must be presented with a clear understanding of the roles and responsibilities of each organisation within the new system. The accountability relationship between the new organisations and the DHSSPS must be stated clearly to avoid any ambiguity.
The RQIA considers that the new organisational model can continue to deliver on all aspects of health and social care in a seamless integrated way, in the best interests of the public and of staff working in the sector. The RQIA welcomes the proposal to create a new organisation with a specific remit for the promotion and protection of the health and wellbeing of the population of Northern Ireland. The new Regional Public Health Agency can be a catalyst for action across organisations to improve health but will need to work collaboratively with the new Regional Health and Social Care Board.
The RQIA supports the introduction of this Bill which will give increased clarity to health and social care structures in Northern Ireland and an increased focus on the improvement agenda championed by the RQIA.
The RQIA strongly supports the ‘Transfer of functions of the Mental Health Commission’ contained in Clause 25 of the Bill and believes that there is a clear rationale for this change. Since the initial proposals under the Review of Public Administration, RQIA has been working closely with the MHC in developing plans, to ensure that the proposed transfer of functions takes place seamlessly and within agreed timescales.
Following the transfer of the functions of the MHC to the RQIA, responsibility for Mental Health and Learning Disabilities will fall under the remit of a newly formed, separate and distinct team within the RQIA. It is expected that this team, operating within the structure of the RQIA, will develop an identity and ethos which reflects and improves on current practice within the MHC, whilst incorporating additional duties. The RQIA recognises that it must make provision in its governance structure for an increased emphasis on mental health and learning disabilities.
The RQIA believes that the distinctions between health care in general and other elements of care, for example, social care and mental health care are to some extent arbitrary. At present patients with mental disorder or learning disability access care in acute hospitals, children’s homes and nursing homes along with access to psychiatric units. The RQIA, through its activities will also ensure a focus on the quality and safety of the new and developing models of care in the community. This is an area where the RQIA already has significant involvement through its inspection and review activities.
Given this situation, it is logical to retain the RQIA title (The Regulation and Quality Improvement Authority), as its activities are generic, and this avoids absolute distinctions. It is also simpler for the public to be able to recognise that there is a single body responsible for the regulation for all health and social care services, irrespective of the area of their concern.
The main benefits of the transfer of the functions of the MHC to the RQIA are that RQIA will:
- retain and further develop a focus on the individual and the rights of service users and carers under the current functions of the MHC, whilst incorporating the powers of enforcement and improvement on organisations under the Health and Personal Social Services (Quality, Improvement and Regulation)(NI) Order 2003;
- place a renewed emphasis on how the existing legislation can assist in ensuring the objectives of the Bamford Review are met;
- promote multi-professional and lay working in a manner not currently available to the MHC through the RQIA’s programme of inspection and governance reviews;
- place an additional emphasis on the promotion and monitoring of services aimed at promoting health and well-being;
- create an opportunity for wider promotion of mental health advocacy, service user and carer engagement;
- allow for greater integration of the regulation and assessment of health and social care. For many individuals, particularly those with mental health problems, better outcomes from care often depend on health and social services working well together;
- facilitate the process of regulation through the integration of the functions of the RQIA and the MHC;
- use information and intelligence, including the views of patients, service users, carers and advocates, to target resources to the areas of greatest risk; and to help inform future inspection and review activity;
- provide comparable independent information across a wider range of health and social care services and settings.
In conclusion, the RQIA welcomes the emphasis on improving quality and standards in the key guiding principles underpinning the changes, and it looks forward to fulfilling its statutory role as the independent assessor of the health and social care systems and processes to improve quality within the new organisational arrangements.
The RQIA would be pleased to meet with Health Committee members to discuss in detail its vision for the delivery of its mental health and learning disability services in light of the Health and Social Care (Reform) Bill.
Royal College of Nursing
Northern Ireland
Introduction
1. RCN Northern Ireland welcomes this opportunity to make a written submission to the Committee in relation to the Health and Social Care (Reform) Bill. We hope that our comments will prove helpful to the Committee in its consideration of the draft legislation.
2. RCN Northern Ireland members have engaged closely with the Review of Public Administration in its application to health and social care services since its inception in 2002. We have consistently highlighted the need for the reformed structures to be able demonstrably to enhance patient and client care. We have also consistently stressed the need to ensure that the promotion of efficiency and productivity within the service does not eclipse the over-riding objective of constructing a system that meets the needs of individuals and communities, facilitates the highest possible standards of patient and client care, and enhances the health and well-being of the people of Northern Ireland.
3. Nurses in Northern Ireland have consistently embraced change, displayed a commitment to modernisation and worked tirelessly to ensure that patients are treated at all times with professional skill and human dignity, often under difficult circumstances and in many cases through working beyond their contractual obligations. RCN Northern Ireland welcomes the modernisation process where it is clearly leading to the establishment of a better health and social care system. It is in this spirit of broad support for, and engagement with, the underlying principles of the reform process that we submit our comments to the Committee.
4. RCN Northern Ireland has two substantive comments upon the draft legislation and these are noted below.
Clause 8: Functions of the Regional Board
Clause 9: Local Commissioning Groups
5. Clause 8 (3) states that “the Board must consult RAPHSW [the Regional Agency for Public Health and Well-being] and have due regard to any advice or information provided by it”. Clause 9 (4) (i) states that each Local Commissioning Group must “consult RAPHSW and have due regard to any advice or information provided by it”. In both cases, RCN Northern Ireland believes that this wording is insufficiently robust and should be strengthened.
6. The Minister has previously stated his intention “to put the public health agenda at the heart of the Health and Social Care system” and views the new Regional Agency for Public Health and Social Well-being as the key to securing this objective. However, we believe that requiring the commissioning authorities merely to consult and have due regard to advice and information provided by RAPHSW may not secure the full integration of public health and commissioning that will be essential in order to give effect to the Minister’s objectives.
7. Accordingly, we suggest that the wording of the relevant phrase within clause 8 (3) be amended to “the Board must work in partnership with RAPHSW and be able to demonstrate that its commissioning plan reflects the priorities determined by RAPHSW”. Similarly, clause 9 (4) (i) should be amended to reflect the need for each Local Commissioning Group to “work in partnership with RAPHSW and be able to demonstrate that the exercise of its functions reflects the priorities determined by RAPHSW”.
8. In this way, the relationship between RAPHSW on the one hand and the Regional Board and Local Commissioning Groups on the other will become one of strategic partnership rather than simply consultation and advice. This will, in turn, help to ensure that public health is firmly at the forefront of service design and delivery, as RCN Northern Ireland endorses and the legislation intends.
Schedule 1: The Regional Health and Social Care Board
Schedule 2: The Regional Agency for Public Health and Social Well-Being
9. In our response to the February 2008 DHSSPS consultation Proposals for health and social care reform, RCN Northern Ireland stated that the Regional Health and Social Care Board [RHSCB], with no defined input from nursing, medicine or social work, risks reducing the management of the health and social care system to the status of financial accounting, with no consideration given to the quality of care and treatment, the assessment of outcomes or the extent of the patient and client experience. In order to ensure that the service is fit for purpose, it must be clinically governed as well as financially managed. Its membership must include nursing, medicine and social work at the top table. Our view on this issue was shared by the British Medical Association.
10. The draft legislation (Schedule 1 (3) (2) and (13) (2); Schedule 2 (3) (2) and (13) (2)) currently states that appointments to the RHSCB and RAPHSW will be determined on the basis of regulations made by the DHSSPS. Whilst we accept that primary legislation is not necessarily the appropriate means to define in detail precise staffing arrangements, we do feel that this is a missed opportunity to ensure that the top tables of the RHSCB and RAPHSW are inclusive of the three key professional groups that will be primarily responsible for delivering the new health and social care agenda to patients, clients and communities. We wish to draw the Committee’s attention to this point and seek its endorsement of the need to ensure that the membership of the RHSCB and RAPHSW includes nursing, medicine and social work at the top tables in order to ensure that it is fit for purpose and provides appropriate leadership. We believe there is potential for these appointments to be of a joint nature between the RHSCB and RAPHSW in order to strengthen partnership working and minimise cost.
Conclusion and further information
11. RCN Northern Ireland reiterates our gratitude to the Committee for inviting this submission and we hope that our comments will prove helpful to the Committee in its detailed consideration of the draft legislation. We urge the Committee to give their response to the Bill immediate consideration to ensure that the target of 1 April 2009 is met. We would be concerned about the impact of any delay on patient care and staff morale.
12. The RCN would be happy to meet the Health Committee for further comment on the Bill or to clarify any of the issues detailed above. For further information about the work of the RCN in support of nurses and patient services in Northern Ireland, please contact Dr John Knape, RCN Northern Ireland Head of Communications and Policy, at john.knape@rcn.org.uk or by telephone on 028 90 384 600.
Children in Northern Ireland
Introduction
Children in Northern Ireland (CiNI) is the regional umbrella body for the children’s sector in Northern Ireland.
CiNI represents the interests of its 117 member organisations, providing policy, information, training and participation support services to members in their direct work with and for children and young people. CiNI has recently opened up its membership to colleagues in the statutory children’s sector recognising that the best outcomes for children are increasingly achieved working in partnership with all those who are committed to improving the lives of children and young people in Northern Ireland. As part of our commitment to partnership working to promote the best interests of children and young people, CiNI and our members are represented on the four HSSB multi-agency Children and Young People’s Committees. CiNI has played a key role in co-ordinating and supporting voluntary and community sector representation on the four Committees.
CiNI welcomes the opportunity to respond with written comments to the Health, Social Services and Public Safety Committee’s consideration of the Health and Social Care (Reform) Bill.
CiNI has an active and ongoing interest in the reform process and in May 2008 we responded to the Department’s consultation on its Health and Social Care Reform Proposals[1] from which the reform legislation has now emerged. We would be happy to provide any further evidence/input to the Committee as it takes forward its consideration of the Reform Bill.
In addition to providing specific written comments on the individual sections of the Reform Bill, CiNI would also like to provide some general comments on issues of relevance and importance to the children’s sector, that must be dealt with as part of the Reform Bill, but which are not, at present, explicit on the face of the Bill.
General Comments
In our response to the Department’s consultation on its reform proposals we detailed our significant concerns that the proposals made no provision for the future of statutory children and young people’s services. It is therefore extremely welcome that the Minister in announcing his decisions on the way forward following consultation, acknowledged our concerns and dealt specifically with the issue of statutory responsibility for children’s services planning. The Minister in his announcement confirmed that existing statutory responsibility for children’s services planning will become the responsibility of the new Regional Health and Social Care Board, and he also stated that he would consider proposals that would strengthen and build upon the children’s services planning process[2].
Currently statutory responsibility for children’s services planning sits with the four Health and Social Services Boards who are required to produce children’s services plans under the Children (NI) Order (Amendment) (Children’s Services Planning) Order (Northern Ireland) 1998. CiNI notes that the Reform Bill at section 8 deals with the functions of the new Regional Board and at section 24 addresses the transfer of statutory functions of the Health and Social Services Boards to the new Regional Board. We trust that section 24 (2) encompasses and addresses the transfer of statutory responsibility for children’s services planning from the four HSSBs to the new regional body. CiNI would ask that the Committee seek to clarify and gain confirmation that children services planning has indeed been transferred to the regional body under section 24 (2), and is one of the functions of the new Regional Board under section 8.
CiNI welcomes the Minister’s commitment to strengthen and build upon children’s services planning and we believe that the current reform process presents a unique opportunity to achieve this. We would highlight to the Committee that the four HSSB Children and Young People’s Committees who have overall responsibility for the planning process have produced proposals to enhance and further develop the planning process by addressing the ‘major deficits’ inherent in the current process[3]. We have appended the proposals to this response and would strongly advocate that the Committee give these their urgent consideration with a view to endorsing these to the Minister as the way ahead for the future planning and commissioning of children’s services and to integrate these proposals within the current reform process.
Children’s Rights Framework
To further underpin the proposals of the four Children and Young People’s Committees, CiNI would highlight to the Committee that any proposals to strengthen and build upon children’s services planning must be firmly grounded in the children’s rights framework which the Department has signed up to through the cross government 10 Year Children and Young People’s Strategy. Statutory provision for children’s services planning must integrate the over-arching guiding principles of the United Nations Convention on the Rights of the Child (UNCRC) which is to inform and guide the Department’s delivery of the strategic outcomes of the 10 Year Strategy. Ultimately, reflecting on the guiding principles for reform which the Minister has set[4], statutory children’s services planning must be child-centred and responsive to the rights and needs of all children and young people, promoting their best interests (UNCRC Article 3) in a non-discriminatory manner (UNCRC article 2). Fundamentally and again reflecting the Minister’s guiding principles for reform, children and young people must be given the opportunity to be heard and have their views given due weight and consideration (UNCRC article 12) at all levels in the planning and commissioning of children’s services.
Statutory Duty to Co-Operate
CiNI would also highlight to the Committee that, as outlined by the four Children and Young People’s Committees, proposals to strengthen and build upon children’s services planning must have at their core a statutory duty to plan and commission children’s services across agency. The Children and Young People’s Committees have recognised the absence of this statutory duty as a limitation within the current children’s services planning process where, despite much good practice multi-agency planning at locality level, the process has been reliant on goodwill in the absence of a requirement for agencies to co-operate and work together.
CiNI therefore recommends that expanded and enhanced provision for children’s services planning within the new arrangements for health and social care should be underpinned by a statutory duty to co-operate to deliver the Ten Year Children and Young People’s Strategy. The statutory duty would be initiated at Ministerial level underpinning the functioning of the Ministerial Sub-Committee on Children and Young People, and would operate at departmental, regional and local levels facilitating and enabling the joint planning and commissioning of services for children to meet the outcomes of the Ten Year Strategy.
Role of the Voluntary and Community Sector
CiNI would strongly recommend that the role of the children’s voluntary and community sector is explicitly recognised within the statutory duty to co-operate thereby ensuring the sector’s established and central role with the existing process is maintained and protected within future arrangements for children’s services planning. We would recommend that there is recognition of the voluntary and community sector as a key partner in the initiation, maintenance and facilitation of the planning process. In other jurisdictions similar recognition of ‘other persons or bodies’ who ‘exercise functions or are engaged in activities in relation to children’ has been included in legislation[5].
Comments on Sections of the Bill
Section 2 Department’s general duty
CiNI welcomed the Minister’s announcement on the way forward for health and social care, where he stated that he would ensure that social care is fully embedded into the entire health agenda[6]. However we do need to see this commitment explicitly followed through in the Reform Bill. Therefore at 2 (3) (a) and (g) the Department must commit to reducing health and social well-being inequalities between people in Northern Ireland.
We also note that as part of its general duty the Department under 3 (c) must allocate financial resources available for health and social care, having regard to the need to use such resources in the most economic, efficient and effective way. We note that this is a theme that runs throughout the Reform Bill and it is unclear whether there exists a hierarchy in relation to these criteria. We would strongly recommend in line with the overall objectives of the DHSSPS, as outlined in its Equality Scheme, that primary consideration must be given to ensuring that effective health and social care services are available to all.
Section 4 Department’s priorities and objectives
CiNI would highlight that with regard to determining and revising priorities and objectives for the provision of health and social care, the Department’s statutory responsibility under section 75 of the NI Act 1998 to promote equality of opportunity when carrying out functions, such as the setting of priorities and objectives, much be explicitly recognised and adhered to. The Department, in its Equality Scheme, has set out arrangements for assessing and consulting representative groups and individuals on the likely impact of its policies on equality of opportunity and for monitoring any adverse impact of its policies on the promotion of equality of opportunity. The term ‘policies’ covers all the ways in which an authority carries out or proposes to carry out its functions relating to Northern Ireland.
Therefore while section 4 would suggest that the requirement on the Department to consult on it priorities and objectives is limited and indeed provides a ‘get out’ from consultation, the Department remains bound by section 75 to consult on the likely impact of its priorities and objectives on the promotion of equality of opportunity. CiNI would strongly advocate that section 4 includes a specific statement that recognises in setting its priorities and objectives the Department must also give due regard to its other relevant statutory obligations namely section 75.
Section 5 The Framework Document
Again in relation to the development of the framework document CiNI would reiterate the above point regarding the Department’s section 75 duty to promote equality of opportunity. It is crucially important that service users including children and young people have a say in the process of determining the priorities and objectives of each of the health and social services bodies.
We note section 5 (5) in relation to the preparation of the framework document which states that while the Department must consult each health and social services body as respects its functions, or persons considered by the Department to represent that body; there is a subtle but significant change of emphasis when it then states that it may consult any other persons the Department considers appropriate. CiNI would advocate that this provision is amended to state that the Department must consult in accordance with the Order and any other relevant statutory provision namely section 75.
In relation to 5 (4) (b) the Department must carry out its duties … in the manner and to the extent that appear to it to be best calculated … to promote the economy, efficiency and effectiveness of health and social care bodies, we would reiterate the comments made above, in line with the overall objectives of the DHSSPS, as outlined in its Equality Scheme, primary consideration must be given to ensuring that effective health and social care services are available to all.
Section 6 Power of Department to give directions to certain bodies
CiNI notes that under 6 (4) it is the duty of a body to comply with any directions given to it, however the issue of non-compliance with directions is not dealt with, that is, what powers does the Department have when a body fails to comply with directions. The Committee may wish to consider what would be necessary to allow the Department to take the necessary steps to secure compliance.
Section 7 The Regional Health and Social Care Board
Functions of the Regional Board
As referred to above in our general comments, CiNI welcomed the statement made by the Minister to the effect that children’s services planning would transfer from the HSS Boards to the new Regional Health and Social Care Board. We trust that the transfer of statutory responsibility for children’s services planning is dealt with through Section 8 Functions of the Regional Board and Section 24 Transfer of functions of Health and Social Services Boards.
We also note that in relation to the functions that have been transferred, under 8 (4) these are deemed to be functions which the Department has directed the Regional Board to exercise. Therefore, following this through with regards children’s services planning, the assumption is that the Department has directed the Regional Board to exercise statutory responsibility for children’s services planning, which is extremely welcome. We would therefore encourage the Department to promote and drive forward the children’s services planning process at government level.
We also note that in relation to section 8 (3) the preparation of the commissioning plan, that the Regional Board must consult the Regional Agency for Public Health and Social Well-Being (the Agency) and have due regard to any advice or information provided by it. We would strongly advocate that this provision must be stronger and that there should be pro-active engagement by the Agency in the development of the Board’s commissioning plan so that there is joint working in the preparation of the commissioning plan, perhaps through representation of the Agency on the Local Commissioning Groups.
Local Commissioning Groups
CiNI notes section 9 (3) (a) each Local Commissioning Group shall exercise such functions with respect to the commissioning of health and social care as may be prescribed and (b) such other functions as the Regional Board may, with the agreement of the Department, determine. We would request that the Committee probe this issue further to find out what other functions may be envisaged. CiNI would recommend that the Committee require the Regional Board and the Department in determining other functions, which may not be directly linked to the core commissioning function of the Groups, to ensure full and transparent public consultation on these functions in line with the statutory requirements of section 75.
We also note section 9 (4) each local commissioning group must (b) in connection with the exercise of its functions (i) consult RAPHSW and have due regard to any advice or information provided by it; and (ii) undertake other such consultation as the Department may direct.
From this it appears that the only body which the LCGs are explicitly required to consult with is the Regional Agency. We would strongly advocate for the inclusion of a requirement that in connection with the exercise of its functions, the LCGs must consult all the people of the area for whom they will be commissioning health and social care.
In relation to 9 (4) (i) we would advocate that each LCG, through the local representation of the Regional Agency on each group, should do more than consult the Agency, rather they should work with the Agency in the exercise of their functions.
We also note section 9 (5) each Local Commissioning Group must exercise its functions with the aim of (c) securing the delivery to people in that area of health and social care that is efficient, co-ordinated and cost effective. Again we would reiterate the primary consideration of the legislation must be to ensure that the reforms enable the planning, commissioning and delivery of health and social care that will be effective in meeting the needs of people. We would strongly advocate that in keeping with 9 (5) (b) this should be amended to state securing the delivery to people in that area of health and social care that can effectively meet their needs.
Further, in relation to 9 (5) (d) in addition to improving the availability and quality of health and social services in their area, the LCGs must also aim to improve the accessibility of services for users. Improving availability of services provides no guarantee that those most in need of these services, that is, those from already marginalised and disadvantaged communities will be able to access and receive equal benefit from these services.
Schedule 1 The Regional Health and Social Care Board
We note that Schedule 1 (7) provides for the appointment of Committees, namely LCGs. The Schedule provides limited further information on these Groups, in terms of membership it says little other than 7 (3) a person who is not a member of the Regional Board shall not, except with the approval of the Department, be appointed to a committee.
While it is welcome that as a result of responses to the consultation on the reform proposals that the Minister has now provided additional places for the voluntary and community sector on the LCGs, we remain concerned that the Schedule provides no further clarity on the role and functions of the committees. This is an issue which the Committee will wish to give further consideration to.
Further, we note that the Schedule at 7 (1) (b) provides that the Regional Board may appoint one or more other committees to which it may delegate such of its functions as it sees fit. If the Regional Board were to appoint additional other committees we would urge the Board to ensure that in doing so it engages in full, public consultation on the setting up of such Committees in line with section 75.
In regard to Schedule 1 20 (1) relating to the recording of information by the Regional Board, we would recommend that the Department should direct the Regional Board to record all the information which would be necessary and appropriate to enable the Regional Board to monitor, analyse, report and review the exercise of its functions.
Section 12 The Regional Agency for Public Health and Social Well-Being
In regard to section 13 which addresses the functions of the Regional Agency, we note the Minister’s comments made in his announcement on the way forward, where he stated that he would ensure that social care is fully embedded into the entire health agenda. We would therefore advocate that it is essential to ensure that social well-being is fully embedded in the functions of the new Regional Agency. In relation to 13 (1) and (2) we would recommend that the functions of the new Agency should be amended to reflect the new title and overall focus of the new Agency, that is, the functions should relate to health and social well-being improvement; and health and social well-being protection.
In relation to 13 (2) (a) the health improvement functions should be amended to reflect the more holistic focus of the new Regional Agency. As well as securing the improvement of the health and social well-being of people in Northern Ireland, the functions must include reducing health and social well-being inequalities between people in Northern Ireland; and health and social well-being promotion. Without these amendments to the Regional Agency’s functions, we would suggest that it is a Regional Agency for Social Well-Being in name only.
In relation to section 13 6 (a) and (b) we would advocate that it is essential that there is a strong duty to co-operate in the exercise of their functions between the Regional Agency and the Regional Board and Local Commissioning Groups.
Schedule 2 The Regional Agency for Public Health and Social Well-Being
We note also at Schedule 2 sections 7 and 8 that the Regional Agency, in the same way as the Regional Body, can appoint Committees and Sub-Committees. However we are unaware of any plans at this point to create such Committees. There should be a strong requirement on any existing or future committees of the Regional Agency and Regional Body to co-operate closely in the exercise of their functions.
In regard to Schedule 2 20 (1) relating to the recording of information by the Regional Agency, we would recommend that the Department should direct the Regional Agency to record all the information which would be necessary and appropriate to enable the Regional Agency to monitor, analyse, report and review the exercise of its functions.
Section 14 The Regional Support Services Organisation
In relation to Section 15 (2) which lists the supports services which are to be provided by the Regional Organisation to other health and social care bodies, we are concerned that in effect some of these ‘support services’ could be described as ‘core services’ linked closely to the delivery of the functions of health and social care bodies, and it would be unhelpful to remove a function such as ‘information management’ and place it in a separate organisation, which inevitably is removed from the core functioning of the other health and social care bodies and which can charge for the provision of such support services.
Section 16 The Patient Client Council
CiNI notes the functions of the Patient Client Council as set out at 17 (1) –
(a) representing the interests of the public;
(b) promoting the involvement of the public;
(c) providing assistance (by way of representation or otherwise) to individuals making or intending to make a complaint relating to health and social care for which a body to which this section applies is responsible;
(d) promoting the provision by bodies to which this section applies of advice and information to the public about the design, commissioning and delivery of health and social care;
(e) such other functions as may be prescribed.
It is our specific concern to advocate strongly that the Council in carrying out its functions give due regard to its Section 75 duty to promote equality of opportunity which should underpin and inform the manner in which the Council carries out its functions in respect of vulnerable individuals, groups and communities. In particular we would highlight that the Council must ensure that it has the required expertise and competence in representing the interests; promoting the involvement; and providing assistance to children and young people and their parents/carers.
We also note section 17 (5) The Patient and Client Council shall –
(a) undertake research and conduct investigations into the best methods and practices for consulting the public about, and involving them in, matters relating to health and social care; and
(b) provide advice regarding those methods and practices to bodies to which this section applies.
We would highlight that under section 75 Government departments and their statutory agencies in promoting equality of opportunity when carrying out their functions are already required to consult directly with affected groups and individuals. The Council should be aware of and give due regard to the Equality Commission for Northern Ireland’s Guide to Implementing Section 75 of the NI Act 1998. As a result there are already models of best practice and much evidence relating to timely and effective involvement and consultation with the public in decision making processes and we would urge the Council to begin with an audit of the methods and practices already in existence as a means of informing of its work.
In relation to involvement and consultation with children and young people we would strongly advocate that the Council take cognizance of the Equality Commission for NI’s Guidance for Public Authorities on Consulting and Involving Children and Young People[7].
In this regard we would also highlight the role and remit of The Participation Network which is supported by OFMDFM[8]. The Participation Network works with Government departments and statutory agencies in Northern Ireland to develop their capacity to fulfil their duties to effectively engage and involve children and young people in decision making. In view of 17 (5) (b) we would strongly recommend that the Council should advise the health and social care bodies, to which this section applies, to engage pro-actively with The Participation Network to ensure that they have the required knowledge, skills and expertise to consult and involve children and young people in matters relating to health and social care.
Section 18 Duty to co-operate with the Patient and Client Council
While we welcome the requirement on health and social care bodies to co-operate with the Patient and Client Council we have grave concerns that 18 (2) significantly undermines the spirit of co-operation, leaving it entirely to the discretion of the health and social care bodies to decide on what and when they will co-operate with the Council.
Section18 (2) (a) states that a body must- consult the Patient Client Council with respect to such matters, and on such occasions, as the body considers appropriate, having regard to the functions of the Council.
Therefore, in essence the body decides what it will consult the Council on, and when it will consult the Council, having regard to the functions of the Council. This can in no way be defined as co-operation.
Section 18 (2) (b) states that a body must- furnish to the Council, subject to such conditions as the body may specify, such information as the Council considers necessary to enable it properly to exercise its functions.
Therefore, it is entirely possible that a body may furnish information to the Council which the Council considers necessary to enable it properly to exercise its functions, BUT placing on the information such conditions that could in effect act to prevent the Council using the information in a way that would allow it properly to exercise its functions. Again this can in no way be defined as co-operation.
We also note 18 (3) which states that regulations may make provision authorising members of the Patient and Client Council to enter, for the purposes of any of the Council’s functions, certain premises as further defined. Under 18 (5) the power of entry is exercisable only so far as is necessary for the purpose of enabling the Patient and Client Council to exercise its functions, and is subject to such conditions as may be prescribed.
The power of entry may be particularly significant and important for the Council in carrying out function 17 1 (c) to provide assistance to individuals making or intending to make a compliant relating to health and social care; however its usefulness in this context will be limited if the regulations do not provide for what the member(s) of the Council can and cannot do upon gaining entry to a specified premises. We would suggest that given the sensitivity of these powers they would be more appropriately dealt with in primary legislation as opposed to regulations.
Overall considering the boundaries that are proposed to the role and functioning of the Patient Client Council, we would suggest that this brings into question the status and value which the health and social care system places on a Patient and Client Council. We would strongly advocate that the Committee give particular consideration to how it can strengthen the Council’s role and functions so that it can be a relevant and effective body protecting and promoting the public’s interest with regard to health and social care.
Public Involvement and Consultation
CiNI notes sections 19 and 20 relating to public involvement and consultation and the production of consultation schemes respectively. We would highlight that these articles must not circumvent the existing duty on public bodies delivering health and social services to promote equality of opportunity according to section 75 of the NI Act 1998. Any further development of these legislative provisions must be taken forward with due regard for the provisions of section 75. We would highlight that under section 75 designated health and social services authorities will be required to produce equality schemes and these will place consultation requirements on the new bodies. We would therefore advocate that in the interest of streamlining the functioning of these new and reformed public authorities that consultation schemes should be integrated within the equality schemes of new health and social services authorities.
Section 19 Public involvement and consultation
In reference to section 19 (1) (a) which provides that- each body must take such steps as it considers appropriate to promulgate information about the health and social care for which it is responsible, we would suggest that each body should develop an information and communications strategy to introduce, promote and raise awareness of it’s new/reformed role and remit amongst the general public. Such a strategy must also incorporate innovative approaches to reach out to marginalised and disadvantaged communities that will be particularly in need of the health and social care provided by the new and reformed bodies. Information must be provided through a variety of mediums encompassing both written and oral communication. Regardless of the medium chosen all information must be accessible, with age appropriate information produced for children and young people.
In reference to section 19 (1) (b) which provides that each body must take steps as it considers appropriate to obtain information about the needs of persons to whom care is being or may be provided; we would highlight that in relation to obtaining information about the needs of children, this is already being fulfilled as a critical element of the statutory children’s services planning process. Therefore we would suggest that this information gathering function is maintained and further developed at regional level as part of the transfer of the children’s services planning process to regional level.
Obtaining information about the needs of persons will necessarily require each body to engage and involve such persons in the planning and commissioning of care that is being or may be provided to them. We would highlight that currently children and young people are involved and actively participate in children’s services planning at local level, and within a strengthened and further developed children’s services planning process, must be involved at all levels from government to regional through to local level.
We have some real concerns with regard to section 19 (c) (i) which states that each body to which the section applies must take such steps as it considers appropriate- to encourage and assist persons to whom that care is being or may be provided – to avail of that care in an appropriate manner, having regard to the need to use resources in the most economic, efficient and effective way. If, as would appear to be suggested by the wording of this section, the expectation is that people to whom care is being or may be provided must have regard to the need to use resources in the most economic, efficient and effective way, we would suggest this is entirely inappropriate and unacceptable. For those to whom care is being or may be provided the most important consideration is that the care which they require is provided in such a way that it can deliver a timely and effective response to their health and social care needs. We would recommend that prior to the legislation progressing any further that the Committee in its consideration of the Bill remove section 19 (1) (c) (i).
Section 20 Public involvement: consultation schemes
We note section 20 (1) which requires that a health and social care body’s consultation scheme must set out arrangements for directly or through representatives involving and consulting, on certain matters, the Patient and Client Council; persons to whom care is being or may be provided; and the carers of such persons.
At section 20 (2) the matters are defined as-
(a) the planning of the provision of that care,
(b) the development and consideration of proposals for change in the way that care is provided, and
(c) decisions to be made by that body affecting the provision of that care
While we welcome the commitment to involvement and consultation we believe that those matters specified in 20 (2) are extremely narrow in scope. We would highlight that the section 75 duty on public authorities, including these health and social care bodies, to promote equality of opportunity is much broader and all encompassing in its scope requiring designated public authorities, including those delivering health and social care, in carrying out their functions relating to Northern Ireland to have due regard to the need to promote equality of opportunity. According to Section 98 (1) of the Act ‘functions’ includes ‘powers and duties’ and is of wide import. Furthermore, each health and social care body will be required to produce an equality scheme which must state the authority’s arrangements for assessing and consulting on the likely impact of its policies and for monitoring any adverse impact of its policies on the promotion of equality of opportunity. The term ‘policies’ covers all the ways in which an authority carries out or proposes to carry out its functions relating to Northern Ireland.
These functions go far beyond simply the provision of care, and include all of the processes whereby health and social care bodies plan, commission, deliver, monitor and review the care for which they are responsible. We would strongly advocate that rather than having various separate arrangements for consultation, these arrangements are dealt with comprehensively within the Equality Schemes of the new bodies.
Section 22 Public-private partnerships
CiNI is concerned at the potential impact this proposed provision on public-private partnerships will have on the role of the voluntary and community sector as a provider of public health and social services. We are particularly concerned to note that within section 22 there is no regulatory provision relating to the formation of public-private partnerships.
We would highlight that Government in Positive Steps its response to the Taskforce Report on Resourcing the Voluntary and Community Sector (DSD March 05) recognised an increasing role from the voluntary and community sector in the provision of public services. We would ask the Commitment in its consideration to probe the Department as to how it believes that the commitment made in Positive Steps sits alongside this current legislative proposal?
Section 24 Transfer of functions of Health and Social Services Boards
Again to reiterate our general comments, we trust that in line with the Minister’s statement which confirmed that children’s services planning would move to the regional body, that section 24 (2) encompasses the transfer of the statutory function of children’s services planning as currently provided for under the Children (NI) Order (Amendment) (Children’s Services Planning) Order (Northern Ireland) 1998. We would ask that the Committee seek to clarify and ensure that children services planning has indeed been transferred to the regional body under section 24 (2).
Section 25 Transfer of functions of the Mental Health Commission
As CiNI stated in response to the Department’s consultation on the reform proposals we do not believe that the Mental Health Commission should be transferred to the RQIA. As was recommended by the Bamford Review of Mental Health and Learning Disability we would again advocate that the Mental Health Commission should remain independent. If the Government is seriously committed to the Bamford agenda it must implement all of its recommendations in full and this includes the recommendation that the Mental Health Commission should remain independent. We would urge the Committee to give specific consideration to this issue with a view to encouraging the Minister to re-think his position on this issue and allow the Commission to remain independent.
CiNI also notes schedule 6 8 (4) which addresses the duties of RQIA in relation to mental health and which states that in addition to the functions that are transferred to it under the Reform Bill, the RQIA shall exercise 8 4 (b) such other functions relating to or connected with mental health as the Department may by order prescribe. We would urge the Committee to probe this further with the Department to find out precisely what other functions relating to or connected with mental health are envisaged as coming within this section.
Equality Impact Assessment
The Minister’s announcement on the way forward for health and social care reform did not acknowledge or adequately respond to the concerns which we raised in our initial response in relation to the Equality Impact Assessment. Therefore our concerns remain outstanding and we wish to bring these to the Committee for their urgent consideration.
The policy aim contained in the Department’s reform proposals centred on reforming and improving health and social care services for the benefit of the health and well being of the people of Northern Ireland, making services more efficient, more patient and client centred, and more focused on prevention and primary care and less on institution-based care.
However the people of Northern Ireland, patients and clients were not identified as ‘groups affected by the policy’, rather groups ‘primarily’ affected by the policy are identified as those who work within existing health and social care structures.
While it is relevant and important to consider the equality impacts of the proposals on the health and social care workforce, it is clearly evident that contrary to the policy aim the service users and more broadly the people of Northern Ireland are not the focus of the EQIA.
CiNI, in our response to the reform proposals, advocated that the EQIA should be carried out again so that it is properly informed by the Policy Aim and therefore accords primary or at least equal attention to the population of Northern Ireland, the service users and wider community, who should ultimately be the primary beneficiaries of improvement in health and well being brought about by reforms of the system.
CiNI notes that the Reform Bill’s Explanatory and Financial Memorandum at section 12 addresses the issue of Equality Impact Assessment. We are deeply concerned to note that while the Equality Impact Assessment of the Department’s proposals for health and social care reform concluded that the proposals may have an adverse impact on some of the section 75 groups, it has now been deemed sufficient to design procedures to ensure that there is no unlawful direct or indirect discrimination against any particular individual or group.
These procedures will not be sufficient to address the adverse impacts of the proposals on some of the section 75 groups. As is made clear in the Equality Commission for NI’s Guidance on Implementing Section 75 of the NI Act 1998 the promotion of equality of opportunity entails more than the elimination of discrimination. Discrimination of various kinds is already prohibited under a raft of anti-discrimination legislation. The promotion of equality of opportunity under section 75 requires proactive measures to be taken to secure equality of opportunity between the section 75 groups. We have grave concerns regarding this apparent lack of understanding of the fundamental concept of equality of opportunity enshrined by section 75.
The Procedure for Conduct of Equality Impact Assessments provides that where an assessment of impact concludes that proposals may have an adverse impact on some section 75 groups, even where these proposals are lawful (not discriminatory), the next step in the procedure is to the consider what to do in light of the adverse impact and this requires consideration of – measures which might mitigate any adverse impact; and alternative policies which might better achieve the promotion of equality of opportunity. The Equality Commission’s Guidance points out that the consideration of mitigating measures and alternative policies is at the heart of the EQIA process. We would suggest that if this fundamental step in the EQIA process is not undertaken then the process itself is flawed and should be undertaken again from the beginning and in full compliance with the procedure as laid out by the Equality Commission. CiNI would urge the Committee to give particular consideration to this issue with a view to recommending that the Department undertake the EQIA process again, so that it is properly informed by the policy aim, and that the procedure is followed through to its proper conclusion.
[1] CiNI (2008) Response to DHSSPS Consultation on Health and Social Care Reform Proposals http://www.ci-ni.org/images/uploads/CiNI_Response_HSC_Reforms.doc
[2] Ministerial Announcement 1st July 2008
[3] HSSB Children and Young People’s Committees, ‘A Joint Planning and Commissioning Framework to Improve Outcomes for Children and Young People’ p.4
[4] DHSSPS (2008) Proposals for Health and Social Care Reform, p.3
[5] Children Act 2004 http://www.opsi.gov.uk/acts/acts2004/ukpga_20040031_en_3#pt2-pb1-l1g10
[6] Ministerial Announcement, 1st July 2008
[7] ECNI (2008) Let’s Talk, Let’s Listen Guidance for Public Authorities on Consulting and Involving Children and Young People
[8] http://www.ci-ni.org.uk/theparticipationnetwork/
Northern Health and
Social Services Board
Thank you for the invitation, on behalf of the Committee for Health, Social Services and Public Safety, to comment on the draft Health and Social Care (Reform) Bill. The Northern Board appreciates the opportunity to make a contribution. I have structured the suggested amendments as you have requested and, for ease of reference, the new or amended text is in bold print in the attachment.
This is an important time in health and social care: change of this magnitude comes once every generation or so and it is incumbent on us all to do our very best to get it right. The legislative framework is important but it is only one piece in the jigsaw and we are mindful that there are a host of other issues which interface with each other and are critical to the success of this project. For example, the working relationships and the dynamics which will underpin all of this are left unexplored at this stage, although few would doubt the significance of getting these elements right. There are other issues critical to the success of this project, for example:
- Staffing matters –how do we harness the talents of the existing workforce to ensure that they continue to give of their best in the new arrangements?
- Location – where will posts be located? We have seen the location principles and engaged with the Bain Review over the past few months but until and unless the location issues are addressed for Health and Social Services staff, uncertainty will prevail. This is too important an issue to be left to chance. There is real concern in the workforce and in local communities that implementation of this phase of RPA will lead to the centralisation of posts in Belfast. Hundreds if not thousands of staff are affected by location decisions, not to mention local economies. The legislation is obviously silent on this issue but the introduction of the legislation will force the issue of location.
This issue has a disproportionate bearing on those who have caring responsibilities and are less well paid, as increased travel to work distances may become incompatible with their caring responsibilities and/or unaffordable. It is important that Public Policy changes have at their heart fairness in the geographical distribution of public employment opportunities and compliance with Section 75 responsibilities. We would urge the Committee to obtain irrevocable commitments on these points as it moves to consider the legislation.
- Business continuity – Over the next twelve months, the pace of change will be fairly rapid and organisations and individuals will be tasked with standing down their old responsibilities and acquiring new roles and duties. In all of this, services still have to be commissioned and provided and this will be a challenge to us all as we strive to ensure business continuity.
This is only a flavour of some of the issues that we will need to address over the coming months. Exciting, but challenging times are ahead for all of us and we need to work together to get this right.
I have had the privilege of addressing the Committee on a previous occasion: a colleague and I met with the Committee at the end of last year for a very frank and open exchange on the budget. I would be pleased to come along again to speak to the legislation and the other matters I have raised in this letter, if the Committee would find it helpful.
Health And Social Care (Reform) Bill – Proposed Amendments
Clause 2 - Department’s general duty
In Clause 2(1)(a)(i), after “physical and mental health”, insert “and well-being”.
(In recent years, the focus has very much been on health and well-being.)
In keeping with this theme, a related amendment is proposed to clause 2(5) where at the end of the definition of “health inequalities”, the words “and well-being” are added.
Clause 2(3)(g) should be omitted as this is more properly a function of the new RAPHSW and is already covered by clause 13(2)(a).
Clause 4 – Department’s priorities and objectives
A new clause 4 (4) is proposed to deal with those times the Department issues priorities or objectives without the requisite consultation –
“Clause 4(4) Where the Department has determined or revised priorities or objectives without the consultation specified in subsection (2), it shall revise those priorities or objectives within one year and in doing so must consult such bodies or persons as it thinks appropriate”.
Clause 5 – The framework document
An amendment is proposed to clause 5(4)(a) given the focus elsewhere in the legislation on the reduction of health inequalities in NI.
For Clause 5(4)(a) substitute “health and social care and the reduction of health inequalities between people in Northern Ireland”.
In both clause 5(4)(b) and (c) for “economy, efficiency and effectiveness”, substitute “economy, equity, efficiency and effectiveness”.
A new Clause 5 (7) is proposed -
“5(7) A health and social care body may propose revisions to the framework document and the Department shall have due regard to the health and social care body’s proposals”.
Clause 6 – Power of Department to give directions to certain bodies
A new Clause 6(3A) is proposed –
“Clause 6(3A) Where the Department has given directions without the consultation specified in subsection (2), it shall revise those directions within 1 year and in doing so must consult that health and social care body to which those directions apply”.
Clause 6(3)(b) should be omitted.
Clause 8 – Functions of the Regional Board
For Clause 8(2)(b)(iii) substitute “for ensuring that resources are used in the most economic, equitable, efficient and effective way in commissioning such care”.
Clause 9 – Local Commissioning Groups
For Clause 9(4)(b)(ii), substitute –
“undertake such consultation as the LCG considers appropriate”.
For Clause 9(5)(c), substitute “ securing the delivery to people in that area of health and social care that is efficient, equitable, co-ordinated and cost effective;”.
For Clause 9(5)(d), substitute “ improving the availability, accessibility and quality of health and social care in that area”.
For Clause 9 (7), substitute “ Before making regulations under subsection (6), the Department must consult the Regional Board and such other bodies or persons as it considers appropriate”.
Clause 10 - Power of Regional Board to give directions and guidance to HSC Trusts
For Clause 10(3), substitute “ The Regional Board must consult- the HSC Trust concerned and the Department, before giving any directions under subsection (1)”.
For Clause 10(6)(b), substitute “ to have due regard to any guidance given to it under subsection (2)”.
Clause 13 – Functions of RAPHSW
For Clause 13(5) substitute “ The Department may by order amend subsections (1) to (4) for the purposes of altering the functions of RAPHSW but only after consultation with RAPHSW in accordance with the Department’s consultation scheme.”.
Clause 15 – Functions of RSSO
For Clause 15(3)(a), substitute – “ secure that those services are provided in the most economic, equitable, efficient and effective way; and”.
Clause 19 – Public involvement and consultation
For Clause 19 (2), substitute – “ in particular, each body to which this section applies must, before the end of the period of 12 months beginning with the day appointed for the coming into operation of this section, or, if later, the establishment of the body concerned –“.
A new Clause 19 (5) is proposed –
“(5) The Department must ensure that the consultation scheme it prepares, in accordance with section 20, includes similar obligations and responsibilities to the schemes prepared by other heath and social care bodies”.
Clause 20 – Public involvement: consultation schemes
After Clause 20(1)(c), insert –
“(d) other health and social care bodies; and
(e) relevant professional groupings”.
Schedule 2
The Regional Agency for Public Helath and Social Well-Being
For paragraph 7(3), substitute – “ a person who is not a member of RAPHSW shall not, except with the approval of Department, be appointed to a committee”.
Schedule 3
The Regional Support Services Organisation (Rsso)
I note that there is no provision for the RSSO to appoint committees in a similar manner to the Regional Board or the RAPHSW. The Committee may wish to consider whether there should be equivalent provision made in this regard.
The Northern Ireland Association
for Mental Health (NIAMH)
Summary of NIAMH Response
Promoting Flourishing Mental Health in the Population of Northern Ireland
An Imperative for Government
- Mental Health Improvement and Wellbeing must be given top priority.
- The failure of Government to deliver on ‘Investing for Health’ – Mental Health Promotion Strategy 03-08, DHSSPS January 2003, means that the proposed RPHA must make this action plan one of their top priorities and take immediate action for driving it forward.
- NIAMH believe that by adopting the call in the Bamford Review for a focused, resourced, centrally driven, cross-sectoral, cross-departmental and prioritised approach we will begin to achieve the goal of improved mental health for all and create a more flourishing society.
- The vital importance of the proposed RPHA creating better inter-sectoral working across Government to tackle health promotion and health inequalities.
- NIAMH are of the view that the role of the proposed RPHA should be more than the prevention of clinically diagnosable illness but also the promotion of positive mental wellbeing and flourishing mental health.
- A Regional Health Improvement Framework must take cognizance of the Mental Health Improvement and Wellbeing recommendations as set out in the Bamford Review for comprehensive delivery at regional and local level.
- Local Commissioning Groups (LCGs) could be solely service driven to the detriment of the strategic recommendations for mental health improvement and wellbeing as set out in the Bamford Review of Mental Health and Learning Disability.
Section 3: Proposed Model and Timescales
The Northern Ireland Association for Mental Health (NIAMH) welcomes the establishment of both a Regional Health and Social Care Board (RHSCB) (3.2., page 12[1]) and a Regional Public Health Agency (RPHA) which is centrally driven with a cross-sectoral approach to tackle health promotion (3.3., bullet point 5, page 13).
We however have some reservations as to how Local Commissioning Groups (LCGs) will translate a regional strategy for delivery at local level. In particular, we have concerns that the LCGs could be solely service driven to the detriment of the strategic recommendations for mental health improvement and wellbeing as set out in the Bamford Review of Mental Health and Learning Disability.
The Minister for Health has indicated that the RHSCB would oversee the implementation of the Bamford Report (2007) ‘which will ensure much needed improvement in mental health and learning disability services’. (4.4.1., Page 16).
NIAMH are of the view that the proposed RHSCB and RPHA must make mental health improvement and well-being a top priority, to embrace the mental health promotion agenda as recommended by Bamford and ensure its delivery.
Section 7: Public Health (7.1.)
At the Heart of Government
The Northern Ireland Association for Mental Health welcomes the
Minister’s proposals to put the Public Health Agenda, which includes Mental Health Promotion, at the heart of the Health and Social Care System (7.1., page31).
This echoes the message of the Bamford Review of Mental Health and Learning Disability with regard to Mental Health Promotion where the Expert Working Committee on Mental Health Improvement and Well-Being – A Personal, Public and Political Issue, recommended:
‘The Creation of a Regional Mental Health Promotion Directorate at the Heart of Government’.
(May 2006, Ch 7, page 81 (Primary Recommendation).
Regional Public Health Agency (7.2- 7.4.)
A multi-professional focus
NIAMH espouse the view that the RPHA, in seeking to maintain a multi-professional focus, must ensure that experts from the mental health promotion field are employed to take forward the Bamford recommendations. Such input will hopefully ensure that commissioning is not solely service driven (7.3., Page 30).
(Friedli. L. and Parsonage. M, (2007) Mental Health Promotion: Building the Economic Case. NIAMH. The cost of mental illness to the NI Economy: £3.5 Billion 06/07 figures).
Health Improvement (7.5.- 7.12)
Mental Health – A public Health Issue
The Northern Ireland Association for Mental Health (NIAMH) welcomes the Minister’s emphases in the consultation Document that mental health will be seen as a public health issue (7.5, page 32).
Mental health and lower suicide rates
We also welcome the Minister’s commitment to ensuring that there is a coordinated and consistent approach to tackling the key public health challenges particularly improved mental health and lowering suicide rates through the mechanism of the proposed RPHA (7.7.5., Page 32).
The proposal for the new RPHA to provide public health programmes and initiatives designed within a common regional health improvement framework (7.6., page 32) must however take cognizance of the Mental Health Improvement and Well-Being recommendations as set out in the Bamford Review for comprehensive delivery at regional and local level.
NIAMH believe that giving top priority to mental health improvement and well-being strategies will lead to flourishing mental health across society and will be a necessary factor in reducing suicide rates.
Building a ‘flourishing society’ is contingent on viewing mental health as not merely the absence of illness, but the presence of health, that is, a state of well-being in which the individual realises his or her own abilities, can cope with the normal stresses of life, can work productively and fruitfully and is able to make a contribution to his or her community. Research has shown that the majority of people in the population experience moderate only mental health. Is it by improving the mental well-being of the whole population from moderate mental health to flourishing mental health that our common goals will be realised.[2]
Cross-sectoral Approach
NIAMH also welcome the Minister’s emphases on what we see as the vital importance of the new RPHA in creating better inter-sectoral working across Government to tackle health promotion and inequalities (3.2., page 13) in conjunction with the Ministerial Group on Public Health, where public health will be at the centre of policy and strategy (7.11., Page 34., 7.1., page 31).
Again this approach to health promotion is in keeping with the Bamford Review, where the vision of how best to promote positive mental health for the whole of society requires ‘a focused, resourced, centrally driven, cross-sectoral, cross-departmental and prioritised approach’. (Mental Health Improvement and Well-Being Report. May 2006. Executive Summary, Section 4, page iii).
Investing for Health - Mental Health Promotion Strategy 03-08, DHSSPS January 2003
HPA
Whilst NIAMH acknowledges the recent work being done by HPA on mental health promotion there continues to be a distinct lack of action in delivering on the Investing for Health - Mental Health Promotion Strategy 03-08, DHSSPS January 2003.
NIAMH do however welcome the proposed centralised position of the RPHA to fulfil an enhanced role in health improvement incorporating the responsibilities of the HPA and other Agencies. (7.10., Page 33).
The failure of Government to deliver on Investing for Health - Mental Health Promotion Strategy 03-08, DHSSPS January 2003 means that the proposed RPHA must make this action plan one of their top priorities and take immediate action for driving it forward.
Health Protection (7.13-7.16)
No Comment
Public Health Support to Commissioning and Policy Development (7.17-7.19)
Prevention and Promotion
NIAMH are of the view that the proposals for Health and Social Care Reform do present a major opportunity to have commissioning that focuses on promoting health and well-being, to which will forward a positive mental health strategy. (7.17 – 7.19. page 35, 36., 7.2. Page 31., 4.3., Page 17).
We believe that by adopting the call in the Bamford Review for a focused, resourced, centrally driven, cross-sectoral, cross-departmental and prioritised approach we begin to achieve the goal of improved mental health for all and create a more flourishing society.
NIAMH are of the view that the role of the proposed RPHA should be more than the prevention of clinically diagnosable mental illness but also the promotion of positive mental health and wellbeing and flourishing mental health. We look forward to the outworking of the Proposals and working with the new RPHA to develop and role out the mental health promotion agenda for the wellbeing of all our citizens.
[1] Page references refer to the unabridged proposal document which can be downloaded from the DHSSPS web site.
[2] Ref: Prof Corey Keyes, Mental Health is a complete state and not merely the absence of mental illness symptoms or diagnoses. 2008, Emory University USA.
Northern Ireland Commissioner
for Children and Young People
NICCY has responded to previous consultations regarding the new Health and Social Services structures that will be created under RPA. In all of our responses we have been consistent in stating that any new legislation should outline clear accountability structures for the delivery of services, in particular for the planning and delivery of services to children and young people. The current legislation does not clearly outline lines of accountability between the various bodies for service planning and delivery, I therefore recommend the legislation explicitly outlines the role of each body in relation to service planning and delivery and to whom they are accountable to in exercising this function.
I am concerned that legislation does not outline who will have the current statutory responsibility for children’s services planning. I believe it is essential that the role and function of the children and young peoples committees continues post RPA to ensure service planning is integrated and all relevant agencies work together to plan and deliver children’s services. I recommend that the legislation is amended to outline what body will have statutory responsible for the children’s services planning.
I believe strong consideration must be given to creating appropriate structures which will allow children and young people to have a specific role in planning and delivering services, which they may need. As you may know Article 12 of the United Nations Convention on the Rights of the Child states that, children should have a say in decisions that affect their lives. Involving them in planning and delivering services, will make sure services are better designed to meet current and future needs. I recommend the creation of young people led planning groups at both commissioning and delivery level within the proposed structures.
While I welcome the role and remit of the Local Commissioning Groups (LCGs) in planning services, to meet the needs of the local areas, I remain concerned that this may result in the development of a post code lottery in how services are provided, whereby services are available in one area and not in another. I recommend that the Regional Board should have a role in ensuring that services are accessible to everyone regardless of where they live.
I welcome the increased function of the Patient Client Council (PCC) regarding assisting patients wishing to make a complaint. It is essential that the PCC has appropriate resources, to provide information, to patients to ensure that they know how to access the service; while this cannot be addressed through the current legislation, NICCY would encourage the committee to highlight this issue throughout the RPA process.
Health Promotion Agency
The HPA welcomes the opportunity to comment. The HPA wishes to see the establishment of a fully integrated approach to public health issues, and the mechanisms and structures through which this is supported will be crucial to future effectiveness.
As per your letter (7 July 2008) I have restricted our response to specific clauses with alternative/additional wording where appropriate.
The HPA has comments as follows:
Page 8, clause 8, part (3) Functions of the Regional Board
The meaning of ‘due regard’ is not clear -there is a need to ensure that the input into the commissioning process from the RAPHSW will have the effect and impact that is expected i.e. that “improving the health and wellbeing of the population is put at the heart of commissioning”. We are uncertain if the wording as it stands is sufficiently robust to ensure this objective is met. This clause should reflect an ‘obligation’ on the Board to comply with such advice or information or give clear reason why this course is not followed so that accountability for subsequent actions is clear.
This comment also applies to page 9, clause 9, part (4b) Local Commissioning Groups.
Page 11, clause 13, part 2 Functions of RAPHSW
We would reword this part as we feel it does not represent the incorporation of the HPA functions into the RAPHSW as stated by the Minister.
We feel there is no need to separate out these functions from health Improvement, and have therefore sought to incorporate these functions in the wording as follows:
The health improvement functions are:
Developing and providing, or securing the provision of, programmes and initiatives designed to secure the improvement of the health and social well-being of, and reduce health inequalities between, people in Northern Ireland.
This function includes all of the constituent elements of health promotion including policy development and advice to DHSSPS on matters relating to health promotion; training; research and evaluation in relation to health promotion; development and implementation of health communications including the provision of information for the public and for professionals; the provision of a regional centre of information and advice on health promotion; and health promotion activity to support health development in specific settings and in relation to specific health issues.
Page 12, clause 13, part (4a)
We would reword this as ‘engage in or commission research and evaluation’
Page 12, clause 13, part (6a)
As it is important that the link between public health and other regional functions in tackling the wider determinants of health is strong, there is a need to ensure a public health component into regional programmes e.g. transport, regeneration and the environment. This highlights the crucial importance of effective partnerships and joint action.
We would therefore reword this as:
‘must engage with, co-operate with and when appropriate work in partnership with other bodies and organisations, including other government departments and agencies, which exercise functions relating to health improvement or health protection’.
Age Concern
1.0 Background
Age Concern Northern Ireland (ACNI) is a major voluntary organisation committed through campaigning and service provision to promoting the rights of all older people as active, involved and equal citizens. We act as a Northern Ireland-wide campaigning body and support a network of local Age Concern Groups operating throughout Northern Ireland.
2.0 General
ACNI welcomes the opportunity to give evidence on the health and social care (reform) bill. We responded to the initial RPA reforms and the proposals on the reform of health and social care earlier this year. We broadly welcome the changes to health and social care and have commented on clauses only where we seek greater clarity.
3.0 Clauses
3.1 Clause 1
ACNI understands the rationale for the changes in the current structures; we hope that chances will not have an adverse impact on frontline budgets.
3.2 Clauses 2-4
ACNI agrees with the general powers and duties as outlined. However, we still have concerns about the structure of local commissioning groups, including the issue of representation and the relationship between the local commissioning groups and the Regional Health and Social Care Board. Our concerns also remain on the relationship between the various bodies. We would seek a commissioning process that avoids a top-down approach.
3.3 Clause 8
ACNI would seek the inclusion of locality-based commissioning.
3.4 Clause 22
ACNI had concerns about the use of private finance initiatives within the health service, particularly in relation to the costs to the NHS and potential adverse impact on service provision, patients and clients.
3.5 Clause 25
As per our response to the initial reform proposals, we wish to see enshrined in legislation that core requirements must be fulfilled to ensure that the functions of the Mental Health Commission are fully met. We would also support strengthening the enforcement powers of the Mental Health Commission.
The British Medical Association
Introduction
1. The British Medical Association
1.1 The British Medical Association, or BMA, is the professional organisation and trade union for doctors in the UK. Across the UK more than three out of four practising doctors, and the majority of medical students, are members.
1.2 The BMA is the voice of the medical profession - putting across to politicians, the public and the press the profession’s collective views on a wide range of subjects including public health, medical ethics and the state of the NHS.
1.3 The BMA in Northern Ireland, or BMA(NI), supports over 4,000 members from every branch of the medical profession in Northern Ireland.
1.4 The BMA represents consultants, general practitioners, staff and associate specialists, junior doctors, public health doctors and medical academics, and medical students. The BMA has a committee to work on behalf of the interests of each of these branches of practice with a Council to represent all the branches of practice in a single entity.
1.5 The BMA is the only recognised trade union for doctors able to negotiate on their behalf with government in relation to contracts and terms and conditions. In addition the BMA produces a wide range of policies from public health issues to medical ethics, and from the state of the health service to doctors’ contracts. Its policies are decided by elected members, mainly practising doctors, and is supported by a professional staff
1.6 The BMA also produces a wide range of publications on health issues including the British Medical Journal.
1.7 The BMA believes in a Health Service that is free at the point of delivery; is centrally planned; is adequately funded; provides equality of access regardless of locality or income; is based exclusively on clinical priority; provides an equal standard of care to all; ensures equality of health outcome; and does not discriminate in terms of race, age, disability or religion
1.8 The BMA is a voluntary professional association of doctors, speaks for doctors at home and abroad, provides services for its members, is an independent trade union, is a scientific and educational body, is a publisher, and is a limited company, funded largely by its members.
Committee Stage: Health and Social Care (Reform) Bill
2. Summary
2.1 The BMA(NI) welcomes the Health, Social Services and Public Safety Statutory Committee inquiry into Health and Social Care (Reform) Bill.
2.2 The BMA(NI) has responded to a number of consultations since the Review of Public Administration began in 2002 and welcomes any reforms that will support frontline services to deliver high quality patient care. The enactment of the Health and Social Care (Reform) Bill will complete the largest part of the reform of Northern Ireland’s health service.
2.3 The BMA(NI) firmly believes that any reform must ensure that the health service is professionally led and patient centred.
The Health and Social Care (Reform) Bill
3. Clause 1
3.1 The BMA(NI) understands the dissolution of current structures are to facilitate the creation of the new ones.
3.2 This must not impact on frontline budgets.
4. Clause 2
4.1 The BMA(NI) agrees with the Department’s general duties.
4.2 A truly integrated system, as set out in Clause 2 (1), is an appropriate objective and the BMA(NI) welcomes clause 2 (3) in setting out how the Department intends to do this at the strategic level.
4.3 The BMA(NI) hopes that the leadership of the medical profession will be closely involved at this level.
5. Clause 3
5.1 The BMA(NI) agrees with Clause 3.
5.2 The BMA(NI) notes that, in combination with Clause 2, commissioning will play a very important role and that commissioning should be led from the local community upwards.
5.3 There is a concern amongst medical professionals that commissioning is part of a top down approach, when it should be a bottom up approach in order to reflect local needs.
6. Clause 4
6.1 The BMA(NI) welcomes the Department putting consultation at the core of its priorities and objectives. However, this must be meaningful consultation and not just going through the motions on a decision that has already been taken.
6.2 The BMA(NI) would suggest an amendment to clause 4,
“(4) If the Department acts under subsection (3), then the Department must consult such bodies or persons as it thinks appropriate not more than 6 months on the determination or revision of such priorities or objectives”.
7. Clause 5
7.1 The BMA(NI) welcomes this clause.
8. Clause 6
8.1 The BMA(NI) suggests that an amendment be made to clause 6.
“(5) If the Department acts under subsection (3), then the Department must consult the body or bodies affected not more than 6 months from when such direction or directions were given.
(6) Subsection (1) does not affect the Department’s own powers to give directions apart from this section.”
9. Clause 7
9.1 The BMA(NI) welcomes this clause as it dissolves the four Health and Social Care Boards and creates one Regional Health and Social Care Board in their place.
9.2 However, the BMA(NI) would still have concerns about how each section will communicate with each other in such a large organisation.
10. Clause 8
10.1 The BMA(NI) welcomes the emphasis on the responsibility of the Regional Health and Social Care Board (RHSCB) for managing the performance of HSC Trusts, commissioning, and how resources are best used as set out in Clause 8 (2) (b).
10.2 The BMA(NI) would contend that under Clause 8 (3) the RHSCB should look to how the process of commissioning, within the commissioning plan, can best be accomplished from the bottom up with the inclusion of locality based commissioning.
11. Clause 9
11.1 The BMA(NI) welcomes Clause 9.
11.2 In conjunction with Paragraph 7 of Schedule 1, there is little given to the actual membership of the Local Commissioning Groups.
11.3 The BMA(NI) disagrees with the proposal, outwith this Bill, that commissioning should be a ‘democratic’ process, as proposed by the Minister in his speech to the Chamber on 4th February 2008. Healthcare commissioning is about assessing need, and prioritising and commissioning according to need, not democracy.
11.4 The BMA(NI) continues to be concerned about the proposal that local councillors should be included in the commissioning process. There is firm agreement that accountability must be part of the reform, however the BMA(NI) believes there is a difference in operation between organisational accountability and democratic accountability.
11.5 The BMA(NI) believes that the consultation process on either the Board or the Department giving directions or revision of priorities or objectives with regard to the commissioning of healthcare must include the Local Commissioning Groups.
11.6 Again the BMA(NI) would raise the issue of the need for a bottom-up approach to commissioning rather than top-down.
12. Clause 10
12.1 The BMA(NI) welcomes Clause 10.
12.2 The BMA(NI) believes that before the RHSCB gives any direction of a general or specific nature, as stated in Clause 10 (1) it must engage with the Local Negotiating Committee to ensure such directions can be implemented.
13. Clause 11
13.1 The BMA(NI) welcomes Clause 11.
13.2 The BMA(NI) believes that the reporting structures, while essential to the process of improving services, should be, at the direction of the RHSCB, consistent across Northern Ireland and should not reduce the time hospital doctors have to treat patients.
13.3 It must be pointed out that hospital doctors may not have their protected time within direct clinical care or may have their time for professional development interfered with. An increase in medical secretarial staff would help facilitate the smooth running of information gathering.
14. Clauses 12 & 13
14.1 The BMA(NI) welcomes Clauses 12 and 13.
14.2 The BMA(NI) welcomes the emphasis on public health and social well being and believes that this is in keeping with the health service working with wider society to promote a holistic approach to maintaining a healthy lifestyle.
14.3 There is an opportunity with this new Regional Agency for Public Health and Social Well being to work with other Departments and Agencies to further the aims of the Department as set out in Clause (2).
15. Clauses 14 & 15
15.1 The BMA(NI) cautiously welcomes Clauses 14 and 15.
15.2 The reorganisation of the health services seems to follow the general trend of Executive Departments as a whole to centralise particular support functions.
15.3 Whilst this is something that can be welcomed in order to reduce unnecessary duplication of particular services, the BMA(NI) is concerned about the size and potential bureaucracy of such a large organisation, particularly against the backdrop of the RPA which was initiated to reduce bureaucracy in the HSC arena and other public sector. The BMA(NI) would want to be assured that this large organisation would be structured in a flat or horizontal form.
15.4 The layers of hierarchy in the new Regional Support Services Organisation should be minimised and the various support functions managed as overall business units within the organisation. Without such a structured approach the BMA(NI) would be concerned that the new RSSO would be too hierarchical and too bureaucratic with far too many communication needs.
15.5 The BMA(NI) would also be concerned that such a huge bureaucracy – as per other bureaucracies – could grow over time (to cope with needs regarding management, communication and internal support functions) and potentially undo much of the work that the RPA has done to eliminate unnecessary bureaucracy.
15.6 The BMA(NI) view is that one overly bureaucratic system should not be replaced with another, particularly given the cost of undertaking and implementing the RPA to date in terms of time, money, commitment and personal sacrifices, such as voluntary redundancy or voluntary early retirement.
16. Clauses 16, 17, 18, 19 & 20
16.1 The BMA(NI) welcomes Clauses 16, 17,18, 19 and 20.
16.2 The BMA(NI) believes that a single Patient and Client Council, with local offices, effectively staffed and resourced would be much more strategically effective and joined-up than four separate HSSCs.
16.3 The emphasis on inclusive consultation is welcome.
17. Clause 21
17.1 The BMA(NI) welcomes Clause 21.
18. Clause 22
18.1 The BMA(NI) is concerned with Clause 22.
18.2 The BMA(NI) is opposed to the use of Private Finance Initiatives (PFI) in the NHS and would oppose any use of this clause to pursue the use of PFI within the health service.
18.3 The BMA, in response to the Westminster Public Accounts Committee report on PFI refinancing published in May 2007, stated,
18.4 “This report confirms what the BMA has been saying for many years - that PFI is an expensive way of borrowing money which stores up debts for the future and drains funds away from the NHS into the pockets of the private investors. We can see just how damaging this is as so many NHS trusts are currently crippled with debts and are struggling to meet PFI repayments. This is already directly affecting patient care.
18.5 It is appalling that the government let these negotiations go ahead allowing the private sector to fleece the NHS. Such huge scale financial projects should have been managed to get the best deals for the NHS, patients and for taxpayers. We warned the government that this would happen and they are reaping the consequences.
18.6 The BMA will be urging the new cabinet to move away from wasting large sums of money in private sector deals which have been shown to offer poor value and can leave hospitals heavily in debt for decades. Private companies may have done very well out of them but the NHS and therefore patients have not.”
18.7 However, it must also be noted that Clause 22 is very vague in what is referred to as public private partnerships. This clause requires further clarification.
19. Clauses 23 to 28
19.1 The BMA(NI) believes that the process of dissolution and transfer should be properly planned with open communication with the staff involved to ensure a smooth implementation.
19.2 The BMA(NI) is concerned about Clause 25, the transfer of the Mental Health Commission to the Health and Social Care Regulation and Quality Improvement Authority. This concern is purely on the issue of staffing and training. The functions of both organisations, within the new amalgamated context, must not be allowed to deteriorate.
20. Clauses 29 to 35
20.1 The Clauses seem to be in order.
20.2 The BMA(NI) welcomes the emphasis on public health and social well being and believes that this is in keeping with the health service working with wider society to promote a holistic approach to maintaining a healthy lifestyle.
20.3 There is an opportunity with this new Regional Agency for Public Health and Social Well being to work with other Departments and Agencies to further the aims of the Department as set out in Clause (2).
21. Schedules
21.1 The BMA(NI) has no comment on the schedules at the moment.
22. Conclusion
22.1 The BMA(NI) generally welcomes the progression of Phase 2 of the Review of Public Administration (RPA) in health as it has the potential to improve the lives of many people in Northern Ireland via a more efficient and less bureaucratic healthcare system, by the consequent release of resources to frontline patient care.
22.2 The BMA(NI) is very concerned about the top-down approach to managing commissioning and believes an opportunity may be lost to create local community based commissioning arrangements, at the level of groups of GP practices or individual practice level.
22.3 The Regional Health and Social Care Board (RHSCB) is welcome.
22.4 The BMA(NI) supports the slimming down of the Department of Health Social Services and Public Safety Northern Ireland (DHSSPSNI) and looks forward to savings from a reduction in bureaucracy being released to frontline patient care. It is essential that such savings are audited and that the Department communicates with HSC organisations and stakeholders on how these savings will be redistributed to frontline patient care. This must be a transparent process.
22.5 The BMA(NI) welcomes, with reservations, the creation of the new Regional Support Services Organisation (RSSO). The size and bureaucracy of this support function is a concern. The BMA(NI) would hope that this huge bureaucracy is structured in a way that is ‘flat’ and ‘divisionalised’, that is to say there should be a streamlined hierarchy with only a few managers. The provision of any out sourcing of work must be subject to the application of stringent business cases and progressed in a transparent and open manner.
22.6 The proposed Regional Agency for Public Health and Social Wellbeing (RAPHSW) and the priority given to public health in the new structures are welcomed in principle. It is vital that the role and functions of public health doctors are enhanced and backed up by the necessary staffing levels and support. The RAPHSW will need to interface significantly with the Department, the RHSCB, the RSSO and Trusts. It is essential that bureaucracy is minimised within the RAPHSW and between such organisations
22.7 The BMA(NI) welcomes the single Patient and Client Council (PCC) which should be effectively resourced, in terms of role, personnel and finance. The need for added local offices should be subject to a full business case but it would be useful if the PCC had local offices in each of the new Trust geographic areas. The BMA(NI) had suggested in its consultation response that some consideration be given, in terms of independence, of the PCC coming under the organisational umbrella of another organisation e.g. Northern Ireland Consumer Council.
22.8 The BMA(NI) has a major concern over the top-down approach to managing commissioning and believes that an opportunity may be lost to create local community based commissioning arrangements, at the level of groups of GP practices or individual practice level.
22.9 Commissioning is about assessing, prioritising and commissioning according to clinical need. It must be evidence based and decisions taken by those with the appropriate level of expertise.
22.10 The BMA(NI) strongly believes that any commissioning body that wishes to have general practitioner involvement must have the freedom to place or move contracts and be free to commission services as long as they operate within the regional strategic framework.
22.11 The BMA(NI), and its General Practitioner Committee, is of the opinion that elected local representatives should not be included on Local Commissioning Groups. This is not to minimise the importance of elected local representatives as the BMA(NI) fully supports the principle that Local Commissioning Groups and local government should work jointly on local health improvement plans. The BMA(NI) believes that the strong scrutiny and accountability role of Local Councils, working alongside the new PCC, may be eroded if elected council representatives are on the LCGs. There is also a concern regarding the practicality of having four local representatives on each LCG. If for instance the Northern Trust has one LCG it will cover eight current local government areas.
The Northern Ireland Confederation
for Health and Social Services
1. Introduction
The Northern Ireland Confederation for Health and Social Services is the voice of management in the integrated Health and Personal Social Services (HPSS). Part of the UK-wide NHS Confederation, it is the only membership body for all HPSS organisations. At present, the membership includes the HSS Boards and Trusts, the Central Services Agency and five of the smaller HPSS bodies.
2. Proposals for Health and Social Care Reform
The Confederation has always supported the need to reform and to streamline the HPSS structures to deliver a more efficient and focused system. We welcomed the consultation document issued by the Minister for Health, Social Services and Public Safety on 18 February 2008 and a copy of our response is submitted for the information of the Committee.
The Confederation appreciates the opportunity to submit views with regard to the Health and Social Care (Reform) Bill. We consider that the provisions of the Bill set out an appropriate legislative framework that will support the necessary structural changes. We recognise that much of the detail will be covered by subsequent subordinate legislation and therefore consider that there must be full consultation on all regulations arising if and when the Bill completes its passage through the Assembly. There are a few specific points that we would wish to make on the Bill and these are set out below.
3. Governance and Accountability
Sections 7(1), 12(1), 14(1) and 16(1) establish the Regional Health and Social Care Board (Regional Board), the Regional Agency for Public Health and Well-being (RAPHSW), the Regional Support Services Organisation (RSSO) and the Patient and Client Council (PCC) as corporate bodies. Section 5 requires the Department to prepare a framework document for each organization within the Health and Social Care (HSC) system, which will define the relationships between it and the Department and with other HSC bodies. It is considered essential that there are clear established lines of governance and accountability between all of the organisations in the HSC system. We see the Minister as responsible to the Assembly, the Department responsible to the Minister, and the Regional Board, RAPHSW, RSSO and the PCC directly responsible to the Department. In our response to the earlier consultation, we highlighted the need to clarify what the Accountable Officer relationship was between the
HSC Trust Chief Executives and the Permanent Secretary. This applies to any chief officer and reinforces the need for clear lines of accountability to be set out in the Bill.
4. Commissioning Responsibilities
The Confederation considers that there must be clarity in the responsibility for commissioning. Section 8 sets out responsibilities for the Regional Board but in Section 8(3) the Regional Board must have “due regard to any advice or information provided by” RAPHSW. Also, in Section 9, responsibilities are given to the Local Commissioning Groups for planning, commissioning and securing services with again having due regard to RPHSW advice and information. While welcoming a role for the RAPHSW being enshrined in legislation, the Confederation considers that the Regional Board must have primacy in terms of the commissioning plan and this should be reflected in the Bill.
5. Political Representation and Appointments
The Confederation supported the involvement of local government representatives but highlighted possible difficulties, such as the potential conflict of Councillors holding more than one post within the HSC system. Schedule 2, paragraph 3(1)(f) provides for the RAPHSW Board to include “a prescribed number of members of district councils appointed by the Department in such a manner as may be prescribed”. In paragraph 3(3), the exclusion of RAPHSW officers does not apply to district council members and the Confederation considers that this should be rectified by changing the sub-paragraph to read “…..no person who is an officer of RAPHSW may be appointed under sub-paragraph (1)(a), (b) or (f)”.
In Schedule 2 paragraph 5 (Term of office), in sub-paragraph (1) district council members are appointed with the same term of office as others and in sub-paragraph (4) the period of office terminates if the member “ceases to be a member of a district council”. We wonder whether this should be “the district council”, that is the district council of which the RAPHSW member was a member when appointed. However, in Schedule 2 paragraph 6 (Resignation and removal) district council members are not included in paragraph 6(1) which provides for the resignation of an RAPHSW member or for the removal of a member by the Department.
The Confederation welcomed the assurance in the consultation document that the merit principle would underpin the selection process and we consider that all all appointments should be in accordance with the OCPA Code of Practice. It is imperative that this is applied to all RAPHSW members in order to ensure consistency and to embed the corporacy of the RAPHSW Board as a whole. Accordingly, the Confederation considers that paragraph 6(1) should be extended to include district council members and this would require a similar change to paragraph 6(5).
Section 9(6)(a) provides for the regulations that will set out the membership of Local Commissioning Groups and we consider that our views above should be taken into account in the preparation of those regulations.
6. Conclusion
The Confederation considers that the provisions of the Bill set out an appropriate legislative framework that will support the necessary structural changes. There is a need to ensure that the HSC system is fit for purpose, delivers high quality outcomes and that the organisational strucure is efficient and effective. We have highlighted a few areas in which we consider further thought is required.
If the Committee would like any clarification etc on any of the issues covered in our submission, we will be most happy to provide same.
Optometry NI
1. Introduction:-
1.1 Optometry NI represent all Optometrists, Dispensing Opticians and bodies corporate, working in Northern Ireland.
1.2 Our ambition is to re-negotiate our GOS contract to enable Optometrists to function to their full potential, in a primary care setting, thereby easing the burden on Hospital Eye Services, and allowing patients to be seen (where clinically appropriate) in their local community.
1.3 We would like to ask the committee to explore the possibility of using the Health and Social Care Bill to accelerate the process of implementing this initiative.
1.4 To this end our committee has been having discussions with the Department of Health and allied professions. We now have a package of detailed measures and proposals, including a business plan. This means we are in a position, with the agreement of the minister and the support of the Health Committee, to implement these changes.
2. Specific comments on the Bill and proposals for change:-
2.1 Local commissioning groups.
The proposal to include a range of primary care practitioners on the LCGs is welcomed. Optometry NI recognises the need for the promotion of health and well-being.
To be effective, commissioning by LCGs will need to encourage and facilitate engagement at a much more local level, between primary care and local users and carers.
Optometry NI would like to emphasise the need for recognition of the scope of practice of Optometrists and Dentists. Both professions are unique, and have an important contribution to make to the commissioning of local services. Optometrists and Dentists are closely engaged with their local communities, both offering front-line primary care to local people, providing them with understanding and knowledge of local need.
In summary, Optometry NI feels active involvement of multi-disciplinary primary care practitioners in service re-design is essential if change is to be effective. There should therefore be representation from both professions on the LCGs as of right rather than a shared seat.
3. Further information
3.1 We would be delighted to talk to members of the Health Committee on these issues. In the first instance please contact Alan Rundle, Chairman of Optometry NI, PO Box 28, Dromore BT25 1YH.
NCH Northern Ireland
Introductory Remarks
1. NCH welcomes the opportunity to respond with written comments to the Health, Social Services and Public Safety Committee’s consideration of the Health and Social Care (Reform) Bill.
2. NCH is a major provider of services to vulnerable children and young people and their families and invested considerably in children’s service planning in Northern Ireland. We therefore have an active interest in the reform process responded to the Department’s consultation on its Health and Social Care Reform Proposals in May 2008[1]. We would be happy to provide any further evidence/input to the Committee as it takes forward its consideration of the Reform Bill.
3. We have provided some information below about NCH and some general comments of relevance to the proposed reforms arising from the previous consultation and the Minister’s subsequent announcement (1st July 2008).
About NCH
4. NCH is one of the UK’s leading children’s charities, helping children achieve their full potential. Through our services we support some of the UK’s most vulnerable and excluded children and young people and facing difficulties such as poverty, disability and abuse. We believe all children and young people have unique potential and that they should have the support and opportunities they need to reach it.
5. Across the UK we run more than 500 projects supporting over 173,000 of the most vulnerable and excluded children and young people, and their families. Through our work and through speaking out, we seek to break the cycle of deprivation, challenge injustice and empower children to overcome the obstacles in their lives that hold them back. We tailor our work to local circumstances, in partnership with children and young people, families, communities and local organisations. We work with children and young people:
- whose families need support
- who cannot live with their birth families
- who are disabled
- who experience severe difficulties in their lives
6. In addition to the £1.6 million already invested in Northern Ireland, NCH plans to invest a further £1.4m in developing and providing services for vulnerable children, young people and families across Northern Ireland. Working closely with children’s services planning processes across the statutory, voluntary and community sectors, we currently provide services to almost 3,900 children, young people and their families in Northern Ireland with services. We currently have 14 developments in each of the current four Health and Social Services Board areas:
- 4 Sure Start linked projects - in Downpatrick, Larne/Carrick, Waterside and Ballymena ;
- Larne Parental Support Project, Locality Planning and Coordination of an Early Intervention Project for Youth Offending in the Northern Board area;
- Early Intervention Family Support (Local Action Planning Groups), Clooney Family Centre, Chance for Change Project and Mentoring Services 5-11 year olds and Floating Support services for care leavers and young homeless in the Western Board area;
- Regional Young Carers provision in partnership with Barnardos with NCH leading in the Eastern and Southern Board areas and;
- A Regional Fostering Service in Northern Ireland.
7. We employ around 100 staff with a range of professional backgrounds including Social Work, Education, Health, Nursing, Youth Work, Social Care and Early Years.
General Comments
8. We welcome the Minister’s announcement[2] on his decisions on the way forward confirming that improving social care with have equal importance to improving health and well-being and that existing statutory responsibility for children’s services planning will become the responsibility of the new Regional Health and Social Care Board. We welcome his intention to consider proposals for strengthening and building upon the children’s services planning process through introducing legislation.
9. We trust this will be based on an appropriate statutory duty to cooperate and the drafting of the necessary legislation and guidance covering this provision and ‘duty to cooperate’ will be taken forward as soon. We would ask the Committee to ensure that any mechanism set up to achieve these will recognise and include representatives of the community / voluntary sector who have played such an active role in supporting the development of children’s services planning processes to date in Northern Ireland. We note in other jurisdictions of the UK similar recognition has been given to the voluntary sector and included in legislation[3].
10. We note that the Reform Bill (at section 8) deals with the functions of the new Regional Board and (section 24) addresses the transfer of statutory functions of the Health and Social Services Boards to the new Regional Board. We trust therefore that section 24 (2) will encompass and address the transfer of statutory responsibility for children’s services planning from the four HSSBs to the new regional body.
11. However, NCH would request that the Committee seek to confirm that responsibility for children services planning will indeed be transferred to the regional body under section 24 (2) and is one of the functions of the new Regional Board under section 8.
12. NCH strongly supports the four HSSB Children and Young People’s Committees proposals to enhance and further develop the planning and commissioning process by addressing ‘major deficits’ inherent in the current process[4]. These proposals include integrating children’s service planning with UNCRC guiding principles and a children’s rights framework which the Department has signed up to through the cross government 10 Year Children and Young People’s Strategy.
13. NCH would, therefore, request that the Committee consider and endorse these proposals to the Minister as the way ahead for the future planning and commissioning of children’s services and seek to integrate these within the current H&SC reform process.
14. In line with the UNCRC Article 12, NCH believes that children and young people must be given the opportunity to be heard and that their views are given due weight and consideration at all levels in the planning and commissioning of children’s services.
Concluding Remarks
15. NCH wish the Committee well in their forthcoming deliberations and would re-iterate that we would be happy to provide any further evidence/input to the Committee as it takes forward its consideration of the Reform Bill. As active members of Children in Northern Ireland (CiNI), NCH endorse the comments sent by to the Committee including those on the specific sections of the Reform Bill.
[1] www.dhsspsni.gov.uk/62-nch_northern_ireland.pdf
[2] Ministerial Announcement 1st July 2008
[3] Children Act 2004 http://www.opsi.gov.uk/acts/acts2004/ukpga_20040031_en_3#pt2-pb1-l1g10
[4]HSSB Children and Young People’s Committees, ‘A Joint Planning and Commissioning Framework to Improve Outcomes for Children and Young People’ p.4
South Eastern Health
and Social Care Trust
South Eastern Health and Social Care Trust values the opportunity given by the Northern Ireland Assembly Committee for Health, Social Services and Public Safety to make a submission in respect of the Health and Social Care (Reform) Bill, which was formally introduced to the Assembly on 23 June 2008 and received its second reading on 1 July 2008. The Trust is cognisant that the implementation of the proposals detailed in the Bill has the potential to totally transform the constitution, purpose and relationships of health and social care bodies now and in the future.
The Trust is supportive of the objectives of the reform process, in creating a modern and responsive health and social care service, which is both patient-centred and efficient. The Trust has considered the details of the structures, duties and functions of the organisations cited in the proposed primary legislation and would be broadly of the view that the proposals detailed espouse the guiding principles developed by the Minister and Department, which have come to underpin the reform process.
The Trust had indicated in its earlier responses to previous Reform Consultation Papers released by the Department, namely:
1. “Proposals for Health & Social Care Reform (February 2008); and
2. “Transformation of Business Services in Health and Social Care - Shared Services” (September 2007).
the elements which the Trust considered to be conducive to the process of reforming structures and organisational relationships across the service. Many of the queries articulated there-in have now been addressed and the Trust is proposing minor revisions and clarifications to the Health and Social Care (Reform) Bill. These suggested inclusions pertain to two distinct Clauses of the proposed legislation:
- “Power of the Regional Board to give directions and guidance to HSC trusts (Clause 10); and
- Provision of information, etc. to Regional Board by HSC trusts (Clause 11).”
Inclusions to the primary legislation:
In respect of Clause 10, the Trust would suggest the following insertion to the wording:
“10. – (1) The Regional Board may give directions, when necessary, of a general or specific nature to an HSC trust as to the carrying out by that trust of any of its functions.”
In making this addition to Clause 10, the Trust has assumed that other previous legislation empowering the DHSSPS to instruct remains extant. If this is not the case there is a need to reflect this in the requirement to make this provision. The Trust considers the term ‘when necessary’ to have a meaning reflecting ‘an unusual event’, and such ‘directions’ would then constitute an ‘instruction’ by the Regional Board.
Also in relation to Clause 11, the Trust would suggest the following insertion to the wording:
“11. -(2) After paragraph 6 insert –
“6A.- (1) An HSC trust shall be the owner of information and shall record such information with respect to the exercise of its functions as the Regional Board may direct.””
The Trust contends that in order for it to undertake the full range and diversity of its many functions it is necessary for the Trust to retain control the information pertaining to its purpose. Not doing so would compromise the Trust’s control of its remit, and thus potentially compromise service delivery. Therefore the Trust would seek to retain control of information generated and maintained by the Trust as part of the revised health and social care arrangements. The Regional Health and Social Care Board (RHSCB), the Regional Agency for Public Health and Social Well-being (RAPHSW), and the Regional Shared Services Organisation (RSSO), would be required to seek through normal protocols access to Trust information. The Trust believes that this inclusion to Clause 11 may obviate any requirement to change the Trust’s legal position in respect of information.
Detail and clarity:
A further suggestion that the Trust would make in respect of the functions of the RSSO would be to offer some detail or clarity in respect of:
“15. – (5) RSSO may charge for support services provided by it.”
The previous consultation paper (February 2008), suggested a particular form of charging adopted by Consultancy organisations. The Trust would suggest that the RSSO should provide a more flexible choice of charging options including hard charging, contracts and service level agreements, to support the variety of services it will be expected to deliver, to a range of different health and social care organisations. The Trust believes that such mechanisms will enable the Trust to retain appropriate control over these functions and thus ensure the quality of service provided.
Conclusion:
South Eastern Trust believes that the Health and Social Care (Reform) Bill reflects appropriate changes to the organisations with regards to functions, arrangements and relationships. These changes are to be welcomed for their ability to deliver lasting reform. Furthermore, the Trust believes the inclusions and clarifications which have been proposed in this submission will ultimately facilitate the implementation of the Health and Social Care (Reform) Bill in the delivery of a modern, responsive and forward looking health and social care service.
The Association of the
British Pharmaceutical Industry
Health and Social Care (Reform) Bill Committee Stage:
ABPI Northern Ireland (ABPI NI) submission to Northern Ireland Assembly Committee for Health, Social Services and Public Safety.
Introduction
The Association of the British Pharmaceutical Industry (ABPI) is the trade association for more than 80 companies in the UK involved in the research, development manufacture and supply of some 80% of the medicines prescribed through the NHS.
The ABPI represents the views of its member companies and maintains close regular contact with government at all levels – the UK Government, devolved governments, the European Union, and other authorities.
The Prescription Medicines Code of Practice Authority was established by the ABPI in 1993 to regulate the industry’s promotional activities under a strict Code of Practice.
The ABPI works to represent the pharmaceutical industry in the UK in a way that:
- Assures patients access to the best available medicines
- Generates a favorable political and economic climate
- Encourages innovative research and development
- Affords fair commercial returns.
ABPI Northern Ireland (ABPI NI) was setup in 2007 as the voice of the pharmaceutical industry in Northern Ireland – a regional presence for the Association of the British Pharmaceutical Industry, established in response to devolution and the changing political context.
ABPI NI represents the ABPI in addressing the distinctive health policy agenda in the region, where the specific health needs of the population are being tackled by a significant investment in health and social care by the Northern Ireland Executive.
ABPI NI submission
The proposed reforms to the health and social care system have been much debated and consulted upon. ABPI NI has previously submitted its response to the public consultation on the draft legislation.
The Health and Social Care (Reform) Bill was introduced on 23 June, had its Second Stage debate on 1 July and will progress through its Committee Stage when the Assembly returns from Recess on 1 September.
The general principles of the Bill and the overall structure of the new system have been accepted. ABPI NI believes that the focus during this stage must be on amendments to the Bill that will improve the transparency, accountability and efficiency of the new system.
Clause 2 – Departmental General Duties
Clause 2 of the Bill deals with the general duties of the Department of Health, Social Services and Public Safety. Sub Section (3) imposes specific tasks with regard to developing policies, determining priorities, allocating resources, set standards, preparing framework documents, securing the commissioning and development of programmes, etc.
ABPI NI believe consideration should be given to inserting an amendment to sub section (3) outlining a duty on the Department to require the implementation of national guidance from bodies such as the National Institute for Health and Clinical Excellence (NICE) within timescales similar to those enforced in England and Wales.
Importantly Clause 2 also imposes a duty on the Department to monitor and hold to account the various Health and Social Care Boards, agencies and bodies. ABPI NI believes that this analysis and monitoring should be provided as a matter of course (rather than upon request) to the Assembly’s Health Committee and relevant stakeholders, including commercial stakeholders.
Clause 4 – Departmental Priorities and Objectives
Sub Section (2)
The Bill leaves it to the discretion of the Department to decide who to consult with in deciding its priorities and objectives. ABPI NI believes the Health Committee should seek to amend this Sub Section to read:
Before determining or revising any priorities or objectives under this section, the Department must consult with a list of stakeholders drawn up in conjunction with the Northern Ireland Assembly Committee for Health, Social Services and Public Safety.
Clause 8 – Functions of the Regional Health and Social Care Board
In its role in overseeing HSC Trusts and their provision of services, the Regional Health and Social Care Board is charged with “ensuring that resources are used in the most economic, efficient and effective way in commissioning such care”. ABPI NI believes it is, therefore, essential that the information used by the Regional Board for such analysis are freely available to stakeholders, including commercial ones.
In order to maximise transparency, accountability and efficiency, ABPI NI believe that this Clause should be amended to make the provision of non-sensitive information regarding HSC decisions and commissioning decisions as widely available as possible. ABPI NI recommends that the following wording is added to sub section (2) (b) as point (iv):
To maximise transparency, accountability and efficiency by making available all information used in decision making processes to all stakeholders.
Clause 9 – Local Commissioning Groups
The Local Commissioning Groups (LCGs) will be important decision makers within the new system. In their efforts to secure the delivery of health and social care “that is efficient, co-ordinated and cost-effective”, the LCG’s must act in a manner that is transparent and accountable. ABPI NI believe that sub section (5) of Clause 9 should be amended by adding an additional point (e):
(e) to maximise transparency, accountability and efficiency by making available all information used in the commissioning process to all stakeholders.
Clause 13 – Functions of the Regional Agency for Public Health and Social Well-being
ABPI NI believes that the Regional Agency for Public Health and Social Well-being (RAPHSW) has the potential to be an important source of information, which should be made available to the public in order to maximise transparency and accountability. In particular, under sub section (4), RAPHSW can commission research, obtain and analyse data, etc. It is charged under Clause 13 sub section (4) point (e) with making available “to any other body such persons, materials and facilities as it thinks appropriate”. ABPI NI believes that the views of the Assembly Committee for Health, Social Services and Public should be taken into account by RAPHSW and that sub section (4) point (e) should be amended as follows:
(e) make available to any other body, after consultation with the Assembly Committee for Health, Social Services and Public Safety, such persons, materials, information and facilities as are deemed appropriate;
19. Public involvement and consultation
ABPI NI believe that it is important that information gathered by the Patient and Client Council is, whenever, possible made publicly available. This will assist the public to assess the level of provision currently being provided. It may, therefore, be necessary to seek the public provision of all non-commercially sensitive information gathered under Clause 19, Sub Section (1) (b) and to add a point (d):
To provide access to generalised and statistical information gathered under 19.1 .b to the public including patient interest groups and other stakeholder organisations.
Disability Action
Disability Action is a pioneering Northern Ireland charity working with and for people with disabilities. We work with our members to provide information, training, transport awareness programmes and representation for people regardless of their disability; whether that is physical, mental, sensory, hidden or learning disability.
More than one in five (300,000) people in Northern Ireland has a disability and over one quarter of all families here are directly affected by disability issues.
As a campaigning body, we work to bring about positive change to the social, economic and cultural life of people with disabilities and consequently our entire community. In pursuit of our aims we serve 45,000 people each year.
Our network of services is provided via our Headquarters in Belfast and in three regional offices in Carrickfergus, Derry and Dungannon.
Disability Action wishes to make the following comments on the draft Health and Social Care (Reform) Bill.
Clause 2 (3) (C)
Continued concern exists that the allocation of available expenditure between acute and community care remains unbalanced in favour of acute care. Disabled people comprise 20% of Northern Ireland’s population the vast majority of whom live in the community and avail of primarily Social Care services.
To safeguard the needs of disabled people and their families. (1 family in 4 in Northern Ireland) Disability Action advises that this clause should read:
“Allocate financial resources available for Health and Social Care, having regard to the need to use such resources in the most economic, efficient, balanced and effective way.”
If this amendment is agreed it may affect clause 4 (b) and 4 (c)
Clause 9 (6) (a)
Disability Action continues to express its concerns that service users are not directly represented on Local Commissioning Groups. We clearly recognise the need for health professionals to manage the process but the Department needs to ensure that those most directly affected by these structural changes have a voice in decisions on local provision.
Disability Action is unsure if such direct representation should be written into this clause or be provided for in regulation. If required in this clause, we advise it should read:
“Make provision for the membership of Local Commissioning Group, ensuring the direct representation of service users.”
Clause 13 (2)
Disability Action commends the comprehensiveness of clause 13 (2) (a) but believes that 13 (2) (b) should be expanded to better outline the Health promotion function.
Clause 17 (2)
Many public bodies have a duty to consult but often undertake consultation exercises in a manner which excludes or partially excludes disabled people. For that reason Disability Action advises the following wording:
“Consult the public in an accessible way about matters relating to Health and Social Care.”
Clause 17 (4)
Disability Action is unsure due to the use of the term “all reasonable requirements” if this clause is meant to refer to reasonable adjustments, under the Disability Discrimination Act, a duty which the PCC will be required to meet. If it is the latter, that should be made clear. If it is not then the clause should be clarified.
Clause 19 (1) (a)
For the reasons outlined above, Disability Action advises that this should read:
“To promulgate information, In accessible formats, about ….”
Pharmaceutical Society
of Northern Ireland
The Pharmaceutical Society of Northern Ireland recommends the Health and Social Care (Reform) Bill be amended in such a fashion as to clarify:
- the means by which the constitution of the Local Commissioning Groups will be determined; and
- the Department’s duty to prepare various kinds of legislation, including for the regulation of professionals working in the health sector.
The Society also suggest the Committee consider the merits of the Assembly Health Committee conducting Appointments Hearings for the position of Chair for the principal health bodies described in the Health and Social Care (Reform) Bill.
Local Commissioning Groups (Section 9 of the Bill)
Section 9, subsection 6:
“Regulations may… make provision for the membership of Local Commissioning Groups”
The pre-Committee stage draft of the Health and Social Care (Reform) Bill does not put into legislation the constituent membership of the Local Commissioning Groups (LCGs). Membership of Local Commissioning Groups is instead to be determined in regulation. The Society suggests the Assembly Health Committee gives the question of whether LCG membership should be stated in regulation or legislation some consideration in their scrutiny of the Bill.
The make-up of the Local Commissioning Groups was a major item of stakeholder interest in the May 2008 consultation on the Health and Social Care reform proposals. For example:
- the Pharmaceutical Society of Northern Ireland felt a case existed for two pharmacists to be members of the commissioning groups in light of the varied forms of pharmacy practice (e.g. hospital, community and specialised areas of practice such as mental health pharmacy) and the growing clinical and public health roles of the profession;
- Local Government stakeholders had particular views on the constitution of Local Commissioning Groups in relation to local councillor involvement; and.
- A number of organisations representing community and voluntary workers opposed the reduction in lay membership of the Groups from original proposals.
Section 9, subsection 7:
“Before making regulations under subsection (6), the Department must consult the Regional Board”
Given the breadth and strength of stakeholder opinion concerning the constitution of Local Commissioning Groups, in a scenario in which the membership of LCGs is laid out in regulation rather than legislation (as per the current draft of the Bill), the Pharmaceutical Society of Northern Ireland recommend this section of the Bill be reworded thus:
“Before making regulations under subsection (6), the Department must consult the Regional Board, stakeholders and the public”
Duties of the Department (Section 2 of the Bill)
Section 2 of the Health and Social Care (Reform) Bill outlines a number of general duties of the Department of Health, Social Services and Public Safety.
A key point raised by the Pharmaceutical Society of Northern Ireland in its response to the May 2008 RPA consultation was the need to create a new Department fit for the future operation of a devolved healthcare system, fully accountable to the Northern Ireland Assembly.
The Pharmaceutical Society of Northern Ireland is the regulatory body for pharmacists in Northern Ireland. Given that regulation of healthcare professionals is a devolved matter to Northern Ireland[1], the Society expressed its view in its response to the May 2008 RPA consultation that the Department should now house a dedicated unit capable of preparing timely Bills and legislative orders for passage in the Northern Ireland Assembly and, if necessary, Westminster. For example, the Society is currently working with the Department to produce a number of amending Orders to modernise the regulation of pharmacy in Northern Ireland.
Accordingly, the Society recommends to the Assembly Health Committee that the necessity of the Department preparing legislation be included within the list of general duties laid out in the Health and Social Care (Reform) Bill. The Bill should be amended thus:
Section 2, Subsection 3, after (g) insert –
(h)(a) develop and bring forward such legislation as may be required to ensure the appropriate regulation of health professionals in Northern Ireland.
The possibility of Appointments Hearings in the Northern Ireland Assembly
The Pharmaceutical Society of Northern Ireland supports the role of the Northern Ireland Assembly in scrutinising and monitoring the performance of the Northern Ireland Executive.
The Society notes the recent reforms in Westminster to allow Parliamentary Select Committees a greater role in scrutinising appointments[2] to key public sector organisations, including the conduct of non-binding appointment hearings after appointment but prior to commencement. A recent example is the House of Commons Health Committee’s hearing into the appointment of the chair of the Care Quality Commission[3].
The Society considers these reforms an important move towards greater transparency and accountability in the governance of public institutions and invites the Health and Social Care (Reform) Bill’s Scrutiny Committee to consider if the Committees of the Northern Ireland Assembly should be given a similar role in scrutinising the chief appointments to the Regional Health and Social Care Board, the Regional Agency for Public Health and Social Wellbeing and the Regional Support Services Organisation.
However, the Society recognises the process, or need for, appointments hearings may not need to be detailed in the Schedules of the Health and Social Care (Reform) Bill, and could instead be agreed informally with the Department.
[1] http://www.publications.parliament.uk/pa/ld200607/ldhansrd/text/71001w0005.htm#0709037000216
[2] http://www.cabinetoffice.gov.uk/newsroom/news_releases/2008/080602_appointments_process.aspx
[3] http://www.parliament.the-stationery-office.co.uk/pa/cm200708/cmselect/cmhealth/545/54502.htm
Royal College of Obstetricians
and Gynaecologists
Thank you for forwarding this Bill for comments which requires a formal response by 22nd August. The Northern Ireland Committee will not be meeting again until 1st September so on the plane home on Saturday I read the 57 pages of the new Bill and I have taken Chairman’s prerogative of replying personally.
This Bill is largely a legal document to change the framework of the way Healthcare is administered in Northern Ireland and I can see very little practical effect at the grass roots level. It is aimed at reducing the amount of bodies managing care in Northern Ireland and should bring the Province into line with the rest of the United Kingdom. This should only be an improvement on our current Four Health Board system and is hence welcomed.
I would not object to any of the proposed changes in the Bill but would point out that although patients and clients are mentioned frequently and seemed to be provided for very well there is no direct referral to Clinicians or Royal Colleges in an Advisory or Standard Setting capacity. This may be because the Bill is a high level and is merely setting out Governance and accountability arrangements at this level.
The Ulster Cancer Foundation
The Ulster Cancer Foundation submission to Northern Ireland Assembly Committee for Health, Social Services and Public Safety
The proposed reforms to the health and social care system have been much debated and consulted upon. The Health and Social Care (Reform) Bill was introduced on 23 June, had its Second Stage debate on 1 July and will progress through its Committee Stage when the Assembly returns from Recess in September.
The general principles of the Bill and the overall structure of the new system have been accepted. The Ulster Cancer Foundation believes that the focus during this stage must be on amendments to the Bill that will improve the transparency and accountability of the new system. The Ulster Cancer Foundation believes that the Northern Ireland Assembly Committee for Health, Social Services and Public Safety should have a strong oversight and consultation role in relation to the bodies being established under the legislation.
Clause 2 – Department’s General Duties
Clause 2 of the Bill deals with the general duties of the Department of Health, Social Services and Public Safety. Sub section (3) imposes specific tasks with regard to developing policies, determining priorities, allocating resources, set standards, preparing framework documents, securing the commissioning and development of programmes, etc.
The Ulster Cancer Foundation believes consideration should be given to whether it would be possible to insert an amendment to sub section (3) outlining a duty on the Department to proactively share the information it uses to carry out these functions with the Assembly Committee for Health, Social Services and Public Safety and other stakeholders.
Importantly, Clause 2 also imposes a duty on the Department to monitor and hold to account of the various Health and Social Care Boards, Agencies and Bodies. The Ulster Cancer Foundation believes that this monitoring information should be provided as a matter of course (rather than upon request) to the Committee and other stakeholders.
Clause 4 – Department’s Priorities and Objectives
Sub section (2)
The Bill leaves it to the discretion of the Department to decide on its priorities and objectives. The Ulster Cancer Foundation believes that the Committee should seek to amend this sub section to read:
“Before determining or revising any priorities or objectives under this section, the Department must consult with the Assembly Committee for Health, Social Services and Public Safety and a list of stakeholders drawn up in conjunction with the Committee.”
Sub section (3): The Ulster Cancer Foundation believes that the Committee should seek to amend this by adding:
“Where the Department acts without public consultation on the introduction of a new policy, due to the urgency of the matter, the Department should immediately inform and provide a detailed explanation of its actions to the Assembly Committee for Health, Social Services and Public Safety.”
Clause 5 – The Framework Document
The Framework Documents for each Health and Social Care body will be extremely important in defining the work of each body going forward. The Ulster Cancer Foundation believes it is, therefore, essential that the relatively weak consultation requirements in sub section (5) (b) are strengthened to read:
“(b) MUST consult with stakeholders drawn up in conjunction with the Assembly Committee for Health, Social Services and Public Safety.”
Clause 8 – Functions of the Regional Board
The work of the Regional Health and Social Care Board is critically important, particularly given its role as a collector and repository of information on the performance of the HSC Trusts. In order to maximise transparency and accountability, the Ulster Cancer Foundation believe an additional point should be added to sub section (2) that should read:
“(iv) for maximising transparency by making as much information as possible publicly available.”
Clause 9 – Local Commissioning Groups
Apparently, it is intended that the Local Commissioning Groups will be important decision makers within the new system. It is unclear, however, precisely how the balance of power between the various aspects of the new system inter-relate. The Foundation believes that the Committee should endeavour to ensure that the opportunities to input into the work of the LCG’s are maximised by amending sub section (4) (ii) to read:
“ - undertake such other consultation as the Department may direct in conjunction with the Assembly Committee for Health, Social Services and Public Safety
Or
- undertake such other consultation as the Committee may direct.”
Clause 13 – Functions of the Regional Agency for Public Health and Social Well-Being
The Ulster CancerFoundation believes that the Regional Agency for Public Health and Social Well-being (RAPHSW) will be an important source of information, which should be made available to the public. It is essential that it is an outward looking organisation that it is encouraged to share information with stakeholders through the Committee. Given this, the Ulster Cancer Foundation believes that sub section (6) should be amended by adding:
“(c) provide the Assembly’s Health Committee with such information, advice and assistance as they may reasonably require in connection with the exercise of their functions.”
19. Public involvement and consultation
The Foundation believes that it is important that information gathered by the Patient and Client Council is, whenever possible, made publicly available.
RNIB Northern Ireland
1. Introduction
1.1 RNIB is the major agency for people with sight loss in Northern Ireland, with direct and indirect services Province-wide and premises in Belfast, Derry/Londonderry, Omagh and Coleraine. We are in touch with the people we seek to serve in a number of ways, not least through our growing membership scheme and through the influence of our Committee and Assembly.
1.2 Our ambition is to make Northern Ireland the best place in the World for people with sight loss to grow up, be educated, live, work, socialise and grow old in. At the same time we seek to reduce avoidable sight loss through timely medical and social intervention.
1.3 We welcome this opportunity to engage with the Assembly Health Committee on the proposals to reform the structure of the health and social care system in Northern Ireland, as set out in the Health and Social Care Reform Bill.
1.4 We also look forward to the imminent launch of the All Party Group on Visual Impairment, which will provide an additional valuable forum in which to engage with MLAs on these and other key issues.
2. Policy Background
2.1 It is sterile to consider organisational structures unless we do so against a background of desired social outcomes. We were pleased to have an opportunity to present our Health and Social Care Manifesto to members of the Health Committee and to highlight our main concerns at the reception held at Stormont on 21st April. These priorities are summarised again below.
2.2 The elimination of avoidable sight loss is a key priority for us. We wish to see a speedy roll out of treatment for “wet” age related macular degeneration (AMD) for anyone with this condition, now that funding has been released by the Department of Health to rectify the cruelly restrictive policy which obtained until June of this year.
2.3 We have noted with deep concern the lack of targets in the Executive’s Programme for Government for reducing the incidence of common eye conditions such as wet AMD, glaucoma or diabetic retinopathy, or for the take-up of regular eye health checks. (See our responses to the draft Programme for Government and to the draft EQIA on the Programme for Government).
2.4 We believe that the public would be encouraged to look after their eyes if regular eye health checks were free of charge for everyone, as in Scotland. Evidence is now available which demonstrates the success of the Scottish Government’s policy in this area.
2.5 We are currently developing our Eye Care Liaison Service across the Province, based both in hospitals and via community optometrists, to bridge the gap between diagnosis and rehabilitation and to provide vital emotional support. This is being achieved entirely from charitable funds, a fundamentally unjust situation.
2.6 We are concerned at current inadequacies and inconsistencies in areas such as the assessment of need and the provision of equipment to assist people with sight loss in daily living, access to information and mobility. This was highlighted in our report “Ill Equipped - Are Blind and Partially Sighted People in Northern Ireland given the Tools for AN ACTIVE AND Fulfilling Life?”, published in may 2008.
2.7 In short, our concern is with the delivery of effective services which are equally available to all, which work towards the elimination of avoidable sight loss and at the same time promote the inclusion and empowerment of all those in Northern Ireland with any degree of sight loss. The UK Vision Strategy now provides a context in which to progress these aims.
3. Specific Comments on the Bill and Proposals for Change
Children’s Services
3.1 The Bill should be amended so that the respective duties of the Department of Health, the Regional Health and Social Services Board, and the Regional Agency for Public Health and Social Well Being each explicitly include an obligation to liaise with their counterparts in the education sector.
3.2 The Bill as currently drafted completely overlooks the need to deliver joined-up services to children. One specific example is the need to ensure that children with sight loss not only benefit from a fully inclusive classroom experience but also receive mobility and daily living skills and emotional support for themselves and their families. Some may need educational provision while undergoing medical treatment. Thus health, social care and education services must be co-ordinated at every level.
User Involvement
3.3 It is essential that the bodies delivering our health and social care services benefit from the involvement of users and their representative organisations. Yet the Bill is very unclear on this. Clauses 19 and 20 set out duties to consult, but these seem a strange mixture of general public consultation and adequate consultation with individual users and carers on their specific care needs. The two issues need to be legislated for distinctly.
3.4 As regards the membership of the Patient and Client Council, we note that Schedule 4 allows for regulations to be made at a later stage stipulating the range and sorts of people to be appointed. We believe that the Bill should be more explicit and specify that membership should include people with direct experience of disability. If this were done, then other sectors would probably have to be specified as well, such as people on low income or people in rural areas, but this would not be detrimental.
3.5 The Board and agency, too, need to be informed by guaranteed input from those with direct experience of disability. At the moment, the Bill contains no stipulations about who the Minister should appoint or what expertise should be co-opted.
Responsibility for Eliminating Avoidable Sight Loss
3.6 It is unclear from the Bill where responsibility will lie for promoting and facilitating regular eye health checks amongst the general population. Regular checks can detect many common eye conditions before the sufferer is aware of them and in time to arrest their development. Thus regular checks save sight and save the money that might otherwise have to be spent later on treatment and on rehabilitation.
3.7 Increased take-up should be a core objective of Government policy, with annual targets. It requires increased public understanding and the elimination of financial disincentives.
3.8 Encouraging regular take-up would seem to fall within the remit of the Agency, while procuring eye health checks from optometrists , and reducing or removing charges, would seem to fall with the Board. The same is no doubt true in other areas of health promotion. The duties of the bodies need to reflect a responsibility on the part of the Board to facilitate the public health goals determined by the Agency.
Tackling Health Inequality.
3.9 Reducing health inequality appears in the Bill as a duty of the Department and of the Regional Agency for Public Health and social Well Being, but is not mentioned as a duty of the Regional Health and Social Care Board. This could usefully be rectified.
The Role of the Voluntary Sector
3.10 The voluntary sector has a vital role to play in voicing the needs of patients and clients, but also as a pool of expert knowledge. In addition, voluntary agencies are often well qualified to bid for contracts to deliver services. It is in everyone’s interests to keep these two roles distinct.
3.11 It is uncertain from the current proposals whether voluntary sector bodies would contract with the Trusts or with the new Regional Health and Social Care Board. Contracting with the Board would ensure more consistent services across Northern Ireland.
3.12 Unfortunately, voluntary agencies far too often find themselves having to plug gaps left by the statutory sector. It may not be unreasonable for charitable funds to be used to pioneer new ways of working, but once need and value has been established the statutory sector should assume responsibility. Furthermore, contracts awarded to the voluntary sector should be on a full cost recovery basis.
3.13 Since we also see the voluntary sector having a role to play in influencing the policies and priorities of the Board and the other new bodies, it is also important to have in place procedures which ensure openness and transparency in the awarding of contracts.
Optometrists
3.14 Optometry is an increasingly important profession in the fight against avoidable sight loss. The profession merits a guaranteed place at the very least on local commissioning groups.
4. Further Information
4.1 We would be delighted to talk to members of the Health Committee further on these issues. In the first instance, please contact David Mann, Campaigns Manager, RNIB Northern Ireland, 40 Linenhall Street, Belfast BT2 8BA, tel. 028 9032 9373, David.Mann@rnib.org.uk. or Charlie Mack, Senior Manager, Regional Services, at the same address and telephone number, Charlie.mack@rnib.org.uk.
The British Red Cross
The British Red Cross was pleased to respond to the consultation document regarding the proposed Health and Social Care (Reform) Bill 2008 earlier this year and welcomes the proposals in the second reading of the Bill to have voluntary sector representation on Local Commissioning Groups.
While we note that Section 13(3)(b) of the Bill refers to emergencies, we are still unclear from reading the consultation document section how the new and existing bodies will work together in both emergency response and risk reduction. Given the recent flooding in Northern Ireland, this has become all the more pertinent.
Future clarification of roles notwithstanding, the Red Cross further notes that Section 13(2)(b) could be strengthened by adding the words “and risk reduction” after “health promotion”. This would enhance the Bill in terms of the health improvement functions of RAPHSW by giving specific reference to human risk reduction and resilience, the result of which would be a community less vulnerable to individual and/or communal crises.
The Red Cross is very keen to be part of subsequent discussions on how the new and existing bodies will work together in emergency planning and response and would welcome the opportunity to address the Committee in its hearings during the commencement stage of the Bill in September.
To help emergency services in Northern Ireland better understand our local and national capabilities, we have recently developed a resource pack entitled Here to help you respond. The pack contains a range of information highlighting how the Red Cross is ideally placed to assist the emergency services in responding to local emergencies across the UK. I enclose a copy of our local brochure for the Committee.
I would be most pleased if you could contact our Public Affairs Officer, Alison Bunting, whose details appear below about the possibilities of engaging with the Committee on the issues raised in relation to the Bill and a more general discussion on our engagement with the emergency responders.
The Community Development
and Health Network
Introduction
CDHN’s mission is to end health inequalities using a community development approach. By this we mean campaigning, influencing policy and developing best practice work which shows that communities, both geographical and of interest & identity, can define their own health needs and design and implement preventative and radical solutions.
This submission contains CDHN’s analysis of the NIA Bill 21/07 Health and Social Care (Reform) Bill. The analysis is built upon CDHN’s response to the consultation on the Ministerial Reforms that took place between March and May 2008.
In its response to the spring 2008 consultation process, CDHN analysed the proposals by asking whether or not users, carers and communities would be equal partners in health and social care decision-making, i.e. the degree to which mainstreaming community development approaches were supported by the proposed reforms.
CDHN continues to use this yardstick to measure the potential success of the Reform Bill in terms of mainstreaming community development approaches. In addition, we also comment on whether or not CDHN’s response (and members’ responses) to the consultation have been taken up, or not, in the Reform Bill.
Executive summary of CDHN submission to consultation on proposed Ministerial Reforms of Health and Social Care, May 2008
The following is an executive summary of CDHN’s response to the spring 2008 consultation on the DHSSPS Proposals for health and social care reform. We are including it here to act as an aide mémoire against which the reader can refer as they go through the CDHN Submission to the NI Assembly Health, Social Services and Public Safety Committee on the NIA Bill 21/07 Health and Social Care (Reform) Bill, August 2008.
Executive Summary
- Responsibility for and direction of community development approaches should be mainstreamed throughout the health and social care system and not placed solely within the new Regional Public Health Agency. Community development approaches, where users, carers and communities are equal partners in health and social care decision-making are necessary in all programs of care, not only in public health. Policy development of community development approaches should be maintained within the Department and should be included in new performance management systems anchored in the new RHSCB. Implementation would then happen via LCGs, Trusts, primary care contractors, community and voluntary sectors and the RPHA.
- ‘Communities’ should be included along with the language on patients, clients and carers. This ensures a commitment to work beyond simple complaint models of user involvement and instead reflects a commitment to work with wider communities as co-designers, co-planners and co-providers of health and social care. In addition, it would also reflect the Minister’s commitment to tackling the unequal distribution of the wider determinants of health (social model) and to tackling health inequalities which are experienced by whole communities. It would also reflect the Minister’s commitment to the ‘fully engaged’ scenario.
- The Statutory Duty of Engagement described in the first round of RPA HSC changes should be reinstated.
- The number of lay representatives on LCGs should be maintained at 2 – reducing the lay representatives from 2 to 1 on each LCG means a reduction from 14 to 5 lay representatives in the commissioning system.
- There should be stronger emphasis on the crucial role of the community and voluntary sectors, especially when it comes to local planning, delivery and engagement.
- CDHN welcomes the strong Ministerial commitment that ‘Improved health and well-being and reduced health inequalities are the yardsticks by which the success of that system will be measured’. CDHN is concerned that the new RPHA might result in a situation where commitment to community development approaches and to tackling health inequalities might become disconnected from other parts of the system. CDHN believes that health improvement, community development and health inequalities functions of Trusts and commissioners should remain inside the relevant bodies and not be transferred to the RPHA.
- Tackling health inequalities must be a function of the RPHA.
- CDHN welcomes the involvement of local government in health and social care, particularly because it enhances our ability to tackle the underlying causes of poor health. However, CDHN believes that this should not be a replacement for either the maintenance of lay representatives in commissioning or working in equal partnership with users, carers and communities.
- The reforms should place stronger emphasis on social care.
Executive summary of CDHN Submission to the NI Assembly Health, Social Services and Public Safety Committee on the NIA Bill 21/07 Health and Social Care (Reform) Bill, August 2008
CDHN has suggested the following amendments:
Section 8, (3)
(3) The Regional Board must in respect of each financial year prepare and publish a document (“the commissioning plan”) setting out such details as the Department may direct concerning —
(a) the health and social care which the Board is to commission in that year; and
(b) the costs to be incurred in that regard;
and in drawing up the commissioning plan the Board must show that RAPHSW was fully involved in and had an impact on the commissioning decisions taken therein;;
and in drawing up the commissioning plan show that users, carers and communities were fully involved in and had an impact on the commissioning decisions taken therein.
Section 9, (4), (i) & (ii)
(4) Each Local Commissioning Group must —
(b) in connection with the exercise of its functions —
(i) work jointly with RAPHSW and have ensure that its advice has an impact on the commissioning decisions the LCG makes; and
(ii) work jointly with users, carers and communities and have ensure that its advice has an impact on the commissioning decisions the LCG makes; and
(iii) undertake such other engagement as the Department may direct.
Section 9, (5), (a)
5) Each Local Commissioning Group must exercise its functions with the aim of —
(a) improving the health and social well-being of and reducing health inequalities for people in the area as regards which the Local Commissioning Group exercises its functions;
Section 19 (1) (a)
19.— (1) Each body to which this section applies must take such steps as it considers appropriate —
(a) to promulgate information about the health and social care and upstream health inequalities work for which it is responsible;
Section 20 (1) (d)
20.— (1) A consultation scheme must make it clear how the body to which the scheme is to apply will make arrangements with a view to securing, as respects health and social care for which it is responsible, that the following are (directly or through representatives) involved in and consulted on the matters mentioned in subsection (2), namely —
(a) the Patient and Client Council;
(b) persons to whom that care is being or may be provided;
(c) the carers of such persons (that is to say the individuals who provide a substantial amount of care on a regular basis for such persons but who are not employed to do so by a health and social care body); and
(d) wider communities.
Section 21
21. It is the duty of an HSC trust to exercise its functions with the aim of improving the health and social well-being of and reducing health inequalities between those for whom it provides, or may provide, health and social care.
CDHN Submission to the NI Assembly Health, Social Services and Public Safety Committee on the NIA Bill 21/07 Health and Social Care (Reform) Bill, August 2008
1 The Framework document (Section 5)
CDHN notes that the legislation instructs the Department to prepare a framework document for each new body created under the legislation. We note that these frameworks documents are currently being prepared. We presume that the detail contained in the framework documents will constitute any later regulations which will form the underpinning detail to the more ‘high-level’ legislative requirements in this Reform Bill. It is difficult therefore to respond in great detail to the Reform Bill itself as many of the detailed concerns which we outlined in our response to the consultation paper relate to, for example the number of Local Commissioning Groups and how many lay representatives will be on each LCG.
CDHN comments on the ‘consultation duty’ below, but does not believe that it offers a strong enough mechanism to mainstream the full and equal involvement of users, carers and communities into health and social care decision-making.
CDHN notes, in addition, that the Department is developing the framework documents even though the Reform Bill has not yet been passed. This appears to assume that the reform timetable will be met and that the new HSC bodies will need a detailed framework to proceed from the 1st April 2009.
CDHN is concerned with ensuring that users, carers and communities are co-designers, co-planners and co-providers of services and are therefore, integral to decision-making at every level (and not only via a single organisation like the Patient Client Council) and it is not possible to tell from the Reform Bill whether or not these framework documents will support this integration.
2 The Regional Health and Social Care Board (Section 7 & 8)
CDHN believes that the RHSCB should be obliged to work with users, carers and communities as equal partners in the commissioning decision-making process. The RHSCB should work with users, carers and communities by asking them to report on whether or not in their opinion service and health inequalities targets are being met. The RHSCB should also work with users, carers and communities in developing a community development performance management framework which would apply to all health and social care bodies.
Again, though this issue may be dealt with under the framework document for the RHSCB in the manner outlined below, CDHN has no way of knowing whether or not this will be the case. Should it not, CDHN would advise that Section 8, (3), be amended to the following statement:
Section 8, (3)
(3) The Regional Board must in respect of each financial year prepare and publish a document (“the commissioning plan”) setting out such details as the Department may direct concerning —
(a) the health and social care which the Board is to commission in that year; and
(b) the costs to be incurred in that regard;
and in drawing up the commissioning plan the Board must consult RAPHSW and have due regard to any advice or information provided by it;
and in drawing up the commissioning plan show that users, carers and communities were fully involved in and had an impact on the commissioning decisions taken therein.
CDHN notes that Section 8, (3) includes an obligation to consult RAPHSW and have ‘due regard’ to any advice or information provided by it’. This is the same language as used in the current equality duty, in Section 75 of the Northern Ireland Act 1998, where public authorities must
- Between persons of different religious belief, political opinion, racial group, age, marital status or sexual orientation;
- Between men and women generally;
- Between persons with a disability and persons without; and
- Between persons with dependants and persons without.’
Public authorities are also required to have regard to the desirability of promoting good relations between persons of different religious belief, political opinion or racial group[1]. The ECNI notes ‘Consultation with those affected by public policy decisions is central to the effectiveness of the duties. Equality schemes spell out an authority’s arrangements for consultation on the duties and on the likely impact of policies.’
CDHN notes that procedurally focused consultations have become the main way in which equality is served inside health and social care bodies. Often, this equality consultation process is process-led i.e. the how we do it is more important than the outcomes generated, i.e. that people do actually end up having their views counted in decision-making.
CDHN notes that a duty to consult RAPHSW and to have due regard to its advice is unlikely to avoid the trap of becoming a procedural technicality. As a result, CDHN has phrased its proposed amendment on working with users, carers and communities in quite different language, requiring instead that the finished commissioning plan must show the outcomes of working with users, carers and communities – to show the impact of their contribution, rather than showing only that they were present.
CDHN would suggest that similar language be used with regard to the relationship between the RHSCB and the RAPHSW:
Section 8, (3)
(3) The Regional Board must in respect of each financial year prepare and publish a document (“the commissioning plan”) setting out such details as the Department may direct concerning —
(a) the health and social care which the Board is to commission in that year; and
(b) the costs to be incurred in that regard;
and in drawing up the commissioning plan the Board must consult RAPHSW was fully involved in and had an impact on the commissioning decisions taken therein;
and in drawing up the commissioning plan show that users, carers and communities were fully involved in and had an impact on the commissioning decisions taken therein.
3 Local Commissioning Groups (Section 9)
9.— (1) The Regional Board shall in accordance with paragraph 7 of Schedule 1 appoint a prescribed number of committees to be called “Local Commissioning Groups”.
CDHN made a series of comments on the number of Local Commissioning Groups to be established, the proposal to reduce these from 7 to 5. CDHN noted the benefits of co-terminosity with Trusts and local government boundaries but pointed out that it was unlikely they would have the same local reach and effect as if there were 7 LCGs or indeed, the originally conceived Community Commissioning Associations. In addition, CDHN noted how a reduction of lay representatives on the LCG from 2 to 1 would also mean that overall, lay representatives would be reduced from 14 to 5, a substantial decrease.
Again the legislation seems to be leaving this to be resolved by the regulations and/or framework document, but these are central points and CDHN is disappointed not to see this in the primary legislation.
With regard to Section 9, (4), (i) & (ii)
(4) Each Local Commissioning Group must —
(b) in connection with the exercise of its functions —
(i) consult RAPHSW and have due regard to any advice or information provided by it; and
(ii) undertake such other consultation as the Department may direct.
CDHN would reiterate the above comments on the weaknesses of a consultation duty, as opposed to focusing on the outcomes of that joint working and would suggest the following amendments:
Section 9, (4), (i) & (ii)
(4) Each Local Commissioning Group must —
(b) in connection with the exercise of its functions —
(i) work jointly with RAPHSW and have ensure that its advice has an impact on the commissioning decisions the LCG makes; and
(ii) work jointly with users, carers and communities and have ensure that its advice has an impact on the commissioning decisions the LCG makes; and
(iii) undertake such other engagement as the Department may direct.
The amendment to Section 9, 4 (b) (i) reflects the need to focus on the outcomes of joint working on commissioning; the amendment to Section 9, 4 (b) (ii) reflects the need to ensure that LCGs specifically work with users, carers and communities, i.e. the people to use services, are affected by service experience and who live in communities and the need to ensure that their views have an impact on commissioning and the addition in the third amendment, Section 9, 4 (b) (iii), is to change the word consultation and replace it with engagement on the basis that engagement is a reciprocal work that reflects full joint-working rather than consultation, with often sees users, carers and communities offered a pre-set list of options rather than treated as full partners.
Finally, with regard to Section 9 on Local Commissioning Groups, CDHN would note that tackling health inequalities is not included as an aim of the LCG:
(5) Each Local Commissioning Group must exercise its functions with the aim of —
(a) improving the health and social well-being of people in the area as regards which the Local Commissioning Group exercises its functions;
(b) planning and commissioning health and social care to meet the needs of people in that area;
(c) securing the delivery to people in that area of health and social care that is efficient, co-ordinated and cost-effective;
(d) improving the availability and quality of health and social care in that area.
CDHN noted in its response to the consultation proposal that tackling health inequalities should be the responsibility of the whole system, rather than only the RAPHSW and as such suggest the following amendment:
Section 9, (5), (a)
5) Each Local Commissioning Group must exercise its functions with the aim of —
(a) improving the health and social well-being of and reducing health inequalities for people in the area as regards which the Local Commissioning Group exercises its functions;
4 The Regional Agency for Public Health and Social Well-being (Sections 12 & 13)
CDHN’s is happy to see that the Agency will have a clear focus on reducing health inequalities, a function which had been absent from the original proposals.
Functions of RAPHSW
13.— (1) RAPHSW shall exercise on behalf of the Department —
(a) the health improvement functions mentioned in subsection (2); and
(b) the health protection functions mentioned in subsection (3).
(2) The health improvement functions are —
(a) developing and providing, or securing the provision of, programmes and initiatives designed to secure the improvement of the health and social well-being of, and reduce health inequalities between, people in Northern Ireland; and
Our concerns were that the Agency would see the separation of firstly health inequalities work away from all other health and social care bodies, rather than the mainstreaming that CDHN believes needs to occur in order to effective reduce health inequalities and secondly, that if the Agency were given primary responsibility for reducing health inequalities and not given the necessary powers to compel other HSC bodies to action, then the system’s capacity to reduce health inequalities would be severely weakened.
Other health and social care bodies must have ‘regard’ to the advice of the Agency, but the ‘have regard’ is a relatively weak legal duty, with no obligation to ensure that the agency’s advice actually changes what the body plans to do. In addition, it does not appear that the Trusts are bound to ‘have regard’ to the advice of the Agency and yet there is a specific mention of their role in improving health and well-being.
5 The Patient Client Council (Sections 16, 17, 18, 19, & 20)
CDHN’s concerns about the implied expanded role of the Patient Client Council reflect our commitment to ensuring that every health and social care body is obliged to mainstream the full and equal involvement of users, carers and communities into their decision-making processes.
CDHN objects to a system with only one channel (the PCC) for views from users, carers and communities to be fed into health and social care decision-making.
CDHN also objects to using consultation processes only rather than mainstreaming the full and equal involvement of users, carers and communities. This is because consultation often only means that users, carers and communities respond to a pre-set menu of options rather than being involved from the beginning where they can shape the possible options.
The Reform Bill states:
Functions of the Patient and Client Council
17.— (1) The Patient and Client Council has the following functions as respects the provision of health and social care in Northern Ireland —
(a) representing the interests of the public;
(b) promoting involvement of the public;
If this means that the PCC becomes the sole way in which the interest of the public would be represented and their involvement organised then CDHN cannot support it. If this would not replace, but rather augment mainstreaming the full and equal involvement of users, carers and communities into health and social care decision-making processes then CDHN would support it.
The Reform Bill states:
Functions of the Patient and Client Council
17. — (1) The Patient and Client Council has the following functions as respects the provision of health and social care in Northern Ireland —
(d) promoting the provision by bodies to which this section applies of advice and information to the public about the design, commissioning and delivery of health and social care;
We welcome this if it means that health and social care bodies are going to provide more information and advice to the users, carers and communities about the design, commissioning and delivery of health and social care. However, we would note that our aim is to see users, carers and communities as equal partners and co-designers, co-commissioners and co-deliverers of health and social care rather than only receiving advice and information.
With regard to this last point, the Reform Bill goes on to state:
17 (3) In exercising its functions under subsection (1)(b), the Patient and Client Council shall promote the involvement of the public in consultations or processes leading (or potentially leading) to decisions by a body to which this section applies which would or might affect (whether directly or not) the health and social well-being of the public.
CDHN welcomes the recognition in this clause that the involvement of the public might be through consultation or other processes, which hopefully would be more meaningful than consultations. CDHN welcomes the promotion of these processes by the Council.
Later the Reform Bill states:
17 (5) The Patient and Client Council shall —
(a) undertake research and conduct investigations into the best methods and practices for consulting the public about, and involving them in, matters relating to health and social care; and
(b) provide advice regarding those methods and practices to bodies to which this section applies.
CDHN welcomes the serious commitment to consultation and involvement best practice, as seen here. CDHN hopes that the Patient Client Council will work closely with the community and voluntary sectors and users, carers and communities in terms of the research and investigations and also in formulating advice for health and social care bodies.
The Reform Bill states:
17 (7) In this section “the public” includes individuals, a group or community of people and a section of the public, however selected.
CDHN strongly welcomes this recognition that when it comes to working with the public, we do not only mean individuals who experience services, but rather also a group or community of people and a section of the public, however they choose to define themselves.
6 Public Involvement and Consultation (Section 19 & 20)
CDHN very much welcomes the aim of these sections to ensure that health and social care bodies that users and carers are widely involved in decision-making with regard to services and changes to services.
The following comments suggest possible additions to the clauses to ensure that this aim is fully realised.
CDHN notes that not only is information about care and services needed but also information and transparency about work that aims to reduce health inequalities, the preventative, upstream work that health and social care bodies take on. Users, carers and communities need information on this work in the same way as they do about services and care.
The Reform Bill states:
19.— (1) Each body to which this section applies must take such steps as it considers appropriate—
(a) to promulgate information about the health and social care for which it is responsible;
(b) to obtain information about—
(i) the needs of persons to whom that care is being or may be provided; and
(ii) the efficacy of that care;
(c) to encourage and assist persons to whom that care is being or may be provided—
(i) to avail of that care in an appropriate manner, having regard to the need to use resources in the most economic, efficient and effective way; and
(ii) to maintain and improve their own health and social well-being.
The Bill here mentions care and individuals maintaining and improving their own health and social well-being. There is a third category of health inequalities work that tackles the unequal distribution of the wider determinants of health, education, relative income, the environment etc.
CDHN suggests the following amendment:
Section 19 (1) (a)
19.— (1) Each body to which this section applies must take such steps as it considers appropriate—
(a) to promulgate information about the health and social care and upstream health inequalities work for which it is responsible;
CDHN notes that the Minister has chosen, in the Reform Bill, to use consultation schemes as a way to oblige health and social care bodies to involve and consult with users, carers and wider communities.
20.— (1) A consultation scheme must make it clear how the body to which the scheme is to apply will make arrangements with a view to securing, as respects health and social care for which it is responsible, that the following are (directly or through representatives) involved in and consulted on the matters mentioned in subsection (2), namely—
(a) the Patient and Client Council;
(b) persons to whom that care is being or may be provided;
(c) the carers of such persons (that is to say the individuals who provide a substantial amount of care on a regular basis for such persons but who are not employed to do so by a health and social care body); and
In its submission to the consultation in the spring, CDHN supported the re-inclusion of the Statutory Duty of Engagement, which had been present in the original RPA proposals. CDHN notes that this Reform Bill has reinstated the duty in the form of these consultation schemes. However, CDHN also notes that the learning from the Section 75 equality duty suggests that though equality schemes have led to substantial cultural change around equality within organisations – their original aim – they have also created a bureaucratic burden which has occasionally allowed the body to avoid mainstreaming equality issues, as the focus becomes one of process rather than outcome.
CDHN notes that many health and social care bodies have already or are in the process of developing community development strategies which enact the recommendations in the Community Development Performance Management Framework (see enclosed) and the CDHN Engagement Toolkit for Commissioners (see enclosed). In doing so, they can fulfill the highest standards of consultation, principles of public and patient involvement, stakeholder engagement and equal partnership between health and social care bodies and users, carers and communities.
CDHN also notes that there is also an extensive consultation duty under Section 75. In most health and social care organisations, the equality scheme reflects the groups listed under the duty (persons of different religious belief, political opinion, racial group, age, marital status or sexual orientation, men and women, persons with a disability and persons without; and persons with dependants and persons without) and so lies horizontally across an organisation rather then reflecting the vertical health and social care programmes of care. We presume that the intention behind the consultation schemes in the Reform Bill is to ensure that progammes of care consult widely with users, carers and communities, but surely it would be more sensible to blend the identity approach of Section 75 with the populations as defined by programs of care rather than burdening the system with an additional reporting mechanism.
CDHN would prefer the health and social care bodies were obliged, under a Statutory Duty of Engagement, to performance manage effective involvement of and consultation with users, carers and communities as a way to guarantee this, rather than using the more bureaucratic mechanism of a consultation scheme. CDHN would therefore recommend taking the consultation scheme obligation out of the Reform Bill and instead, keeping at Statutory Duty of Engagement which would manifest in the performance management of community development approaches. This could be designed within the Framework document.
Delete Section 20 (1) (d)
If, however, the consultation schemes remain in the Reform Bill, CDHN welcomes Section 20 (1) that people should be both ‘involved in and consulted on’.
However, CDHN notes that Section 20 (1) (a) (b) & (c) list those to be involved and consulted as the Patient Client Council, persons receiving care and carers, but not wider communities.
CDHN suggests that this be amended to include involving and consulting wider communities:
Section 20 (1) (d)
20.— (1) A consultation scheme must make it clear how the body to which the scheme is to apply will make arrangements with a view to securing, as respects health and social care for which it is responsible, that the following are (directly or through representatives) involved in and consulted on the matters mentioned in subsection (2), namely—
(a) the Patient and Client Council;
(b) persons to whom that care is being or may be provided;
(c) the carers of such persons (that is to say the individuals who provide a substantial amount of care on a regular basis for such persons but who are not employed to do so by a health and social care body); and
(d) wider communities.
Again, if the consultation schemes remain in the Reform Bill, CDHN notes that at Section 20 (3) (a) the language ‘have regard to’:
(3) The consultation scheme must provide for the body to which it is to apply—
(a) to have regard to any comments submitted to it in response to the consultation; and
(b) to prepare a written statement which—
(i) summarises the comments received; and
(ii) sets out the body’s response to those comments.
(4) The consultation scheme must provide that the body to which it is to apply shall take such steps as in its opinion will give adequate publicity to the statement.
is weaker than the Section 75 duty to ‘have due regard to’. In addition, the Section 75 duty is built around avoiding or mitigating the negative impact of policies on equality. However, no avoidance or mitigations actions are requested here. So for example, should a user group note that a proposed change to a service will have X negative effect, though there is an obligation to regard (listen to?) this comment, there is no attendant obligation to stop the change happening or to mitigate the impact of its negative consequences.
As noted before, CDHN suggests that the obligation to on consultation scheme be removed, but should it remain an emasculated bureaucratic obligation seems even more redundant than a potent obligation scheme.
7 Duty on HSC trusts in relation to improvement of health and social well-being (Section 21)
CDHN welcomes the duty at Section 21:
21. It is the duty of an HSC trust to exercise its functions with the aim of improving the health and social well-being of those for whom it provides, or may provide, health and social care.
on the understanding that it confirms the role of health improvement and community development with health and social care Trusts.
CDHN would add that Trusts should have a duty to exercise its functions with the aim of reducing health inequalities between those for whom it provides, or may provide, health and social care and would therefore suggest the following amendment:
Section 21
21. It is the duty of an HSC trust to exercise its functions with the aim of improving the health and social well-being of and reducing health inequalities between those for whom it provides, or may provide, health and social care.
Involvement of local government
CDHN notes that the Reform Bill does not refer to how local government representatives will be involved formally in commissioning and in public health, yet these are crucial issues which will affect the roll out of important health and social care work, and have a substantial impact on how users, carers and communities are included as equal partners in health and social care decision-making. In absence of specific clauses, and on the understanding that these issues may be dealt with within the Framework document CDHN can only reiterate its earlier statement on this:
- CDHN welcomes the involvement of local government in health and social care, particularly because it enhances our ability to tackle the underlying causes of poor health. However, CDHN believes that this should not be a replacement for either the maintenance of lay representatives in commissioning or working in equal partnership with users, carers and communities.
[1] Equality Commission Northern Ireland website, http://www.equalityni.org/sections/default.asp?cms=Policy_Section%2075%20-%20the%20statutory%20duty&cmsid=89_98&id=98&secid=6
Lisburn City Council
10 September 2008
I refer to your letter dated the 4th July, 2008 on the above subject and to your agreement facilitate the submission of the Council’s comments by extending the closing date until today.
I can advise you that, at its Meeting held on the 9th September, 2008 the Council’s Corporate Services Committee agreed that the provisions of the Bill should be such so as to ensure that local authorities achieved optimum representation on those bodies to be established.
This response is subject to ratification by the Council at its Meeting to be held on the 23rd September, 2008. I shall correspond with you after that date to advise you as to whether or not the response was accepted by the Council.
24 September 2008
I refer to my letter dated the 10th September, 2008 on the above subject and hereby confirm that, at its meeting held on 23rd September, 2008 the Council accepted the recommendation of its Corporate Services Committee that the Bill should be such so as to ensure that local authorities achieved optimum representation on those bodies to be established.
Appendix 4
Written Evidence and
Other Correspondence Considered by the Committee
Research and Library Services

5th of September 2008
Health and Social Care (Reform) Bill
Neil Foster
The Health and Social Care (Reform) Bill was introduced to the Northern Ireland Assembly on 23 June 2008. The main purpose of the Bill will be to provide the legislative framework within which the proposed new health and social care structures can operate.
To facilitate Members’ consideration of the Bill this paper seeks to identify any potential gaps in the legislative provision specifically in relation to the functions and responsibilities of the key health and social care organisations proposed within the Bill.
Library Research Papers are compiled for the benefit of Members of The Assembly and their personal staff. Authors are available to discuss the contents of these papers with Members and their staff but cannot advise members of the general public.
Executive Summary
The Health and Social Care (Reform) Bill represents one the most significant pieces of legislation affecting the Northern Ireland health service in recent decades. The current provision of health and social care in Northern Ireland is provided by the Health and Personal Social Services (Northern Ireland) Order 1972. This piece of legislation has been significantly amended over the years. The Health and Social Care (Reform) Bill will deliver a major overhaul of the existing structures underpinning the health and social care system. The Bill contains legislative provision for the reconfiguration of a number of key organisations including the creation of a smaller Department, an amalgamation of the four existing Health and Social Services Boards into one Regional Board accompanied by 5 Local Commissioning Groups, the creation of a new Regional Agency for Public Health and Social Well-Being and the amalgamation of four existing Health and Social Services Councils into one body – the Patient and Client Council.
This paper provides an overview of the legislative provisions in the Bill, focusing on the functions and responsibilities of the key health and social care organisations. The paper also seeks to identify potential changes to the legislation and has considered the multitude of views expressed within the considerable number of responses to the consultation exercises conducted by the DHSSPS on their HSC reform proposals and the HSSPS Committee on the Health and Social Care (Reform) Bill itself. In examining the proposed legislative framework within the Bill, a key observation is that the DHSSPS has chosen to advocate the retention of a highly centralised approach to health and social care delivery in which power cascades down from the Department and the Regional Board. Despite the contention of the Department to ‘support democratisation within the system’, there is evidence that in the configuration of powers of the Local Commissioning Groups there is insufficient levels of autonomous decision-making and budgetary control.
Contents
1. Background to the Health and Social Care (Reform) Bill
1.1 Rationale for the Bill
1.2 Consultation Process
1.3 Overview of the Bill
2. Functions of key Health and Social Care Organisations
3. Other relevant clauses and issues
Annex
1. Background to the Health and Social Care (Reform) Bill
Shortly following appointment as Minister for Health, Social Services and Public Safety in May 2007, Michael McGimpsey ordered a review of the raft of proposals for reform of the Health and Social Care in Northern Ireland put forward as part of the Review of Public Administration (RPA). Indeed, the decision to reconsider all the plans devised during suspension is one that the Minister has supported since coming into office. In a speech to the Assembly on 4th February 2008, the Minster stated that:
…the return of devolution, with a local Minister and a local Assembly scrutinising their work presents a real opportunity to deliver a local solution that meets our local needs. I have said it before, and I shall say it again: I make no apology for having taken the time to consider the organisational changes that are required to put in place arrangements that are fit for purpose, both now and in the future and that will deliver the best possible outcome for patients and clients. To do otherwise would be to fail the people of Northern Ireland.[1]
1.1 Rationale for the Bill
The purpose of the Bill will be to provide the legislative framework within which the proposed new health and social care structures can operate. The Bill seeks, either within the body of the Bill or by securing sufficient power to make subordinate legislation, to establish the parameters within which each health and social care body will be permitted to operate and to establish the necessary governance and accountability arrangements, which will support the effective delivery of health and social care in Northern Ireland.[2]
1.2 Consultation exercises
A formal consultation exercise on the DHSSPS’s policy proposals to inform the draft Health and Social Care (Reform) Bill was undertaken during the period from the 18th February 2008 until the 12th May 2008. By the end of the consultation process the DHSSPS received over two hundred responses from various stakeholders including other Health and Social Care (HSC) organisations, the medical profession, the voluntary and community sector, academia and the trades unions.
Meanwhile, at their meeting on the 3rd July 2008, the Committee for Health, Social Services and Public Safety authorised the commencement of a consultation exercise on the Health and Social Care (Reform) Bill. The consultation exercise ended on the 22nd August 2008. Throughout this paper, clear indication will be made between those responses received throughout the Department’s consultation exercise on their HSC reform proposals and the HSSPS Committee’s consultation exercise on the HSC (Reform) Bill.
A concern expressed by the organisation Children in Northern Ireland (CiNI) relates to how the responses received during the DHSSP’s consultation process are used by them to inform the draft legislation. According to CiNI, their concerns have ‘been considerably heightened by confirmation that it is not the Department’s intention to consult on the draft reform legislation which will be laid before the Assembly.’[3] The response raises an important issue regarding the timing of the DHSPSS’s consultation process and the publication of the Health and Social Care (Reform) Bill. With the consultation exercise ending in mid May 2008 and the Bill published several weeks later in mid Jun 2008 it supports the concern expressed by CiNI regarding the extent to which the DHSSPS took cognisance of the responses in the drafting of the HSC (Reform) Bill. It is also worth noting that the DHSSPS’s response to the submissions received during the consultation exercise is due to be published in early to mid September 2008. In this regard, the timetabling of the different stages between the ending of the consultation exercise and publication of the Bill seems incongruous with the Minister’s initial commitment to ‘go back to first principles’ and allow adequate time for serious consideration of the structural reform proposals and drafting of the legislation.
1.3 Overview of the Bill
The Bill comprises 35[4] clauses and 7 Schedules and is divided into 10 broad headings:
- Restructuring of administration of health and social care – covers the restructuring of health and social care bodies;
- Department’s role in promoting and providing health and social care – consists of 5 clauses and outlines the general duties, powers and priorities of the Department of Health, Social Services and Public Safety (DHSSPS)
- The Regional Board – consists of 5 clauses and provides for the establishment of the Regional Health and Social Care Board. It also covers the functions of the Regional Board and outlines its objectives;
- RAPHSW – consists of 2 clauses and provides for the establishment of the Regional Agency for Public Health and Social Well-being;
- RSSO – consists of 2 clauses and provides for the establishment of the Regional Support Services Organisation;
- Patient representation and public involvement – establishes the Patient and Client Council, covers the functions of the Patient and Client Council (PCC) and deals with the need for health and social care bodies to consult with service users and produce consultation schemes;
- HSC trusts – places a duty on HSC trusts in relation to the improvement of health and social well-being;
- Public-private partnerships – provides for the Department of Health, Social Services and Public Safety, the Regional Health and Social Care Board, the Health and Social Care trusts, the RSSO, special agencies and the RAPHSW to form, or participate in forming, public-private partnerships;
- Transfer of assets, liabilities and functions – deals with the dissolution of various health and social care bodies and the transfer of assets, liabilities and functions;
- Supplementary – provides for the Department to make supplementary provisions as it thinks necessary and makes general provisions in respect of subordinate legislation, amendments and repeals. It also sets out the title and commencement dates and includes interpretation provisions.[5]
2. Functions of key Health and Social Care Organisations
The following section identifies the functions and powers of the key organisations at the heart of the Northern Ireland Health and Social Care system. Through identifying the specific clauses in the HSC (Reform) Bill, a number of pertinent issues are raised relating to how the legislative provisions could potentially affect the different organisations’ execution of their functions and the interaction between the bodies in delivering HSC services.
Clauses 2-6 Department of Health Social Services and Public Safety (DHSSPS)
Clauses 2-6 within the Health and Social Care (Reform) Bill set out the general duties, powers and priorities of the DHSSPS. For instance, clause 2 delineates the Department’s general duty ‘to promote…an integrated system of health care designed to secure improvement in the physical and mental health of people in Northern Ireland.’[6] Moreover, clause 2, subsection 3 also states that the Department must among other things,
…develop policies to secure the improvement of the health and social well-being of, and to reduce health inequalities between, people in Northern Ireland.[7]
…allocate financial resources available for health and social care, having regard to the need to use such resources in the most economic, efficient and effective way.[8]
…secure commissioning and development of programmes and initiatives conducive to the improvement of the health and social well-being of, and the reduction of health inequalities between people in Northern Ireland.[9]
…monitor and hold to account the Regional Board, RAPHSW, RSSO and HSC Trusts in the discharge of their duties.[10]
A primary objective within the DHSSPS’s proposals to restructure the health and social care system is the significant reduction in size, including personnel of the DHSSPS. The aim is to create a smaller organisation to support the Minister ‘in advising on and reviewing policy, legislation, standards, priorities and targets and in all aspects of business in the Assembly, the Executive, the North-South Ministerial Council and the British Irish Council.’[11]
The intention is to ensure that the Department becomes,
…more sharply focused on its responsibilities for serving the devolved administration…driving performance primarily by setting strategic targets, tracking outcomes and applying strategic change levers to ensure that the health and social care system maintains a focus on delivering those outcomes, rather than being involved in the day-to-day operational management, which would be the role of the new RHSCB.[12]
Commenting on the Health and Social Care (Reform) Bill, Children in Northern Ireland (CiNI) highlight the need for the DHSSPS to include the commitment to reduce health and ‘social well-being’ inequalities between people in Northern Ireland. Currently within the HSC Bill there is only a commitment to reduce health inequalities.[13] Consideration may be given to the inclusion of legislative provision to commit each of those HSC organisations responsible for the commissioning and delivery of health and social care services to the reduction of health and social well-being inequalities between people in Northern Ireland.
It is worth noting that, as the Bill stands, the Department, amongst other things has a duty to develop policies to reduce health inequalities rather than to actually reduce these inequalities themselves.
Meanwhile, CiNI’s response also raises an issue around the need for clarity relating to the DHSSPS’s general duty under clause 2, section 3, paragraph (c) to allocate resource in the most economic, efficient and effective way. CiNI contend that it is unclear as to whether a hierarchy exists in relation to these important criteria and argue that ‘primary consideration must be given to ensuring that effective health and social care services are available to all.’[14]
Departmental interference
Complementing the DHSSPS’s responsibility to ‘monitor and hold to account’ the other key organisations within the health and social care system, there is a legislative requirement set out in clause 5 for the Department to prepare a “framework document”. Significantly, this document sets out the main priorities, objectives, guidance and other matters for each health and social care body in connection with the carrying out of its functions. Under the same clause, the Department must keep the framework document under review and if required, revise it.
Consequently, the legislative provision within clause 5 raises a number of questions around the Department’s potential to intervene in the functions of other key health and social care organisations. Naturally, the DHSSPS retains the statutory authority to intervene in the execution of the responsibilities of key organisations such as the RHSCB, the RAPHSW, the Trusts and the RSSO – without consultation in instances where urgent action is required.
However, the Department’s power to prepare a ‘”framework document” ‘setting out in relation to each health and social care body the main priorities and objectives of the body in carrying out its functions’[15] raises concerns around the potential for the DHSSPS to unnecessarily intervene in the operation of other HSC organisations. While clause 5, subsection 5 states that, ‘in preparing the framework document, or any revision of it which appears to the Department to be significant’, the legislation could clarify the Department’s responsibility to ensure that the document cannot be employed simply as a controlling mechanism on the activities of other HSC organisations.
One HSC organisation where the unnecessary interference of the DHSSPS would be particularly concerning is the proposed Patient and Client Council (PCC). In its important role providing the ‘patient voice’ within the HSC system, representing the interests of the public and seeking redress from the DHSSPS, the RHSCB and the Trusts, it would be helpful for the legislative provision within the Bill to be clarified around the preparation of the framework document in relation to the PCC.
Capital Investment
In relation to the wider issue of capital development and investment, it is worth considering the view expressed within the consultation response submitted by the Southern Health and Social Care Trust,
The Department’s role in capital investment is not clearly defined…The Trust believes that the relationship between pubic, private and independent sector in developing capital schemes need closer working between the Department, RHSCB, the Strategic Investment Board, Health Estates and the Trusts.[16]
Without an explicit reference to the DHSSPS’s function in the area of capital development, consideration may be given to the inclusion of legislative provision within the HSC (Reform) Bill, which clearly defines the role of the Department, and its relationship with the other agencies mentioned above in the procurement of capital assets.
Clauses 7-8 Regional Health and Social Care Board (RHSCB)
Clauses 7 and 8 provide for the establishment and functions of the new Regional Health and Social Care Board, which effectively will assume the powers of the existing 4 Health and Social Services Boards (whose dissolution and transfer of functions is provided for under Clauses 1 and 24 respectively) as well as ‘any other functions which the Department directs it to exercise.’[17]
It is important to note that there is also legislative provision for the RHSCB within Schedule 1 of the Bill setting out the constitution of the body.
The core functions of the RHSCB in relation to the performance management of the trusts and the commissioning of health and social care services is provided for within clause 8, subsection 2:
The Regional Board must exercise its functions with the aim of-
(a) improving the performance management of HSC trusts, by reference to such indicators of performance as the Department may direct; and
(b) establishing and maintaining effective systems-
(i) for managing the performance of HSC trusts;
(ii) for commissioning health and social care;
(iii) for ensuring that resources are used in the most economic, efficient and effective way in commissioning such care[18]
Additionally, in relation to the RHSCB’s commissioning function, clause 8, section 3 outlines the following provision:
The Regional Board must in respect of each financial year prepare and publish a document (“the commissioning plan”) setting out such details as the Department may direct concerning-
(a) the health and social care which the Board is to commission in that year;
(b) the costs to be incurred in that regard;
and in drawing up the commissioning plan the Board must consult RAPHSW and have due regard to any advice or information provided by it.[19]
Reflecting the close working relationship between the RHSCB and the DHSSPS, subsection 6 states that,
It is the duty of the Regional Board to carry out its functions in the manner which it considers is best calculated to discharge the Department’s general duty under section 2(1).[20]
It is also worth noting that clauses 10 and 11 make provisions for the Regional Board in relation to conferring powers to give directions and guidance to HSC trusts and the provision of information by the RHSCB to the trusts.
Managing performance of non-state/private sector providers
A potentially significant omission in the clauses providing for the core functions of the RHSCB is the management of performance in relation to service providers other than HSC trusts. As the primary organisation responsible for commissioning services within the health and social care system, it would seem logical for the Regional Board to monitor the performance of non-state providers. This is particularly salient within the current health policy environment where the Department are increasingly considering employing the services of private sector companies (including construction and facilities management) in the area of capital development and healthcare companies in an effort to reduce waiting times in key treatment areas.
Duplication
There are a number of recurrent issues that emerged from the DHSSPS’s HSC reform proposals relating to the establishment and functions of the new Regional Board. One overriding point highlighted throughout a number of responses was that there should be clarity of roles, responsibilities and governance arrangements throughout the new health and social care system. In relation to the Bill, there is evidence of possible duplication in the area of commissioning responsibilities performed by the DHSSPS and the RHSCB. For instance, clause 2, subsection 3 states that,
The Department must-
…secure the commissioning and development of programmes and initiatives conducive to the improvement of the health and social well-being of, and the reduction of health inequalities between, people in Northern Ireland.[21]
In comparing this key responsibility of the DHSSPS with the RHSCB’s core function to ‘establish and maintain effective systems for commissioning health and social care’ it is possible to argue that the proposed legislation could produce duplication in this key area of service commissioning.
Clause 9 Local Commissioning Groups
Reflecting the Department’s HSC reform proposals, the Bill provides for the RHSCB to be responsible for the appointment of Local Commissioning Groups (LCGs). Clause 9, subsection 1 states that, ‘The Regional Board shall in accordance with paragraph 7 of Schedule 1 appoint a prescribed number of committees to be called “Local Commissioning Groups”.’[22]
Under the Department’s proposals, the RHSCB ‘would be ultimately accountable for the outcomes of commissioning functions discharged by LCGs. This includes the statutory responsibility to contain expenditure within allocated resources. The Chair of each of the LCG would be accountable to the Chair of the RHSCB.
In relation to the functions of the LCGs, Clause 5 states that,
Each Local Commissioning Group must exercise its functions with the aim of-
(a) improving the health and social well-being of people in the area as regards which the Local Commissioning Group exercises its functions;
(b) planning and commissioning health and social care to meet the needs of people in that area;
(c) securing the delivery to people in that area of health and social care is efficient, co-ordinated and cost-effective;
(d) improving the availability and quality of health and social care in that area.[23]
It is also important to note that, ‘in connection with the exercise of these functions [each] Local Commissioning Group must consult RAPHSW and have due regard to any advice or information provided by it’.[24]
Greater autonomy in executing commissioning function
A significant number of the responses to the DHSSPS’s HSC reform proposals supported the role of the RHSCB in establishing the Local Commissioning Groups. These proposals included,
- The RHSCB would ultimately be accountable for the outcomes of commissioning functions discharged by LCGs;
- The Chair of each LCG would be accountable to the Chair of the RHSCB;
- The RHSCB would approve each LCGs Annual Commissioning Plan and would be responsible for monitoring their performance.[25]
Conversely, Professor Derek Birrell, University of Ulster commented that,
Local Commissioning Groups are proposed which have no independent status or autonomy. They can be overruled by RHSCB and are really local advisory groups in terms of public administration systems. They are not commissioning organisations in the sense of primary care trusts in England and the actual term is misleading.[26]
Meanwhile, in their submissions to both the DHSSPS and the HSSPS Committee’s consultation exercises, the Eastern Health and Social Services Board (EHSSB) stated that,
With devolved responsibility must come devolved budgets to allow the LCGs to address the needs of the local population within coherent regional policy and strategy frameworks. To that end, there should be a Senior Finance Office on the Board of the LCG. LCGs could then properly assure the Board of financial propriety and regularity.[27]
Consideration may be given to inserting more detail around the specific functions including areas of commissioning responsibility under the control of Local Commissioning Groups. Greater clarity could assist in improving partnership working between the RHSCB and the LCGs and ensure that LCGs are fully engaged and consulted in regional decisions which affect their local area of responsibility. Providing more detail within the proposed legislation could provide a stronger platform enabling LCGs to develop into effective local commissioning organisations and support the objective of enhancing the devolution of health and social care in Northern Ireland.
Consultation
While there is an obligation for the LCGs to consult with the RHSCB and the RAPHSW in developing and finalising local commissioning plans coupled with a duty to cooperate with the PCC, there is no requirement on the part of LCGs to consult with the people within their locality and for whom they commission and health and social care services. Therefore, consideration may be given to the inclusion in the Bill of legislative provision making it a statutory requirement for LCGs to engage in consultation exercises as an integral component in the coordination of local commissioning plans.
Membership
Within the HSC (Reform) Bill there are two significant references in relation to the membership of Local Commissioning Groups. These are located within clause 9, sub-sections 6 and 7. According to sub-section 6, paragraph (a):
Regulations may-
Make provision for the membership of Local Commissioning Groups.[28]
Meanwhile, section 7 states that,
Before making regulations under subsection (6), the Department must consult the Regional Board.[29]
The HSC (Reform) Bill lacks detail in relation to the composition of the membership of the LCGs including the number of representatives from the health professions or the number of publicly elected figures. Consideration may therefore be given to the inclusion of legislative provision to clearly state the number of representatives from the health professions, elected local representatives and other groups as outlined within the DHSSPS’s proposals.[30]
In their response to the HSSPS Committee’s consultation exercise, the Pharmaceutical Society of Northern Ireland (PSNI) expressed their view that given the significant ‘breath and strength of stakeholder opinion concerning the constitution of Local Commissioning Groups’ the proposed legislation could be reworded as follows:
Before making regulations under subsection 6, the Department must consult the Regional Board, stakeholders and the public.[31]
Meanwhile, the BMA(NI) in its response to the HSSPS’s Committee’s consultation exercise have voiced their opinion that ‘elected local representatives should not be included on Local Commissioning Groups.’ According to the organisation,
This is not to minimise the importance of elected local representatives as the BMA(NI) fully supports the principle that Local Commissioning Groups and local government should work jointly on local health improvement plans. The BMA(NI) believes that the strong scrutiny and accountability role of Local Councils, working alongside the new PCC, may be eroded if elected council representatives are on the LCGs. There is also a concern regarding the practicality of having four local representatives on each of the LCGs. If for instance the Northern Trust has one LCG, it will cover eight current local government areas.[32]
Clauses 12-13 The Regional Agency for Public Health and Social Well-Being (RAPHSW)
Clauses 12 and 13 provide for the creation of the Regional Agency for Public Health and Social Well-Being (RAPHSW) and sets out its key functions, which include health promotion and protection and a responsibility to cooperate with other key HSC organisations. These include working with the RHSCB and the LCGs in the commissioning of services at a regional and local level. The provisions within the Bill reflected the 3 key functions of the RAPHSW as delineated within the Department’s HSC proposals – health improvement, health protection and public health support to commissioning and policy development.
Clause 13, subsection 1 states that,
RAPHSW shall exercise on behalf of the Department-
(a) the health improvement functions mentioned in subsection (2), and
(b) the health protection functions mentioned in subsection (3).[33]
Subsection 2 outlines the health improvement functions as
(a) developing and providing, or securing the provision of, programmes and initiatives designed to secure the improvement of the health and social well-being of, and reduce health inequalities between, people in Northern Ireland; and;
(b) health promotion.[34]
Subsection 3 states that, ‘Those health protection functions are the protection of the community (or any part of the community) against-
(a) communicable disease, in particular by the prevention or control of such disease;
(b) other dangers to health and social well-being, including dangers arising on environmental or public health grounds or arising out of emergencies.[35]
Significantly, subsection 5 affirms that, ‘The Department may by order amend subsection (1) to (4) for the purposes of altering the functions of RAPHSW.’[36]
Sharing responsibility for the local public health agenda
A considerable number of responses to the DHSSPS’s reform proposals support the creation of a dedicated public health agency reflecting the Minister’s intention to place the public health agenda at the heart of the Health and Social Care system. Equally there are concerns that in creating one body it could result in the centralisation of the key functions of health promotion and health protection which according to Professor Derek Birrell, University of Ulster ‘is contrary to structures in the rest of the United Kingdom’.[37]
In their response, the Northern Ireland Council for Voluntary Action (NICVA) have expressed concern around the new Public Health Agency incorporating the public health functions and responsibilities that currently rest with the Boards and Trusts. They have pointed out that, consequently,
…responsibility for work on health improvement, health inequalities and community development will not lie with organisations commissioning and providing services. The LCGs and Trusts will have a responsibility to consult the RPHA on their plans but we would be concerned that this separation might weaken these areas of work because commissioners and providers will feel less obliged to mainstream health improvement and health inequalities issues into all their work. This would detract from, rather than strengthen, the public health agenda, especially at local level where good relationships and good practice current exist.[38]
These sentiments were shared in a number of the responses submitted by the different trusts. For example, the Southern Health and Social Care Trust (SHSCT) commented that,
It is important that in the design of the Regional Public Health Agency that it retains a locality sensitive model of working that can respond quickly and effectively to the needs of local communities to a more centrally driven strategic model that is driven largely by Departmental priorities.[39]
It goes on by highlighting the considerable expertise and experience built up in recent years within the trust in the delivery of public health services and promotion. Emphasising concern around the impact of removing the Specialist Health Improvement functions currently cited within the trusts the SHSCT response stated that,
The Trust has invested in the development of a high profile, integrated Promoting Well Being Department, which incorporates the specialist health improvement function combined with that of community development, the Health Action Zone and user involvement. The Trust believes that this unique combination of agendas add significant strength and value to the work of improving health and well being and reducing health inequalities.[40]
There is a statutory requirement on both the RHSCB and LCGs to have ‘due regard’ to the advice or information provided by the RAPHSW in the execution of their commissioning functions. However, there is no reference in the Bill with regard to direct cooperation between the trusts and the RAPHSW. To ensure the trusts’ considerable experience in public health service delivery is not jeopardised and to enhance collaborative working between regional and local HSC bodies, consideration may be given to include legislative provision requiring the RAPHSW to work closely with the trusts in the execution of its responsibilities.
Additionally, the Royal College of Nursing (NI) in their response to the HSC Bill highlight their concern that current legislative provision is ‘insufficiently robust and should be strengthened’ in relation to ‘partnership working’ between the commissioning bodies and the RAPHSW. They contend that,
…requiring the commissioning authorities merely to consult and have due regard to advice and information provided by RAPHSW may not secure the full integration of public health and commissioning that will be essential in order to give effect to the Minster’s objectives [to put the public health agenda at the heart of the HSC system].[41]
In their submission, they suggest that the wording of the relevant phrase within clause 8, section 3 should be amended to, “the Board must work in partnership with RAPHSW and be able to demonstrate that its commissioning plan reflects the priorities determined by RAPHSW.” In relation to Local Commissioning Groups, the RCN suggest amending clause 9, section 1 to ensure that LCGs “work in partnership with RAPHSW and be able to demonstrate that the exercise of its functions reflects the priorities determined by RAPHSW.”[42]
By making these changes the RCN argue that the relationships between the RAPHSW and the RHSCB and the LCGs will ‘become one of strategic partnership rather than simply consultation and advice…ensuring that public health is at the forefront of service design and delivery.’[43]
Clauses 16-17 The Patient and Client Council (PCC)
Clauses 16 and 17 reflect the Department’s decision to choose Option 1[44] within their HSC reform proposals to establish ‘a body corporate to be known as the Patient and Client Council’.[45]
According to Clause 17, subsection 1,
The Patient and Client Council has the following functions as respects the provision of health and social care in Northern Ireland-
(a) representing the interests of the public;
(b) promoting involvement of the public;
(c) providing assistance (by way of representation or otherwise) to individuals making or intending to make a complaint relating to health and social care for which a body to which this section applies is responsible;
(d) promoting the provision by bodies to which this section applies of advice and information to the public about the design, commissioning and delivery of health and social care;
(e) such other functions as may be prescribed.[46]
In addition to the functions of the PCC, clause 18 of the Bill provides for a duty on other health and social care organisations to cooperate with the PCC in the execution of its responsibilities.
Strengthening the powers of the PCC
Clause 18, section 2, paragraph (a) states that ‘a body must consult the Patient and Client Council with respect to such matters, and on such occasion, as the body considers appropriate, having regard to the functions of the Council.’[47]
Children in Northern Ireland (CiNI) have raised concerns around the potential scope of HSC organisations to ‘significantly undermine the spirit of cooperation, leaving it entirely to the discretion of the health and social care bodies to decide on what and when they will cooperate with the Council.’[48] Given these concerns, consideration may be given to the rewording of clause 18 to include ‘due regard’ in relation to cooperating with the PCC thus placing a greater obligation on all the HSC organisations.
3. Other relevant clauses and issues
Public Private Partnerships (Clause 22)
Clause 22 enables the Department, and certain health and social care bodies to form, or participate in forming, public-private partnerships to provide facilities or services for the promotion or provision of health and social care.[49]
Performance Management
One of the notable deficiencies within the Northern Ireland health service identified by the 2005 Appleby review was the distinct absence of an explicit performance management system. Such a system within the health service was regarded as pivotal to achieving improvements in efficiency, effectiveness and responsiveness. Appleby was critical of the existing performance management structures in place at the time of the review contributing to an impression of ‘a system lacking urgency, or general drift, and a consequent frustration amongst many in the services – at all levels – with the relative lack of improvement in performance’.[50] He contended that the current performance management system was devoid of the clear and effective structures, information and most importantly incentives – both rewards and sanctions – at individual, local and Northern Ireland organisational levels to encourage innovation and change.
Beyond the provision for the Regional Board to achieve the aim of ‘improving the performance of HSC trusts, by reference to such indicators of performance as the Department may direct’ and ‘establish and maintaining effective systems for managing the performance of HSC trusts’ – very little information is provided regarding clear performance enhancing mechanisms or structures. The importance of ensuring robust performance management structures, clear information and effective incentives are embedded within the HSC system is highlighted in the consultation response submitted by the RQIA.
It is essential that a performance management framework is developed and put in place [which] clarifies the duties of the DHSSPS, RHSCB, RAPH (RAPHSW), HSC Trusts, Agencies and other bodies (including RQIA)….Clarity on the arrangements for the commissioning, performance management and governance arrangements for primary care family practitioner services is also required.[51]
Those recommendations that emerged from the Appleby review which feature in the proposals and the HSC (Reform) Bill include the operation of a form of separation between commissioners and providers of services and the establishment of ‘a single pan-Northern Ireland commissioner’ in the form of the proposed RHSCB. The Appleby review also highlighted a number of other mechanisms or ‘performance levers’ which could underpin a more robust performance management regime within the HSC system. These included,
- serious, long-term target setting coupled with rewards and sanctions at organisational and individual levels;
- an ‘activity-based prospective reimbursement system’ for providers (similar to ‘Payment by Results’ currently employed within the English health system) with tariff setting used to drive improvement in efficiency and selective increases in activity to meet pan-service goals;
- careful expansion of patient choice - not similar to the way choice between Trusts competing within a market-based system in England but ‘from the patient’s point of view, a more formalised and embedded process of choice (not just hospital, but over the myriad of decisions that are taken throughout the system which affect a patient’s care) can improve patient satisfaction and service responsiveness;
- General Practitioner (GP) involvement – despite previous rejection of GP fundholding, ways of both strengthening the involvement of General Practitioners in the system and as part of a devolution strategy for commissioning secondary care services, thought should be given to the practical involvement of GPs in the purchasing of care.[52]
The development and implementation of a robust performance management regime integrated into the commissioning functions of the Regional Board and LCGs will be critical within the new HSC system. Better monitoring of contract performance and the imposition of financial sanctions in the event of organisational failure on the part of the service provider would help to focus the attention of Trust management.
ANNEX
35 Clauses of the Health and Social Care (Reform) Bill
Clause 1: Restructuring of administration of health and social care
2: Department’s general duty
3: Department’s general power
4: Department’s priorities and objectives
5: The framework document
6: Power of Department to give direction to certain bodies
7: The Regional Health and Social Care Board
8: Functions of the Regional Board
9: Local Commissioning Groups
10: Power of Regional Board to give directions and guidance to HSC trusts
11: Provision of information, etc. to Regional Board by HSC trusts
12: The Regional Agency for Public Health and Social Well-Being (RAPHSW)
13: Functions of the RAPHSW
14: The Regional Support Services Organisation
15: Functions of RSSO
16: The Patient and Client Council
17: Functions of the Patient and Client Council
18: Duty to co-operate with the Patient and Client Council
19: Public involvement and consultation
20: Public involvement: consultation schemes
21: Duty on HSC trusts in relation to improvement of health and social well-being
22: Public-private partnerships
23: Schemes for transfer of assets and liabilities
24: Transfer of functions of Health and Social Services Boards
25: Transfer of functions of the Mental Health Commission
26: Transfer of functions of Central Services Agency
27: Amendment of statutory and other references to dissolved bodies, etc
28: Dissolution of special agencies
29: Orders, regulations, guidance and directions
30: Further provision
31: Interpretation
32: Minor and consequential amendments
33: Repeals
34: Commencement
35: Short title
[1] Ministerial statement to the Northern Ireland Assembly – 4 Feb 2008.
[2] Health and Social Care (Reform) Bill (2008) Exploratory and Financial Memorandum, paragraph 4.
[3] Children in Northern Ireland (CiNI) Consultation Response.
[4] A list of the headings of the 35 Clauses is provided in the Annex.
[5] Health and Social Care (Reform) Bill (2008) Explanatory and Financial Memorandum: 2.
[6] Clause 2, subsection 1, Paragraph (a), Sub-Paragraph (i).
[7] Clause 2, subsection 3, Paragraph (a).
[8] Clause 2, subsection 3, Paragraph (c).
[9] Subsection 3, Paragraph (g)
[10] Subsection 3, Paragraph (h).
[11] DHSSPS (2008) Proposals for Health and Social Care Reform, DHSSPS: 23.
[12] DHSSPS (2008) Proposals for Health and Social Care Reform, DHSSPS: 23.
[13] See clause 2, section 3, paragraph (a).
[14] Children in Northern Ireland’s (CiNI) consultation response to the Health and Social Care (Reform) Bill.
[15] Clause 5, subsection 1, paragraph (a).
[16] Southern Health and Social Trust consultation response.
[17] Health and Social Care (Reform) Bill (2008) Explanatory and Financial Memorandum: 4
[18] Clause 8, subsection 2 (a) and (b).
[19] Clause 8, subsection 3.
[20] Clause 8, subsection 6.
[21] Clause 2, subsection 3, paragraph (g).
[22] Clause 9, subsection 1.
[23] Clause 9, subsection 5.
[24] Clause , subsection 4, paragraph (b), sub-paragraph (i).
[25] DHSSPS (2008) Proposals for Health and Social Care Reform, DHSSPS: 20-21.
[26] Professor Derek Birrell Consultation response.
[27] Eastern Health and Social Services Board Consultation response to the DHSSPS’s HSC reform proposals and the HSSPS Committee’s consultation exercise on the HSC (Reform) Bill.
[28] Clause 9, sub-section 6, paragraph (a).
[29] Clause 9, sub-section 7.
[30] See DHSSPS (2008) Proposals for Health and Social Care Reform, DHSSPS: 19-20.
[31] Pharmaceutical Society of Northern Ireland (PSNI) Consultation response to the HSC (Reform) Bill.
[32] BMA(NI) Consultation response to the HSC (Reform) Bill.
[33] Clause 13, subsection 1.
[34] Clause 13, subsection 2.
[35] Clause 13, subsection 3.
[36] Clause 13, subsection 5.
[37] Professor Derek Birrell’s Consultation response to the DHSSP’s HSC reform proposals.
[38] NICVA Consultation response.
[39] Southern Health and Social Care Trust response to the DHSSP’s HSC reform proposals.
[40] Southern Health and Social Care Trust response to the DHSSP’s HSC reform proposals.
[41] Royal College of Nursing (NI) Consultation response to the HSC (Reform) Bill.
[42] Royal College of Nursing (NI) Consultation response to the HSC (Reform) Bill.
[43] Royal College of Nursing (NI) Consultation response to the HSC (Reform) Bill
[44] See DHSSPS (2008) Proposals for Health and Social Care Reform, DHSSPS: 40.
[45] Clause 17, subsection 1.
[46] Clause 17
[47] Clause 18, section 2, paragraph (a).
[48] Children in Northern Ireland (CiNI) response to the HSC Reform Bill.
[49] Health and Social Care (Reform) Bill (2008) Explanatory and Financial Memorandum: 6.
[50] Appleby, J. (2005) Independent Review of Health and Social Care Services in Northern Ireland, August: 10.
[51] Regulation Quality and Improvement Authority (RQIA) Consultation response.
[52] Appleby, J. (2005) Independent Review of Health and Social Care Services in Northern Ireland, August: 11-12.
NILGA
Committee for Health, Social Services and Public Safety - Briefing Paper 5th June 2008
Context
Programme for Government Commitments
Principles: Leadership, Partnership, Rising Standards, Fair Outcomes
A Peaceful, fair and prosperous society
- Deliver modern, high quality and efficient public services (move focus away from administrative boundaries to the citizen)
- Promote tolerance, inclusion health and wellbeing
- Protect and enhance our environment and natural resources
- Invest to build our Infrastructure
Our Vision for Local Government
Aligns with that set out in the Minister’s Statement
- Innovative and modern approach supported by a new partnership relationship between local and central government
- Modern citizen centred public services and greater efficiency and effectiveness
- An appropriate suite of functions
- Defined Roles: Central -Policy and Strategy / Local- Delivery
- Partnership Approach - provide greater integration (Beyond Boundaries)
Key Objective (1)
Democratisation; NILGA welcomes the proposed wider democratisation of the existing health structures, through a stronger role for political representatives.
Democratisation
NILGA would highlight that it is necessary take a strategic look at how locally elected members are represented within the various structures, to avoid both duplication and confusion and ensure effectiveness and consistency of approach. This is of increasing importance in the changing context of new Central local relationships and Community Planning Relationships and/or new Local Area Agreements (A area based contract between local and central government). We would encourage the Minister to have regard to;
- The full NILGA support the role of public representatives on new bodies
- Processes
- Role Clarity (Board member/Public representative/Council Representative)
- Support structures for members
- Reporting structures if required
- Mechanisms for appointing members
- The wider emerging arrangements across central government
- NB – A paper is being produced for the SLB in regard to this issue and should be available in the next 8 weeks.
Key Objective (2)
Call for Co-terminosity or other support arrangements to facilitate mechanisms for joint working.
Coterminosity / Better Outcomes for the Citizen
- NILGA call for full analysis to provide Co-terminosity or alternative support arrangements. (Only 3 Councils are outside the Boundaries (Limavady, Newry and Mourne, and Dungannon)
- Provides significant opportunities for developing a stronger more ‘partnership’ orientated relationship in the context of the proposed new statutory Central/Local relationship arrangements.
Key Objective (3)
Explore opportunities for Community Planning.
Community Planning
- NILGA welcomes the development of legislation on the community planning process.
- NILGA believes that for the process to be effective there must be a strong scrutiny role with a statutory obligation upon other agencies to participate and be locally accountable for example Regional Public Health Agency.
- NILGA would seek to ensure the work of the new agency will support the development and delivery of the local community plan and will fit with other priorities within the local area. Highlight the need for local arrangements alongside relationships at the regional level.
- We would welcome the exploration of innovative delivery approaches such as co-locating local PHA teams within Councils, or providing a joint appointment arrangement.
- A local community plan must be influenced and established in the light of regional policy, however the process will be ineffectual if inadequate regard is given to local priorities.
- Guidance must also be agreed so that effective mechanisms of participation are ensured for all other stakeholders including the Private and Community/Voluntary sectors. This must also include cross/inter departmental working across both central and local government regarding all cross-cutting issues.
- In relation, to Patient Client Councils we would note the necessity of the involvement of these councils in the development process for Community Plans.
Key Objective (4)
Discuss the proposed new structures and seek to ensure that local government is fully involved in the consideration and development of more detailed arrangements.
- Ask the Committee to consider increasing the number of elected representatives on Local Commissioning Groups (LCG) to ensure that elected representatives make up no less than 50% of the members of each LCG.
- We would welcome the consideration of a role for councils in scrutinising the delivery of health services, and would suggest that scrutiny mechanisms should be put in place as part of these proposals.
The Mental Health Commission
1.1 What is Our Purpose?
The Commission has a duty to keep under review the treatment and care of people in Northern Ireland who have a learning disability or who have mental health needs. The Commission’s authority is based on the Mental Health (Northern Ireland) Order 1986 (the Order).
1.2 What Do We Do?
The Commission provides a number of key services in meeting this duty:
- Multi-disciplinary teams of Commission members undertake announced and unannounced visits to learning disability hospitals, psychiatric hospitals and community facilities.
- To bring to the attention of the Department, the Secretary of State, an HSS Trust Board or any other body or person any matter concerning the welfare of patients which the Commission considers ought to be brought to their attention.
- Where it thinks fit, refer to the Mental Health Review Tribunal the case of any patient who is liable to be detained in hospital or subject to guardianship under this Order.
- At any reasonable time visit, interview and medically examine in private any patient in a hospital, private nursing home, residential care home, voluntary home or nursing home or any person subject to guardianship under this Order.
- The Commission appoints doctors who can legally detain people in hospitals.
- The Commission reviews legal documentation regarding detention and guardianship to determine if Trusts have complied with the Order.
- The Commission reviews all serious untoward events involving people with mental health needs or a learning disability.
- The Commission reviews treatment plans of patients detained for longer than three months. These are scrutinised for clinical acceptability and evidence of consent or a second opinion.
- The Commission arranges for the appointment of independent doctors for second opinions for people who require specified treatment, such as electroconvulsive therapy.
1.3 Who Are We?
The Commission comprises a part-time Chairperson and 16 sessional Commission members, supported by 7 full-time equivalent administrative staff.
1.4 Who Funds Us?
The Department of Health, Social Services and Public Safety provide the Commission’s funding. The funding drawn down from the Department during the 2007-2008 financial year was £621,709.
1.5 Where Are We?
The Commission’s headquarters is based in leased premises at Lombard House, Lombard Street, Belfast, BT4 1NY, telephone 028 90436760, Fax 028 90333297, email mhc@dhsspsni.gov.uk.
The Health and Social Care (Reform) Bill
2.1 On 23rd June 2008 the Minister introduced the Health and Social Care (Reform) Bill into the Assembly. It is the Minister’s intention to transfer the functions of the Mental Health Commission to the RQIA, with effect from 1st April 2009.
2.2 The Commission submitted a response to the Consultation on the Proposals for Health and Social Care Reform. The response stated that the Commission should remain as a separate, independent body as in other jurisdictions mainly because:
2.3 People with a learning disability or mental health needs are vulnerable and need their own independent watchdog that can protect and advocate for their human rights.
2.4 Mental Health and Learning Disability have traditionally been considered “Cinderella” services that have suffered the most from the lack of funding. The Commission, placed within a wider HSS body could suffer from a lack of funding, given that the work of the Commission will only constitute 15% of RQIA overall work. Therefore, there is a very significant risk that mental health and learning disability service users’ interests could become marginalised in such a body.
2.5 The Commission’s focus is on people and not solely on measurable standards and services. HSS bodies that focus on measurable standards and services may overlook the real issues of concern that can’t easily be measured, such as quality of life.
2.6 HSS professionals can become complacent, reactive and accepting of existing systems, environmental conditions and the ways that things are done. A key strength of the Commission is the regular input of lay members with different experiences and value bases to challenge the status quo and the way things are done. In addition, another key strength is the varied background of members including users, carers, social work, nursing, management, legal, general medical practitioner, psychology and allied health professional.
2.7 The Commission is independent of health and social services and is seen by our users as an independent arbitrator. This independence would be diluted, or lost, if the Commission were a part of another HSS body.
Transfer of Functions to the RQIA
3.1 A Paper on the future of the Mental Health Commission was prepared by the Legal Issues Sub-group 2 (Report of the Review of Mental Health Commission Working Group, September 2004), as part of the Bamford Review. The Working Group determined that there was a very clear need for an independent watchdog body to monitor and regulate the services provided to people with mental health or learning disability. The Working Group recommended that the future watchdog body should become an integral arm of the Regulation and Quality Improvement Authority, known as the Mental Health Commission, but as a stand alone unit within the RQIA. It is the view of the Commissioners that this approach would be the most acceptable alternative to retaining its full independent status.
3.2 There are several specific functions and the way in which those functions are performed, is the crux of what the Mental Health Commission considers to be extremely important for the RQIA and Mental Health and Learning Disability Service Users. These are:
3.3 Visiting detained patients and interviewing detained patients in private, and having the necessary breadth and depth of expertise of mental health care such that those undertaking visits and inspections are able to identify shortcomings or difficulties in mental health and learning disability services.
3.4 Engaging mental health and learning disability service users actively as full partners in the enterprise of health and social care assessment, monitoring and inspection;
3.5 Adequate organizational and personal accountability for monitoring and reporting on the needs and rights of detained patients;
3.6 Statutory notifications of admissions, discharges and deaths of detained patients, and other relevant information;
3.7 Ensuring adequate and appropriately trained staff.
3.8 Having an overarching principle of equality and human rights, focussing at all times on the civil, legal and human rights of patients;
Post April 2009 Recommendations
4.1 The Mental Health Commission would propose that the following are requirements which should be met by the new organisation:
4.2 The Commission’s budget should be protected within the RQIA’s overall spend to ensure that the allocation is used to develop and improve services for this client group. In particular, a strong service user and carer input must be developed and a reference group of service users/carers representing the various sub-specializations should be set up. This would be ensured if the Mental Health & Learning Disability programme becomes a “stand alone” section within the body of the RQIA.
4.3 The appointment of full time staff – solely dedicated to Mental Health and Learning Disability should be a priority for RQIA and will provide dedicated professional advice to the range of issues that will arise.
4.4 It is important that the functions of the Mental Health Order are represented in RQIA’s name and/or logo. Service users must be able to quickly identify the Organisations they want to contact for help. With the Mental Health Commission it is clear, but the title RQIA gives no indication that this organisation deals with the Mental Health Order.
4.5 The Board of RQIA must have membership with a Mental Health and Learning Disability background and familiarity with the Mental Health Order.
4.6 A position of Deputy or Vice Chair to the RQIA should be created with the postholder having in addition to deputising for the Chair specific responsibility for Mental Health & Learning Disability Services.
4.7 In the event that there is not a stand alone Unit created to deliver the transferred functions, there must be an agreed Model of Delivery arrived at through joint discussion with RQIA and Commissioners.
4.8 An External Relations function must be developed, to pick up on, comment and raise issues of importance that impacts on service delivery, identify trends or draw attention to issues of concern.
4.9 There should be a user/carer representation, for Mental Health & Learning Disability on the Board of RQIA.
The British Medical Association
(Northern Ireland)
Briefing Paper to the Northern Ireland Assembly Health, Social Services and Public Safety Statutory Committee on the Health & Social Care Reform Billl, 02 October 2008.
Contents
Introduction
Summary
Getting to the Health & Social Care (Reform) Bill
Purpose and Function of the Health & Social Care (Reform) Bill
The Health (Miscellaneous Provisions) Bill Proposals
Introduction
The British Medical Association is the professional organisation and trade union for doctors in the UK. Across the UK more than three out of four practising doctors, and the majority of medical students, are members. The BMA office in Northern Ireland (BMA(NI)) is based in the Old Gasworks in Belfast and supports over 4,700 members from every branch of the medical profession in Northern Ireland.
The BMA is the voice of the medical profession - putting across to politicians, the public and the press the profession’s collective views on a wide range of subjects including public health, medical ethics and the state of the NHS.
The BMA(NI) welcomes the opportunity to give evidence to the Assembly Health Committee on the Health (Miscellaneous Provisions) Bill.
Summary
The BMA(NI) has examined the Health and Social care (Reform) Bill and wishes to state the following
1. The BMA(NI) welcomes the Bill as the progression of Phase 2 of the Review of Public Administration (RPA) in health as it has the potential to improve the lives of many people in Northern Ireland via a more efficient and less bureaucratic healthcare system, by the consequent release of resources to frontline patient care.
2. The proposed Regional Health and Social Care Board (RHSCB) is welcome. The BMA(NI) has long had the policy objective of the reduction of the number of Boards in Northern Ireland.
3. The BMA(NI) supports the slimming down of the Department of Health Social Services and Public Safety Northern Ireland (DHSSPSNI) and looks forward to savings from a reduction in bureaucracy being released to frontline patient care. It is essential that such savings are audited and that the Department communicates with HSC organisations and stakeholders on how these savings will be redistributed to frontline patient care. This must be a transparent process.
4. The BMA(NI) welcomes, with reservations, the creation of a new Regional Support Services Organisation (RSSO). A single centralised support service to provide a range of Shared Services was the recommended option in the BMA(NI) response to the consultation - Transformation of Business Services in Health and Social Care 2007. The size and bureaucracy of this support function is, however, a concern. The BMA(NI) would hope that this huge bureaucracy is structured in a way that is ‘flat’ and ‘divisionalised’, that is to say there should be a streamlined hierarchy with only a few managers. The provision of any out sourcing of work must be subject to the application of stringent business cases and progressed in a transparent and open manner.
5. The Regional Agency for Public Health and Social Well-being (RAPHSW) and the priority given to public health in the new structures are welcome in principle. It is vital that the role and functions of public health doctors are enhanced and backed up by the necessary staffing levels and support. The RAPHSW will need to interface significantly with the Department, the RHSCB, the RSSO and Trusts. It is essential that bureaucracy is minimised within the RPHA and between such organisations
6. There should be no clash between the Director of Public Health and the Chief Medical Officer. There must be clarity about the relationship of the advisory roles of the Director of Public Health and the Chief Medical Officer to the Minister.
7. The BMA(NI) has concerns about the lack of engagement with public health doctors by the Public Health Work Streams project team. The mechanism used currently does not compare with the mechanism used with the previous consultation process for workstreaming in terms of transparency and staff involvement. The mechanism for selecting people for different work streams is not clear. On its own this would, perhaps, not be terribly important but there have been constraints put upon the ability of those selected to consult fully with their colleagues. In particular they have not been allowed to share relevant documentation. There appears to be no logical explanation for this, as it could probably be obtained under a freedom of information request. It does cause a lot of suspicion and resentment and does not allow open and transparent working.
8. The BMA(NI) welcomes one Patient Client Council (PCC) which should be effectively resourced, in terms of role, personnel and finance with local offices in the new Trust/LCG/Council geographic areas.
9. The BMA(NI) has a major concern over the top-down approach to managing commissioning and believes that an opportunity may be lost to create local community based commissioning arrangements, at the level of groups of GP practices or individual practice level.
10. Commissioning is about assessing, prioritising and commissioning according to clinical need. It must be evidence based and decisions taken by those with the appropriate level of expertise.
11. The BMA(NI) strongly believes that any commissioning body that wishes to have General practitioner involvement must have the freedom to place or move contracts and be free to commission services as long as they operate within the regional strategic framework.
12. The BMA(NI), and its General Practitioner Committee, is of the opinion that elected local representatives should not be included on Local Commissioning Groups. This is not to minimise the importance of elected local representatives as the BMA(NI) fully supports the principle that Local Commissioning Groups and local government should work jointly on local health improvement plans. The BMA(NI) believes that the strong scrutiny and accountability role of Local Councils may be eroded if elected council representatives are on the LCGs. There is also a concern regarding the practicality of having 4 local representatives on each LCG. If for instance the Northern Trust has one LCG it will cover 8 current local government areas.
13. The BMA(NI) has consistently called for more powers for local councils, especially with regard to the power of well being and community planning.
Getting to the Health & Social Care (Reform) Bill
The Health and Social Care (Reform) Bill is a major part of the implementation of the overall Review of Public Administration (RPA), which began in 2002[1]. There have been a number of overarching consultations on the RPA[2],[3] to which the BMA(NI) have responded[4].
The BMA(NI) responded to the proposed Health and Social Services (Reform) (NI) Order 2007 in April 2007 and also responded[5] to the proposed legislation Proposals for Health and Social Care Reform consultation[6] published in February 2008.
The BMA(NI) now welcomes the opportyunity for the Health and Social Care (Reform) Bill to be fully debated witnin the devolved adminiatration.
It is an extremely important piece of legislation as it will affect service delivery, healthcare workers including doctors, patients and the public.
To put this all in context, the reform of the health and social care system should put in place structures which will provide patient-centred, professionally-led health services.
The health service needs to be patient centred to ensure the patient’s needs are met to as high a standard as possible. The service needs to be professionally led to ensure that the clinical decisions required are made so that the right patient can receive the right service at the right time in the right location. Professionally led services will involve frontline staff helping to continually evaluate provision frameworks to improve best practice. This will ensure the evolution of an efficient and effective service.
Healthcare professionals delivering health services need to be engaged from frontline delivery to the very centre of policy decision making.
Purpose and Function of the Health & Social Care (Reform) Bill
The purpose of the Bill will be to provide the legislative framework within which the proposed new health and social care structures can operate. It seeks to set out, as transparently as possible, the high level functions of the various health and social care bodies.
The Bill seeks, either within the body of the Bill or by securing sufficient powers to make subordinate legislation, to establish the parameters within which each health and social care body will be permitted to operate and to establish the necessary governance and accountability arrangements which will support the effective delivery of health and social care in Northern Ireland.
The Bill has 35 clauses and 7 Schedules[7]. It comprises 10 headings:
1. Restructuring of administration of health and social care – covers the restructuring of health and social care bodies;
2. Department’s role in promoting and providing health and social care – consists of 5 clauses and outlines the general duties, powers and priorities of the Department of Health, Social Services and Public Safety (“the Department”);
3. The Regional Board - consists of 5 clauses and provides for the establishment of the Regional Health and Social Care Board. It also covers the functions of the Regional Board and outlines its objectives;
4. RAPHSW - consists of 2 clauses and provides for the establishment of the Regional Agency for Public Health and Social Well-being;
5. RSSO - consists of 2 clauses and provides for the establishment of the Regional Support Services Organisation;
6. Patient representation and public involvement – establishes the Patient and Client Council, covers the functions of the Patient and Client Council and deals with the need for health and social care bodies to consult with service users and produce consultation schemes.
7. HSC trusts – places a duty on HSC trusts in relation to the improvement of health and social well-being;
8. Public-private partnerships – provides for the Department of Health, Social Services and Public Safety, the Regional Health and Social Care Board, the Health and Social Care trusts, the RSSO, special agencies and the RAPHSW to form, or participate in forming, public-private partnerships;
9. Transfer of assets, liabilities and functions - deals with the dissolution of various health and social care bodies and the transfer of assets, liabilities and functions;
10. Supplementary – provides for the Department to make supplementary provisions as it thinks necessary and makes general provisions in respect of subordinate legislation, amendments and repeals. It also sets out the title and commencement dates and includes interpretation provisions.
The Health & Social Care (Reform) Bill Proposals
1. The BMA(NI) welcomes the Bill as the progression of Phase 2 of the Review of Public Administration (RPA) in health as it has the potential to improve the lives of many people in Northern Ireland via a more efficient and less bureaucratic healthcare system, by the consequent release of resources to frontline patient care.
2. Restructuring of administration of health and social care
(Clause 1) The BMA(NI) understands the dissolution of current structures are to facilitate the creation of the new ones. However any restructuring must not impact on frontline budgets. The BMA(NI) supports the slimming down of the Department of Health Social Services and Public Safety Northern Ireland (DHSSPSNI) and looks forward to savings from a reduction in bureaucracy being released to frontline patient care. It is essential that such savings are audited and that the Department communicates with HSC organisations and stakeholders on how these savings will be redistributed to frontline patient care. This must be a transparent process.
3. Department’s role in promoting and providing health and social care –
(Clause 2) The BMA(NI) agrees with the Department’s general duties and hopes that the leadership of the medical profession will be closely involved at this level.
(Clause 3) The BMA(NI) notes that commissioning will play a very important role and that commissioning should be led from the local community upwards. There is a concern amongst medical professionals that commissioning will be implemented in a top down approach, when it should be a bottom up approach in order to reflect local needs.
(Clause 4, 5 & 6) The BMA(NI) welcomes the Department putting consultation at the core of its priorities and objectives. However, this must be meaningful consultation and not just going through the motions on a decision that has already been taken. The BMA(NI) would also like to see all ‘emergency’ decisions by the department subject to some form of retrospective consultation.
4. The Regional Board –
(Clause 7) The BMA(NI) welcomes the dissolution the four Health and Social Care Boards to create one Regional Health and Social Care Board in their place. The reduction of the number of Boards has been a long standing BMA(NI) policy objective. However, there are still some concerns about how each section or department will communicate with each other in such a large organisation.
(Clause 8) The BMA(NI) welcomes the emphasis on the responsibility of the Regional Health and Social Care Board (RHSCB) for managing the performance of HSC Trusts, commissioning, and how resources are best used as set out. The BMA(NI) would contend that the RHSCB should look to how the process of commissioning, within the commissioning plan, can best be accomplished from the bottom up with the inclusion of locality based commissioning.
(Clause 9) The BMA(NI) welcomes the creation of Local Commissioning Groups which will contain healthcare professionals. There is little given to the actual membership of the Local Commissioning Groups in this Bill and the BMA(NI) disagrees with the proposal that commissioning should be a ‘democratic’ process, as proposed by the Minister in his speech to the Chamber on 4th February 2008. Healthcare commissioning is about assessing need, and prioritising and commissioning according to need, not democracy. The BMA(NI) continues to be concerned about the proposal that local councillors should be included in the commissioning process. There is firm agreement that accountability must be part of the reform, however the BMA(NI) believes there is a difference in operation between organisational accountability and democratic accountability. The BMA(NI) believes that the consultation process on either the Board or the Department giving directions or revision of priorities or objectives with regard to the commissioning of healthcare must include the Local Commissioning Groups. Again the BMA(NI) would raise the issue of the need for a bottom-up approach to commissioning rather than top-down.
(Clause 10) The BMA(NI) believes that before the RHSCB gives any direction of a general or specific nature it must engage with the Local Negotiating Committee[8] to ensure such directions can legally and practically be implemented.
(Clause 11) The BMA(NI) believes that the reporting structures, while essential to the process of improving services, should be, at the direction of the RHSCB, consistent across Northern Ireland and should not reduce the time hospital doctors have to treat patients. It must be pointed out that hospital doctors may not have their protected time within direct clinical care or may have their time for professional development interfered with. An increase in medical secretarial staff would help facilitate the smooth running of information gathering.
5. RAPHSW -
(Clauses 12 & 13) The BMA(NI) welcomes the creation of a single Regional Agency for Public Health and Social Well being and the emphasis on public health and social well being. The BMA(NI) believes that this is in keeping with the health service working with wider society to promote a holistic approach to maintaining a healthy lifestyle. The BMA(NI) also believes that the public health function should be led by a Director of Public Health and that there should be no split of the public health profession nor should public health doctors be employed by more than one body. The division of responsibilities between RHSCB and RPHA adds an unnecessary layer of complication to the Public Health function. If the RPHA is set up it will be essential that its Director of Public Health is also on the Board of the new RHSCB. Regarding the Regional Public Health Agency (RPHA) the BMA(NI) views are as follows:
- The priority given to public health in the new structures is welcomed
- It is assumed that the role/functions of public health doctors will be enhanced and that public health doctors are backed up by the necessary staffing levels and support
- The RPHA will need to interface significantly with the Department, the RHSCB, the CSO and Trusts. It is essential that bureaucracy is minimised within the RPHA and between such organisations
- There should be no clash between the Director of Public Health and the Chief Medical Officer. There must be clarity about the relationship of the advisory roles of the Director of Public Health and the Chief Medical Officer to the Minister.
6. RSSO –
(Clauses 14 & 15) The BMA(NI) cautiously welcomes the creation of the Regional Support Services Organisation (RSSO), which seems to follow the general trend of Executive Departments as a whole to centralise particular support functions. Whilst this is something that can be welcomed in order to reduce unnecessary duplication of particular services, the BMA(NI) is concerned about the size and potential bureaucracy of such a large organisation, particularly against the backdrop of the RPA which was initiated to reduce bureaucracy. The BMA(NI) would want to be assured that this large organisation would be structured in a flat or horizontal form.
The layers of hierarchy in the new Regional Support Services Organisation should be minimised and the various support functions managed as overall business units within the organisation. Without such a structured approach the BMA(NI) would be concerned that the new RSSO would be too hierarchical and too bureaucratic with far too many communication needs. The BMA(NI) would also be concerned that such a huge bureaucracy – as per other bureaucracies – could grow over time (to cope with needs regarding management, communication and internal support functions) and potentially undo much of the work that the RPA has done to eliminate unnecessary bureaucracy.
The BMA(NI) view is that one overly bureaucratic system should not be replaced with another, particularly given the cost of undertaking and implementing the RPA to date in terms of time, money, commitment and personal sacrifices, such as voluntary redundancy or voluntary early retirement.
7. Patient representation and public involvement –
(Clauses 16 to 20) The BMA(NI) believes that a single Patient and Client Council, with local offices, effectively staffed and resourced would be much more strategically effective and joined-up than five separate Patient Client Councils. The emphasis on inclusive consultation is welcome.
8. HSC trusts -
(Clause 21) The BMA(NI) welcomes the duty placed on the Health and Social Care Trusts to exercise their functions with the aim of improving the health and social well-being of those for whom it provides, or may provide, health and social care. Though maybe more clarity is required on how this is to be achieved and managed.
9. Public-private partnerships –
(Clause 22) The BMA(NI) is concerned with the issue of Public Private Partnerships (PPP). The BMA(NI) is opposed to the use of Private Finance Initiatives (PFI) in the NHS and would oppose any use of this clause to pursue the use of PFI within the health service. However, it must also be noted that Clause 22 is very vague in what is referred to as public private partnerships. This clause requires further clarification on its actual intended purpose.
10. Transfer of assets, liabilities and functions –
(Clauses 23 to 28) The BMA(NI) believes that the process of dissolution and transfer should be properly planned with open communication with the staff involved to ensure a smooth implementation.
The BMA(NI) is concerned about the transfer of the Mental Health Commission to the Health and Social Care Regulation and Quality Improvement Authority. This concern is purely on the issue of staffing and training. The functions of both organisations, within the new amalgamated context, must be properly resourced and not be allowed to deteriorate.
11. Supplementary –
It is important that the scrutiny and power of the Legislative Assembly is maintained through out this process. The BMA(NI) looks forward to the subordinate legislation receive due scrutiny before they are enacted.
[1] OFMDFM press release, Preparations for the Review of Public Administration, 12 February 2002, http://archive.nics.gov.uk/ofmdfm/020212e-ofmdfm.htm (accessed on 23 September 2008)
[2] Review of Public Administration (2003), The Review of Public Administration consultation, http://www.rpani.gov.uk/consult2003_doc.pdf (Accessed on 23 September 2008)
[3] Review of Public Administration (2005), The Review of Public Administration further consultation, http://www.rpani.gov.uk/2005_consultation_doc.pdf (Accessed on 23 September 2008)
[4] The response to the 2003 consultation can be accessed at http://www.rpani.gov.uk/british_medical_association_northern_ireland-2.pdf and the response to the 2005 consultation can be accessed at http://www.rpani.gov.uk/british_medical_association_(ni).pdf
[5] The BMA(NI) response can be found at http://www.dhsspsni.gov.uk/51a-british_medical_association_bma_ni.pdf
[6] DHSSPS (2008), Proposals for Health and Social Care Reform, http://www.dhsspsni.gov.uk/consultation_package.pdf
[7] This can all be found in the Health & Social Care (Reform) Bill Explanatory and Financial Memorandum at http://archive.niassembly.gov.uk/legislation/primary/2007/niabill21_07efm.htm (Accessed on 23 September 2008)
[8] In 1991 when Health Trusts were established, the BMA formed Local Negotiating Committees (LNCs) within Health Trusts. LNCs consist of local representatives of doctors (and dentists), employed by the Trust, who meet regularly to identify issues for negotiation with local management and agree their objectives. They will meet with management representatives in the Joint Negotiating Committee in order to conclude and monitor the application of local agreements and agree and monitor arrangements for the implementation of national agreements within the organisation.
The LNC will also usually nominate BMA representatives for other joint committees (e.g. Joint Consultative Committee, Health and Safety Committee) and work with other trade unions in areas of common interest within the organisation.
LNC membership includes Consultants, Staff and Associate Specialist doctors, Doctors in training, Salaried GPs, Dental staff representatives, Medical Academics, Public Health doctors and Community Health doctors. A BMA Industrial Relations Officer will also be a member of the Committee.
Members of the Committee who are BMA members will be accredited as local representatives by the Association (see below)The Committee will appoint a chairman and vice-chairman and may appoint a secretary. These appointments should also be for a fixed (renewable) period of not more than two years. An LNC meets regularly and engages with management at least every two or three months.
Provided that the majority of members are BMA members and the constitution complies with the above guidance, the BMA will accredit the LNC as a representative Committee. That will ensure the entitlement to the benefits of being a recognised trade union set out in the legislation and any national and local agreements. It will also ensure that the Committee receives support from the BMA.
The BMA provides training and information for chairmen and members of accredited LNCs and will establish an LNC forum in each Region and devolved nation. LNCs will nominate a representative (normally the chairman) to the forum which will provide a focus for the exchange of information and development of a consistent approach to issues where this is important. BMA Regional Services staff also maintain a database of local agreements.
Letter from the BMA
23 October 2008
BMA(NI) evidence to the Health Committee on 2nd October 2008
The BMA(NI) would like to thank the Committee for allowing us to provide our evidence on 2nd October 2008 on the proposed Health and Social Care (Reform) Bill. The level of discussion was of a very high standard and we are glad the members of the Committee were able to take on board what we were saying and we appreciated the chance to discuss difficult reform issues with the Committee.
We were, however, deeply disappointed by the comment referring to doctors as only working their hours and afterwards play golf or go sailing. This is an unjust and unfair generalisation that does nothing to recognise the contribution the medical profession makes to society every day by working in, living in, and actively contributing to their local communities. We were also disappointed that our opinions on LCGs were viewed in a way that our presentation was ‘damned by its inclusion’. While we recognise and take on board the views of the members of the committee, we felt this was an unhelpful comment.
We hope the members will genuinely consider our thoughts on the issue of LCG membership. We have always supported the Power of Wellbeing and community planning role of local councils and are fully in support of a genuine partnership approach.
It may also be worth reiterating that LCGs are a linchpin in what should be effective commissioning and that the BMA(NI), along with other health related organisations, want to see strong commissioning powers and budgetary control at this level. There also needs to be structures for commissioning below LCG level to effect real local commissioning.
We look forward to continuing to work with the Committee and its members to ensure the healthcare system in Northern Ireland provides the best health outcomes.
Briefing Paper from RQIA
The Regulation and Quality Improvement Authority (RQIA)
1. Introduction
1.1 The Regulation and Quality Improvement Authority (RQIA) welcomes the introduction of the Health and Social Care (Reform) Bill which will give increased clarity to health and social care structures in Northern Ireland and an increased focus on the improvement agenda championed by the RQIA.
1.2 The RQIA strongly supports the ‘Transfer of functions of the Mental Health Commission (MHC)’ contained in Clause 25 of the Bill, and believes that there is a clear rationale for this change. Since the initial proposals under the Review of Public Administration, the RQIA has worked closely with the MHC to develop plans to ensure that a seamless transfer of functions takes place within agreed timescales.
1.3 The transfer offers a unique developmental opportunity to take account of the recommendations contained in the Bamford Review of Mental Health and Learning Disability, and the benefits of the combined strengths of both organisations and the legislation under which they operate (The Mental Health (NI) Order 1986 and The Health and Personal Social Services (Quality, Improvement and Regulation) (NI) Order 2003).
2. Strategic Alignment
2.1 The RQIA has established a Project Board with membership from both the RQIA and the MHC to oversee the transfer. The work of the Project Board includes, to:
a) approve a due diligence action plan;
b) clarify the legal implications of the transfer;
c) clarify the implications for the RQIA Board;
d) decide on the workforce and financial alignment;
e) prepare the operational alignment of the activities of the MHC;
f) develop an appropriate communications plan.
2.2 An important part of the Project Board’s work has been the development of a comprehensive delivery model of how the RQIA will carry out its new responsibilities in respect of mental health and learning disability services This model has been developed in consultation and partnership with Mental Health Commissioners. It identifies and highlights the specific and unique functions, ethos and focus of the MHC and proposes how these features can be retained and further developed following the transfer. This model has been subject to review by the MHC and leading professionals in the fields of psychiatry and learning disability.
2.3 The RQIA is in the process of establishing a dedicated Mental Health and Learning Disability Programme Team as a separate and distinct entity to take forward this important work within the RQIA.
2.4 The revised organisational structure will provide an opportunity to ensure that all review and inspection activity focuses on:
- the specific care and treatment and human rights of individuals under The Mental Health (NI) Order 1986;
- engagement and consultation with the wider service user group, their carers and advocates;
- the context and environment within which care is provided;
- an assessment of the quality and availability of care using quality standards, clinical and care guidelines and legislative regulations;
- taking relevant enforcement action against non-compliance with regulations and failures in service quality and safety.
2.5 The RQIA is committed to protect and promote the core functions of the MHC as enshrined in legislation. This includes a commitment to maintain the spirit of the MHC’s views of The Mental Health (NI) Order 1986 and complements the RQIA principles of:
- independence
- multidisciplinary working
- investigative action
- inspectorial action
- advisory work
- protection of patients and public
3. A new way forward
3.1 The combined powers and functions of the RQIA following the transfer will reflect a number of the aspirations cited within submissions to the Bamford Review, including:
- retention and further development of a focus on the individual and the rights of service users and carers under the current functions of the MHC, whilst incorporating the powers of enforcement and improvement on organisations under The Health and Personal Social Services (Quality, Improvement and Regulation)(NI) Order 2003;
- promotion of multi-professional and lay working in a manner not currently available to the MHC through the RQIA’s programme of inspection, governance and service reviews;
- placing of an additional emphasis on the promotion and sharing of good practice across mental health and learning disability services;
- creation of an opportunity for wider promotion of mental health, advocacy, service user and carer engagement.
3.2 The ‘person centered’ approach adopted is designed to:
- respect every person’s human rights and their right to timely high quality care;
- promote choice;
- listen to the needs of individual service users and the views of carers;
- develop a culture of learning and innovation;
- challenge practice where deficiencies are evident or where a need for change is demonstrated;
- work with integrity in a transparent and open way.
3.3 The RQIA will aim to be more accessible, responsive and targeted in how it monitors the quality of health and social care by engaging more effectively in public participation. (The RQIA has developed a Public Participation Strategy which is currently out to consultation.) It is also committed to further developing lay participation in informing, planning, implementing and evaluating the MHC functions within the RQIA.
3.4 External reference groups will be established that will include service users, carers and advocates representing the respective interests of Mental Health and Learning Disability.
4. Operational Alignment
4.1 The RQIA views the transfer as an opportunity to build upon its existing resources, with the addition of an expert specialist team of full-time and paid sessional, multi-professional officers with appropriate, experience, skills and knowledge to discharge these functions.
4.2 The specific responsibilities for mental health and learning disability issues will be incorporated into the wider mental health and learning disability review team. This team will be further augmented with a range of lay reviewers.
4.3 As recommended by the Bamford Review, the RQIA visiting programme will include annual announced and unannounced reviews and inspections of mental health and learning disability hospital facilities in Northern Ireland. The RQIA will move to a mixed methodological approach to ensure that the needs and rights of individuals are met through its visiting, review and inspection programmes.
4.4 The RQIA will also establish arrangements to monitor and review all cases involving Guardianship in Northern Ireland. It will continue to maintain close scrutiny of all circumstances of instances of ill-treatment, deficiency in care, maltreatment, improper detention in hospital or reception into guardianship of any patient. To ensure that full account is taken of the human rights and equality implications of The Mental Health (NI) Order 1986, the RQIA will recruit a human rights advisor.
4.5 The RQIA will employ a sessional medical panel drawn from practising and recently retired psychiatrists who will, as required, accompany and support Mental Health Order officers. The RQIA will endeavour to facilitate the recruitment of existing medical panel members of the MHC to provide continuity into the future.
4.6 The RQIA will establish a multidisciplinary panel for the review of all treatment plans to include ECT, pharmacological, and psychological. therapies. This multidisciplinary panel would be drawn from staff employed by the RQIA.
5. Governance
5.1 The RQIA will continue to foster a strong working relationship with the DHSSPS. A revised code of practice will be developed in line with the agreed functional model and the proposals contained in the relevant Bamford reports
5.2 Functions arising out of The Mental Health (NI) Order 1986 will be subject to performance management and scrutiny by the Executive Management Team of the RQIA. This will be further reflected to the RQIA Board at all Board meetings, in quarterly performance management reports and within the RQIA’s Annual Report and Accounts.
Allied Health Professions
Briefing for Health, Social Services and Public Safety Committee
October 2008
Background & Introduction
The AHP Federation NI represents over 6000 professional and technical health care staff working in Northern Ireland. Allied health professionals (AHPs) work with all age groups and across all programmes of care. Their particular skills and expertise play a central role in health and social care and will be essential in delivering the Department’s modernisation and reform agenda. AHPs fully understand and support the need to modernise and reform health and social care structures to ensure that patients receive the right care, at the right time, in the right location. AHPs focus on a holistic, person centred approach to health and well being, and this means that they are ideally placed to lead on service development and deliver better, more cost effective outcomes for service users. The purpose of this briefing is to demonstrate the unified, collective views of allied health professionals on the changes currently under consideration and the impact that AHPs can make to service modernisation.
Restructuring of the Administration of Health & Social Care
Organisational structure directly influences the provision of patient care, affecting staffing and service delivery. It affects how services are delivered across boundaries and impacts on how resources are directed to front-line services. The management structures at Departmental, Regional Board, Trust and Commissioning level must reflect adequate representation for AHPs to ensure that health care professionals involved in the planning and delivery of services can play a more inclusive role in developing effective integrated health and social care services for patients.
It is our view that many of the concerns regarding the impact of the current organisational changes on AHP services have been overlooked. The requirement for effective and efficient management of AHP services is of paramount importance for patient care. Better more supportive structures for AHPs will provide significant opportunies to develop more innovative and creative ways to address long-established problems. They will facilitate better partnerships with professional colleagues in overcoming real and perceived boundaries between services and organisations, and will help develop ways of working which will benefit service users.
At Departmental Level
We welcome the general duties, priorities and objectives outlined for the Department in the legislation. We welcome the emphasis placed on the Department for setting policy and strategy across the health service. We are concerned however, with the current arrangements at the Department for AHPs and the absence of an adequate support structure for our professions. We need to ensure that there is an AHP structure at strategic level within the Department, staffed by those who have the necessary experience and expertise to appropriately advise on the planning and delivery of services.
We are further concerned by the conclusions in Top Structures Review report, which was carried out by the Department in 2006, that “the current top management and processes within the Department are not adequate to meet the challenges ahead” and that, “the policy development process itself was flawed because of the silo based approach within the Department, with each area developing its own agenda in isolation from the wider strategic intent” (DHSSPSNI, Top Structures Review, August 2006). It is crucially important therefore, that there is an appropriate structure at Departmental level to ensure the development of policy and professional standards, effective professional governance frameworks and support for the regulation of the AHP professions. We look forward to the outcome of the review of the Department’s structure, role, functions and staffing in the expectation that it will address these issues.
At Regional Board, RAPHSW & Trust level
AHPs support the proposals to establish a new Regional Health and Social Care Board. There is considerable benefit in the establishment of a single regional strategic planning authority. We would reinforce the point made previously in relation to the Department that adequate structures are required at a strategic level at the Board to ensure that there is appropriate professional advice and support available for AHPs and other HPSS agencies.
With regard to Health and Social Care Trusts each of the HSC Trusts has a key responsibility to develop community initiatives to reduce inequalities and enhance the health of the local population. Many are already developing robust engagement strategies and have brought together the health promotion teams from the legacy Trusts. Having the support of the Regional Agency for Public Health and Social Wellbeing (RAPHSW) will be crucial for the work of the HSC Trusts and will enable the sharing of best practice across the HPSS. Local government has a key role to play in the delivery of health messages to the public. It has local knowledge of the health and social issues facing its constituents and should be more involved in delivering health care messages to its public.
AHPs support the proposal that local government should consult more explicitly with RAPHSW to ensure that the wider public health agenda is communicated effectively at a local level. AHPs are already working with members of local government - e.g. environmental health officers, sports development officers as well as Leisure Services, Housing and Education to promote key healthy lifestyle messages around activity and diet. The Regional Health & Social Care Board and its Local Commissioning Groups would be required, through legislation, to seek advice from the RAPHSW when developing their commissioning plans. We support the above proposal, as it will mean that commissioning will be targeted to reduce the health costs of the population in the long term whilst providing the necessary health interventions in the short term. RAPHSW can act as a conduit for best practice and signpost RHSCB and the LCGs to other good practice examples.
The Committee should note however, that under the label of reorganisation brought about by the RPA, the roles and career prospects of a high number of very experienced and valuable AHP colleagues have been cut in order to make further savings. Senior posts with both clinical and management responsibilities have been identified as RPA impacted. Not only does this contradict the commitment given at the start of the RPA process, that frontline staff would not be affected by RPA, but will have a detrimental impact on the ability of services to achieve the improvements in the quality and efficacy for services to patients.
Commissioning/LCGs
The AHP Federation supports the broad concept of commissioning as the means by which we can secure the best possible health and wellbeing outcomes, and health and social care provision for service users. AHPs support the establishment of five Local Commissioning Groups (LCG’s) coterminous with the exiting five Health and Social Care Trusts. This will provide a more responsive local mechanism for commissioning patient services. The new arrangements should promote an inclusive approach to the development of regional objectives with a view to the staff tasked with delivering frontline services having real ownership in implementing those objectives. The new system and structures, above all else, must be accountable to the population they serve and have open, inclusive, and transparent processes, which are readily accessible to public and staff alike. It is essential that the new structures ensure that the needs of service users have appropriate forums for planning and commissioning. Previous structures failed to sufficiently engage the full range of professionals in the planning and commissioning of services to meet the needs of users requiring therapeutic interventions.
We welcome the intention to ensure the promotion of health and wellbeing as central to commissioning. It is essential that greater emphasis is placed on prevention and health improvements. This is an area where AHP’s skills have been significantly under utilised in the past. Social inclusion is a fundamental tenet of well-being and AHPs already have the skills and knowledge to engage and lead community group activities to promote inclusion. This has recognised benefits for the demand on health services. By working closely with service users, AHPs act as key ‘sign posters’ and are able to conceptualise the whole journey for the patient. AHPs can advocate for service users, bring a solution focus to individual patient need rather than just a clinical diagnosis, enabling patients to make informed choices and helping them to understand and balance the risks within the decision making process. Due to this empowering relationship with service users, AHPs are able to educate and support service users to develop and sustain new positive health behaviours much more effectively.
Regarding the commissioning process itself, further clarification regarding the mechanisms and extent of financial control to be devolved to Local Commissioning Groups is required. Care needs to be taken to ensure that there is minimum duplication in the commissioning roles of the Board and the Local Commissioning Groups (LCGs).There needs to be clear direction on what is commissioned regionally and locally with as much commissioning as possible done at a local LCG level.
Adequate resources and financial controls should be devolved to these groups to ensure that commissioning is effective. This will require a high level of professional support, including input from public health, social services, nursing, allied health professionals, planning, finance and information.
Patient Representation & Public Involvement/RQIA
Public and patient involvement is a key element in improving health and social care in Northern Ireland. Involving the public and patients is central to service planning and provision; it is a major driver for service improvement and leads to a better patient experience of care. The reforms under consideration must involve individuals and communities in the design, delivery and monitoring of health services. AHPs strongly support the establishment of single Patient and Client Council with five local offices operating in the same geographical areas as the existing Trusts. This will provide a strong voice for patients and carers and will ensure strong local influence. This arrangement will best present the strongest method of challenge to the health and social care system. Strong links with the RAPHSW and LCGs will need to be developed to ensure effective user engagement. A Patient and Client Council with five local offices will be better placed to promote and represent the public interest. Structures in the Trusts are very individual and we therefore take the view that it is more important in this instance that there are strong local bodies to engage with service providers and articulate the public voice and carry out the functions of the new organisations.
AHPs welcome the intention to dissolve the Mental Health Commission and transfer its functions to the Regulation and Quality Improvement Authority. RQIA is the independent body responsible for monitoring and inspecting the availability and quality of health and social care services in Northern Ireland, and encouraging improvements in the quality of those services. Patients need to feel that the quality of care they are receiving is consistent regardless of where they live. AHPs are concerned however, that the current arrangements within the RQIA do not allow for the full participation of allied health professionals in relation to the monitoring and regulation of the quality of health and social care services provided in Northern Ireland. It is our view that the RQIA needs to make provision for the involvement of AHPs in each and every initiative designed to produce faster, more efficient high quality services to ensure the very highest standards of patient care.
Appendix 5
List of Witnesses
Dr Andrew McCormick Permanent Secretary, DHSSPS
Dr Michael McBride Chief Medical Officer, DHSSPS
Dr Miriam McCarthy Deputy Secretary Health Care Policy, DHSSPS
Mr Bernard Mitchell Modernisation Directorate, DHSSPS
Mr David Bingham Director Human Resources, DHSSPS
Dr Brian Gaffney Chief Executive, Health Promotion Agency
Dr Jane Wilde Chief Executive, Institute for Public Health
Ms Claire Higgins Public Health development Officer, Institute for Public Health
Ms Heather Moorhead Chief Executive, NILGA
Mr Arnold Hatch President, NILGA
Mr Paul McBrearty Chief Executive, Mental Health Commission
Mr Noel McKenna Chairperson, Mental Health Commission
Ms Clare Quigley Social Work Member of the Commission
Dr Brian Fleming Consultant Psychiatrist and Medical Member of the Commission
Mr Ivan McMaster Modernisation Unit, DHSSPS
Mr Craig Allen Modernisation Unit, DHSSPS
Mr Stephen Hodkinson Chief Executive, Central Services Agency.
Ms Jacqueline Kennedy Director of Human Resources and Corporate Services, Central Services Agency.
Ms Paula Sheils Director of Family Practitioner Services, Central Services Agency.
Prof Dominic Burke Acting Chief Executive, Western Health & Social Services Board
Dr Paula Kilbane Chief Executive, Eastern Health & Social Services Board
Mr Stuart MacDonnell Chief Executive, Northern Health & Social Services Board
Ms Fionnuala McAndrew Director of Social Services, Southern Health & Social Services Board
Mr Richard Dixon Chief Officer, Eastern Health & Social Services Council
Ms Alice Casey Interim Chief Executive, Regulation & Quality Improvement Authority
Mr Phelim Quinn, Director of Operations, Regulation & Quality Improvement Authority
Mr Jude O’Neill Head of Mental Health and Learning Disability, Regulation & Quality Improvement Authority
Ms Mary Hinds Director, Royal College of Nursing Northern Ireland
Ms Ann Marie O’Neill Chair, Royal College of Nursing Northern Ireland Board.
Dr Brian Patterson British Medical Association (NI), Chairman of Northern Ireland Council
Dr Brian Dunn British Medical Association (NI), Chairman of the General Practitioners Committee
Mr Danny Lambe British Medical Association (NI), Deputy Secretary
Mr Ivor Whitten British Medical Association (NI), Assembly & Research Officer
Mrs Liz Cavan Committee Member, Allied Health Professions Federation UK
Ms Liz McKnight Chair, Allied Health Professions Federation NI.
Mr Tom Sullivan Policy Officer, Chartered Society of Physiotherapy NI.
Dr Carolyn Harper Department of Health, Social Services & Public Safety
Mr Martin Bradley Chief Nursing Officer, DHSSPS



